0% found this document useful (0 votes)
21 views14 pagesBacterial Infection..
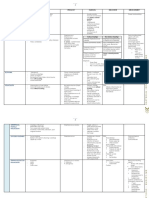
The document provides an overview of various bacterial infections, including impetigo, erysipelas, folliculitis, and furuncle, detailing their classification, clinical features, treatment options, and causative organisms. Impetigo is a common superficial infection in children, while erysipelas is characterized by marked lymphatic involvement and requires specific antibiotic treatment. Folliculitis and furuncle are infections of hair follicles, with furuncle presenting as a deeper abscess, often treated with antibiotics and drainage.
Uploaded by
Chakshu KalraCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
21 views14 pagesBacterial Infection..
The document provides an overview of various bacterial infections, including impetigo, erysipelas, folliculitis, and furuncle, detailing their classification, clinical features, treatment options, and causative organisms. Impetigo is a common superficial infection in children, while erysipelas is characterized by marked lymphatic involvement and requires specific antibiotic treatment. Folliculitis and furuncle are infections of hair follicles, with furuncle presenting as a deeper abscess, often treated with antibiotics and drainage.
Uploaded by
Chakshu KalraCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd