0% found this document useful (0 votes)
41 views89 pagesECG For Residents
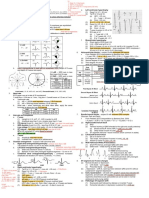
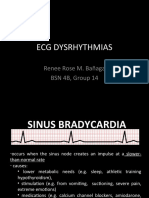
The document provides a comprehensive overview of ECG principles, including electrode placement, waveforms, and diagnostic criteria for various cardiac conditions. It covers abnormalities such as chamber enlargement, hypertrophy, and myocardial ischemia, along with exercises for interpreting ECGs in clinical scenarios. The content is structured for residents in cardiology, emphasizing the importance of systematic reading and analysis of ECGs.
Uploaded by
bibekrnr500Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
41 views89 pagesECG For Residents
The document provides a comprehensive overview of ECG principles, including electrode placement, waveforms, and diagnostic criteria for various cardiac conditions. It covers abnormalities such as chamber enlargement, hypertrophy, and myocardial ischemia, along with exercises for interpreting ECGs in clinical scenarios. The content is structured for residents in cardiology, emphasizing the importance of systematic reading and analysis of ECGs.
Uploaded by
bibekrnr500Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd