Professional Documents
Culture Documents
Autonomic Dysreflexia
Uploaded by
EOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Autonomic Dysreflexia
Uploaded by
ECopyright:
Available Formats
1
Elisabeth Fandrich
10/08/08
524 K,C,T
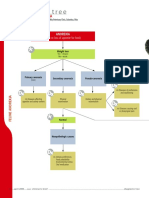
Autonomic Dysreflexia
Autonomic dysreflexia is a condition that is potentially life-threatening. The
autonomic nervous system overreacts to excessive stimulation of the nerves below
the level of the spinal cord injury. Normally, when the autonomic nervous system
response is activated, the mediating parasympathetic nervous system response is
triggered. In the case of the patient with a spinal cord injury, the parasympathetic
nervous system response is blocked at the site of the injury.
Severe hypertension occurs as a result of the vasoconstriction elicited by the
autonomic nervous system response. This severe hypertension can lead to seizures
or even a stroke if it is not controlled and reversed as soon as possible.
The body itself will try to counteract the hypertensive state by vasodilation. This
will only occur above the location of the spinal cord injury. The result of this is that
the lower body has a blood pressure that is very high, and the upper body has a
lower blood pressure. The vagus nerve is stimulated by the high blood pressure
which triggers bradycardia. Rather than stimulating vasodilation like it normally
would, the signal never reaches the vessels lower than the site of the injury.
Autonomic dysreflexia can be triggered by any strong nerve stimuli below the site of
injury, but the most common causes are as follows: bladder distention, constipation,
renal calculi, ejaculation, uterine contractions, skin rash, pressure sores,
thrombophlebitis, enemas, exposure to hot/cold stimuli, gastric ulcers,or
menstruation.
When a patient exhibits signs of autonomic dysreflexia, a quick assessment must be
done, catheters must be inspected for kinks, bladder distention, constipation, etc.
The stimulus that has triggered the autonomic dysreflexia must be discontinued
immediately.
Manifestations of autonomic dysreflexia are paroxysmal hypertension (no known
reason), pounding headache, blurred vision, bradycardia, diaphoretic above site of
spinal cord injury, piloerection, nasal congestion, nausea, and papillary dilation.
Treatment for autonomic dysreflexia is to remove the causative stimulus, and
administer medications to lower blood pressure.
2
524, K, C, T is a 45 year old man who has a longstanding history of paraplegia (the
result of a motorcycle accident as a teenager). He was in the transitional care unit
(TCU) for the treatment of a leg ulceration (MRSA and cellulitis) . Over the course of
the day, he reported back pain with increased muscle spasms. His blood pressure
increased, IV labetalol was administered with initial improvement then overall
worsening of symptoms. His suprapubic catheter was flushed and found to have
been kinked. The catheter was replaced and had good urine output. His blood
pressure did not improve. He became tachycardic and diaphoretic. He was
transferred to the ICU where his condition was stabilized then transferred to the
acute care floor.
Lab values were overall normal with the exceptions of decreased RBC (4.49 chronic
infection), decreased Hgb (12.1 may be false low caused by antibiotics), increased
RDW (18.4 may be result of dietary insufficiencies), A:G ratio decreased (0.7
prolonged immobilization), increased C-Reactive Protein (1.8 chronic infection).
His blood pressure was still higher than normal at 0800 on 10/08/08 (178/62), but
he was otherwise asymptomatic. Additional hypertension medications were
prescribed in an attempt to prevent another episode of autonomic dysreflexia.
References:
Introduction to Medical-Surgical Nursing
Linton
Diseases and Disorders: A Nursing Therapeutics Manual
Marilyn Sawyer Sommers
Susan A. Johnson
Theresa A. Beery
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- MCU 2019 Human Diseases 5th EditionDocument626 pagesMCU 2019 Human Diseases 5th EditionMoon Edits100% (1)
- Zosyn (Piperacillin/tazobactram)Document2 pagesZosyn (Piperacillin/tazobactram)E67% (3)
- Geodon (Ziprasidone)Document2 pagesGeodon (Ziprasidone)ENo ratings yet
- Lamictal (Lamotrigine)Document1 pageLamictal (Lamotrigine)E100% (1)
- MCQs and Viva in Public Health Dentistry PDFDocument235 pagesMCQs and Viva in Public Health Dentistry PDFRitika90% (10)
- Pyelonephritis 1 Running Head: PYELONEPHRITISDocument4 pagesPyelonephritis 1 Running Head: PYELONEPHRITISENo ratings yet
- Pneumonia Short PathoDocument2 pagesPneumonia Short PathoENo ratings yet
- Influenza B PathoDocument4 pagesInfluenza B PathoENo ratings yet
- Hyponatremic Dehydration PathoDocument4 pagesHyponatremic Dehydration PathoENo ratings yet
- Iron Deficiency Anemia PathoDocument6 pagesIron Deficiency Anemia PathoENo ratings yet
- Clinical Medications Worksheets: (Why Med Ordered) Contraindications/warnings/interactionsDocument1 pageClinical Medications Worksheets: (Why Med Ordered) Contraindications/warnings/interactionsENo ratings yet
- Acute Pancreatitis PathoDocument5 pagesAcute Pancreatitis PathoENo ratings yet
- Hyperparathyroidism PathoDocument2 pagesHyperparathyroidism PathoENo ratings yet
- Congestive Heart FailureDocument4 pagesCongestive Heart FailureENo ratings yet
- Congestive Heart Failure-ABDocument3 pagesCongestive Heart Failure-ABENo ratings yet
- Theragran (Multiple Vitamins)Document3 pagesTheragran (Multiple Vitamins)ENo ratings yet
- Silvadene (Silver Sulfadiazine)Document1 pageSilvadene (Silver Sulfadiazine)ENo ratings yet
- Pancreatitis Short PathoDocument2 pagesPancreatitis Short PathoENo ratings yet
- Campral (Acamprosate Calcium)Document1 pageCampral (Acamprosate Calcium)E100% (1)
- Prozac (Fluoxetine) 40mgDocument1 pageProzac (Fluoxetine) 40mgENo ratings yet
- Buspar (Buspirone)Document1 pageBuspar (Buspirone)ENo ratings yet
- ZofranDocument1 pageZofranKatie McPeek0% (1)
- FiberCon (Polycarbophil)Document1 pageFiberCon (Polycarbophil)ENo ratings yet
- Lexapro (Escitalopram Oxalate)Document2 pagesLexapro (Escitalopram Oxalate)ENo ratings yet
- Florinef (Fludrocortisone)Document3 pagesFlorinef (Fludrocortisone)E100% (1)
- Synthroid (Levothyroxine)Document2 pagesSynthroid (Levothyroxine)E100% (2)
- Keppra (Levetiracetam)Document2 pagesKeppra (Levetiracetam)E100% (1)
- Zocor (Simvastatin)Document3 pagesZocor (Simvastatin)E100% (1)
- Neurontin (Gabapentin)Document1 pageNeurontin (Gabapentin)E100% (3)
- Ecotrin (ASA 81mg)Document3 pagesEcotrin (ASA 81mg)E100% (1)
- Solu-Cortef (Hydrocortisone)Document3 pagesSolu-Cortef (Hydrocortisone)E100% (2)
- Seroquel (Quetiapine)Document3 pagesSeroquel (Quetiapine)E100% (1)
- Kosongan Jadwal Ok Senen 30 Mei 2022Document4 pagesKosongan Jadwal Ok Senen 30 Mei 2022Arif KurniawanNo ratings yet
- LP UapDocument18 pagesLP UapHat MutisalNo ratings yet
- CHN 2Document12 pagesCHN 2Missy CookNo ratings yet
- Nursing Care Plan: Clustered Cues Nursing Diagnosis Rationale Outcome Criteria Nursing Interventions Rationale EvaluationDocument2 pagesNursing Care Plan: Clustered Cues Nursing Diagnosis Rationale Outcome Criteria Nursing Interventions Rationale EvaluationKarl Lourenz Deysolong100% (1)
- Diagnostic Tree: Feline AnorexiaDocument2 pagesDiagnostic Tree: Feline Anorexializ solanoNo ratings yet
- Gutierrez, Winell M. 5 NOVEMBER 2019 BSN Ii-3 Rle-Camantiles Rhu PoliomyelitisDocument6 pagesGutierrez, Winell M. 5 NOVEMBER 2019 BSN Ii-3 Rle-Camantiles Rhu PoliomyelitisWinell GutierrezNo ratings yet
- Simple EmergenciesDocument177 pagesSimple Emergenciesharsh89100% (1)
- Askep Diabetes MelitusDocument13 pagesAskep Diabetes MelitusfahrulNo ratings yet
- PsychiatryDocument19 pagesPsychiatryAnet Augustine AnetNo ratings yet
- Anthrax Background Information: Bacillus AnthracisDocument3 pagesAnthrax Background Information: Bacillus AnthracisDhea.MutiaraNo ratings yet
- Emergency PrepareDocument2 pagesEmergency Prepareapi-254322811No ratings yet
- ADC Part 1 - TG Keynotes II v1.0 PDFDocument17 pagesADC Part 1 - TG Keynotes II v1.0 PDFDrSaif Ullah KhanNo ratings yet
- Glue Ear / Secretory Otitis MediaDocument2 pagesGlue Ear / Secretory Otitis MediaBharat JoshiNo ratings yet
- Actinobacillosis: (Wooden Tongue)Document20 pagesActinobacillosis: (Wooden Tongue)Adeel SarfrazNo ratings yet
- Ards Quiz 20 ItemsDocument2 pagesArds Quiz 20 ItemsNicholas TagleNo ratings yet
- Comorbidity Psychiatric Disorders Posttraumatic StressDocument11 pagesComorbidity Psychiatric Disorders Posttraumatic StressReka Jakab-FarkasNo ratings yet
- South-East Asia Trend P-A M-1 L-12: Number of People Suffering From DM in SEA Region Is Also IncreasingDocument1 pageSouth-East Asia Trend P-A M-1 L-12: Number of People Suffering From DM in SEA Region Is Also IncreasingtanzirNo ratings yet
- Cerebrovascular DiseaseDocument2 pagesCerebrovascular Diseaseapi-3717941No ratings yet
- Sanjeevini CombinationsDocument22 pagesSanjeevini Combinationsikonoso100% (1)
- PAR-Q+: Oo Oo Oo OoDocument6 pagesPAR-Q+: Oo Oo Oo OoRoxyNo ratings yet
- Cudurrada CaruurtaDocument160 pagesCudurrada CaruurtaHilowle YareNo ratings yet
- Medical Symptoms Questionnaire v2Document2 pagesMedical Symptoms Questionnaire v2coolestgodgiftNo ratings yet
- Chir20001 Practical Assessment - Steven James ChangDocument7 pagesChir20001 Practical Assessment - Steven James Changapi-455408952No ratings yet
- 682 Saudi Arabia Fact SheetsDocument2 pages682 Saudi Arabia Fact SheetsMohammed GazoNo ratings yet
- 2+ Years: PECARN Pediatric Minor Head Injury CT Guidelines For Children AgeDocument2 pages2+ Years: PECARN Pediatric Minor Head Injury CT Guidelines For Children AgeIna AguilarNo ratings yet
- Cough and Dyspnea Case StudyDocument4 pagesCough and Dyspnea Case StudyAbigail Balbuena100% (1)
- Food Handler Teach and TestDocument2 pagesFood Handler Teach and TestSavitri Maharani BudimanNo ratings yet
- Classification of Mental DisordersDocument4 pagesClassification of Mental DisordersStuti Peter100% (1)