0% found this document useful (0 votes)
11 views34 pagesFamily Planning
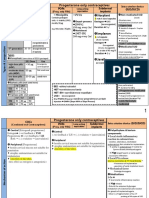
The document provides an overview of various family planning methods, including combined oral contraceptives, emergency contraceptive pills, progestin injectables, implants, and intrauterine devices (IUDs). It details how each method works, their side effects, and benefits, such as protection against pregnancy and certain cancers. Additionally, it discusses the effectiveness of different contraceptive methods and guidelines for their use.
Uploaded by
Joshua SinghCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
11 views34 pagesFamily Planning
The document provides an overview of various family planning methods, including combined oral contraceptives, emergency contraceptive pills, progestin injectables, implants, and intrauterine devices (IUDs). It details how each method works, their side effects, and benefits, such as protection against pregnancy and certain cancers. Additionally, it discusses the effectiveness of different contraceptive methods and guidelines for their use.
Uploaded by
Joshua SinghCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd