Professional Documents
Culture Documents
Vital Signs
Uploaded by
g44ngCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vital Signs
Uploaded by
g44ngCopyright:
Available Formats
Volume 3, Issue 3, 1999 ISSN 1329 - 187
BestPractice
Evidence Based Practice Information Sheets for Health Professionals
Vital Signs
Acknowledgement Levels of Evidence
This Best Practice Information Sheet has
This Practice Information
been based on a systematic review of Sheet Covers The Following All studies were categorised according to the
strength of the evidence based on the
research relating to vital signs. If you wish Concepts following classification system.
to view the primary references on which
this information sheet is based, they are Level I
available in the systematic review report Evidence obtained from a systematic review
of all relevant randomised controlled trials.
published by the Joanna Briggs Institute. 1. Vital Signs: General
Level II
Introduction Issues Evidence obtained from at least one properly
designed randomised controlled trial.
Patient observations are an important part
of nursing care in that they allow the 2. Vital Signs: Respiratory Level III.1
patient’s progress to be monitored and also Evidence obtained from well designed
ensure prompt detection of adverse events Rates controlled trials without randomisation.
or delayed recovery. Patient observations, Level III.2
or vital signs, traditionally consist of blood Evidence obtained from well designed cohort
pressure, temperature, pulse rate and 3. Vital Signs: Pulse Rate or case control analytic studies preferably
from more than one center or research
respiratory rate. A systematic review was group.
recently conducted addressing issues such
as the purpose of vital signs, the optimal 4. Vital Signs: Blood Level III.3
frequency with which they should be Evidence obtained from multiple time series
Pressure with or without the intervention. Dramatic
conducted, what observations constitute results in uncontrolled experiments.
vital signs and to identify issues related to
the individual measures of temperature, 5. Vital Signs: Temperature Level IV
pulse rate, respiratory rate and blood Opinion of respected authorities, based on
clinical experience, descriptive studies, or
pressure. reports of expert committees.
This Best Practice Information Sheet inconsistent and at times inter-changeable. What Constitutes Vital Signs
summarises current best evidence on the The term vital signs suggests measurement Traditionally, the term “vital signs” is used
topic. In this information sheet, the term of vital or critical physiologic functions, in reference to the measurement of
observations refers to patient observations where as the term “observations” implies temperature, respiratory rate, pulse rate
in general, while vital signs is used in broader range of measures. While there and blood pressure. However, within the
reference specifically to temperature, is no clear definition in the literature, the literature there are suggestions that these
pulse, respiration and blood pressure. panel of experts which guided the system-
parameters could be supplemented with
atic review process argued that observa-
other useful measures such as nutritional
Vital Signs: General Issues tions is the more appropriate term, in that
it more accurately reflects current clinical status, smoking status, spirometr y,
practice. This implies that patient obser- orthostatic vital signs and pulse oximetry.
Vital Signs versus Observations
The measurement of temperature, pulse, vations need not be limited to the tradi- However, only pulse oximetr y and
heart rate and blood pressure is termed tional four parameters but supplemented determining a patient’s smoking status have
both vital signs and observations. Neither with other measures as indicated by the been shown to actually change the practice
have been well defined and their use is patient’s clinical status. of clinicians.
volume 3, issue 3, page 1, 1999
Studies have demonstrated that in some of this is based on surveys of nurses, clini- breaths per minute, thereby questioning the
situations pulse oximetry is useful for cal practice reports and expert opinion. value of having a “cut-off” at 50 breaths
detecting a deterioration in physiological Surveys of nurses have shown that many per minute as the indicator of serious res-
function that might otherwise be missed. admit to carrying out frequent vital sign piratory illness. It has also been reported
This has resulted in a reduction in the measurements on patients they believed did that factors such as crying, sleeping, agi-
number of investigations undertaken and not require them, and that they had be- tation and age have a significant influence
has changed the planned management of come a routine procedure unrelated to per- on the respiratory rate. As a result of these
patients. On this basis, pulse oximetry has ceived individual patients needs. and similar studies the value of respira-
been recommended as a useful addition tory rate as an indicator of serious illness
to the four traditional measures of Two studies evaluated the impact of reduc- is limited.
physiologic status. ing the frequency of post-operative obser-
vations, but both involved only minor Vital Signs: Pulse Rate
The use of the concept “smoking status is a changes to measurement frequency. One There has been very little research
vital sign” has been evaluated during the practice report describes the change from evaluating the measurement of pulse rates.
initial patient encounter and has been 15 and 30 minutely vital sign measurement It is likely, that when heart rate is of
shown to increase the likelihood that during a blood transfusion, to vital signs concern, cardiac monitors are used to
counselling and smoking cessation advice only at commencement, at 15 minutes and determine not only rate, but also rhythm.
would be provided by the health care on completion. This report used visual ob- The role of the “pattern of the pulse”, for
worker. While this parameter does not fit servation to monitor patient status at other example regular pulse versus irregular
within the traditional concept of vital signs times during the transfusion, and suggest pulse or strong pulse versus weak pulse,
or patient observations, it may still have there was no compromise to safe practice. have not been addressed in the context of
an important role during the initial patient However, the strength of this evidence is vital signs or patient observations. On this
assessment. limited and so cannot be used to justify basis, an important role of pulse rate
practice change. The “vital signs” system- monitoring will likely be to identify when
Other proposed vital sign measurements, atic review concluded that there has been
more advanced monitoring is required.
such as nutritional and orthostatic vital little serious evaluation of the optimal fre-
signs, have not been shown to have an quency of patient observations.
Measurement of a person’s pulse rate in
influence on patient management. While the presence of atrial fibrillation was
many other measures and scales exist, their Vital Signs: Respiratory Rate evaluated and results suggest that pulse
role within the framework of patient There is only limited research relating to rate, measured apically using a
observations has yet to be determined. monitoring respiratory rate, and these stethoscope for a 60 second count period,
Indeed, in some situations simple visual studies focused on issues such as the is likely to be the most accurate rate. This
observation of the patient may be all that inaccuracy of respiratory rate measurement study noted that 86% of nurses under-
is required in terms of monitoring the and respiratory rate as a marker for estimated the pulse rate, and that as the
patient’s progress and clinical status, yet respiratory dysfunction. heart rate increased the magnitude of error
this has still to be addressed. also increased. Another study
Inaccuracies in respiratory measurement recommended a 30 second count period
have been reported in the literature. One as the most accurate and efficient way of
Limitations
study compared respiratory rate counted measuring pulse rate, noting that the 15
Based on the findings of a small number using a 15 second count period, to a full second count time was the least accurate.
of studies, it appears that vital signs are minute, and found significant differences
quite limited in terms of detecting important A third study found that there was no
in the rates. Respiratory rates measurement
physiologic changes. Examples of this advantage in using the longer 60 seconds,
in children under five years, for a 30 sec-
include: their failure to detect large blood over the 15 or 30 second count periods.
ond or 60 second period, suggesting the
losses, to identify serious illness in infants, These researchers suggest that counting an
60 seconds resulted in the least variability.
and their inability to detect an inadequate accurate pulse rate may be more difficult
Another study found that rapid respiratory
plasma volume in burn injury patients. One than commonly recognised.
rates in babies, counted using a stetho-
retrospective study of patients with severe scope, were 20% to 50% higher than those
thoracoabdominal injury found that A study assessing infants apical pulse rate
counted from beside the cot without the aid
normal or stabilised post injury vital signs using a stethoscope, suggested that length
of the stethoscope.
did not signify that life threatening of time may not be the primary factor in
haemorrhage was absent. These studies errors, and that like respiratory rate, pulse
The value of respiratory rate as an indica-
suggest that the usefulness of vital signs is tor of potential respiratory dysfunction has rate also appears to be influenced by infant
perhaps more as an indicator for the need been investigated but findings suggest it is states in addition to illness.
of further more appropriate investigations. of limited value. One study found that only
It is therefore important to note that normal 33% of people presenting to an emergency While these studies have identified that the
vital sign parameters do not guarantee a department with a oxygen saturation be- accuracy of pulse rate measurements is
stable physiological status. low 90% had an increased respiratory rate. influenced by the number of seconds that
An evaluation of respiratory rate for the the pulse is counted, the clinical
Frequency of Vital Signs differentiation of the severity of illness in significance of these findings is unclear. The
There is only limited information regard- babies under 6 months found it not to be contradictory findings of studies suggest
ing the frequency with which patient ob- very useful. Approximately half of the ba- that the count period used to determine
servation should be undertaken and much bies had a respiratory rate above 50 pulse rate is of only limited significance.
volume 3, issue 3, page 2, 1999
Vital Signs: Blood Pressure Cuff Size Bell versus Diaphragm
Studies addressing the measurement of The length and width of the inflatable cuff The accuracy of blood pressures measured
blood pressure with a sphygmomanometer (bladder) that is used during the with the bell or the diaphragm of the
measurement of blood pressure may be a stethoscope have been investigated. One
have focused on issues such as the accu-
source of error. Much of the research has study found the bell of the stethoscope
racy of indirect blood pressure, palpation
focused on cuff width, (the dimension resulted in higher readings than those
versus auscultation cuff size, position of
across along the bladder) as the potential taken using the diaphragm. These results
arm during measurements and health care
source of this error. The standard width of were supported by another study, with
workers technique.
currently available cuffs is approximately researchers recommending the use of the
12cm, with both larger and smaller sizes bell for all blood pressure measurements.
Direct versus Indirect
Several studies have compared direct (in- also available. Studies have shown that the
Health Care Workers Technique
tra-arterial) and indirect (auscultation) use of a cuff that is too narrow results in
The technique used by health care work-
measurements of blood pressure. There an overestimation of blood pressure, and
ers to measure blood pressure has been
appears to be little significant difference a cuff that is too wide underestimates blood
shown to differ from recommended prac-
in systolic pressures measured by either pressure. Length of cuff appears to have
tice. Using the American Heart Associa-
method, with differences ranging from 3 little influence on accuracy. tion Guidelines as the standard, one study
mmHg in two studies to 12mmHg in a third. found that 57% of nursing students failed
Differences in diastolic blood pressure are For obese people it has been suggested to comply with these guidelines in areas
greater, and are influenced by the refer- that large cuffs (15cm width) will be such as cuff placement, estimation of
ence point that is used. When the phase V required when the person’s arm systolic pressure by palpation, calculation
Korotkoff’s sound is used (disappearance circumferences is between 33 –35cm, and of proper inflation pressure, and proper
of the sound), both methods provide simi- a thigh cuff (18cm width) may be needed stethoscope placement. Another study of
lar pressures. However when the phase IV if the arm circumferences is greater than 172 health care workers concluded that
Korotkoff’s sound (muffling), is used, aus- 41cm. However, difficulties in applying nurses and physicians evaluated blood
cultated measurements are significantly thigh cuffs to large arms have been pressure in an inadequate, incorrect and
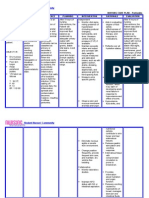
Table One
Korotkoff’s Sounds
Measurement of blood pressure by auscultation is based on the sounds produced as a result of changes
in blood flow, termed Korotkoff’s sounds, and are:
1. Phase I The pressure level at which the first faint, clear tapping sounds are heard, which increase as the
cuff is deflated (reference point for systolic BP).
2. Phase II During cuff deflation when a murmur or swishing sounds are heard.
3. Phase III The period during which sounds are crisper and increase in intensity.
4. Phase IV When a distinct, abrupt, muffling of sound is heard
5. Phase V The pressure level when the last sound is heard (reference point for diastolic BP).
greater than intra-arterial pressures (see reported. Cuff width may also be important inaccurate way, and that only 3% of gen-
when measuring blood pressure in eral practitioners and 2% of nurses ob-
table one). A study in children reported
neonates and a cuff width equal to tained reliable results. Two studies evalu-
the use of either auscultation or palpation ating the impact of education programs
overestimated systolic pressure. See table approximately 50% of the arm on blood pressure measurement, found
two for current recommended practice for circumference has been recommended. they increased agreement between the dif-
the measurement of blood pressure. ferent blood pressure readings and also
Arm and Body Position significantly reduced differences in opera-
Comparisons of blood pressures measured tor technique.
Palpation versus Auscultation
A comparison between systolic blood pres- in the sitting person with their arm sup-
Limitations
ported horizontally or with the arm rest- A descriptive study of blood pressures in
sure measurements taken by auscultation
ing at their side, have found an average critically ill patients who had suffered a
and palpation found both were within 8
difference in systolic pressure of 11mmHg cardiac arrest highlighted some limitations
mmHg. While palpation has been commonly
and diastolic pressure of 12mmHg. When to these measurements. Of the 15 patients
limited to the measurement of systolic blood investigated, 5 patients had adequate
the arm was placed above or below the
pressure, one study reported that diastolic intra-arterial blood pressures, but
level of the heart, blood pressure meas-
pressures could be accurately palpated us- unreadable cuff pressures. Four patients
urements changed by as much as had cuff pressures approaching normal,
ing the brachial artery to identify the sharp
20mmHg. As a result of this, it has been but had an inadequate cardiac output. This
phase IV Korotkoff’s sound, However, the
recommended that blood pressures be study suggests that indirect blood pressure
value of this technique in clinical practice, measurements do not always accurately
taken in the sitting position with arm sup-
and its accuracy when used by health care ported horizontally at approximately heart reflect haemodynamic status of critically ill
workers, has yet to be demonstrated. level. people.
volume 3, issue 3, page 3, 1999
Table Two
Recommended Blood Pressure Measurement Technique
Based on published information, below is a summary of the
recommended practice
• Patient should be seated and have rested for 5 minutes and have arm supported
at heart level.
• Appropriate cuff size should be used, and the bladder should nearly (at least
80%) or completely encircle arm.
• Patients should not have smoked or ingested caffeine within 30 minutes before
measurements.
• Measurements should be taken with a mercury sphygmomanometer, a recently
calibrated aneroid manometer, or a calibrated electronic device.
• Both systolic and diastolic blood pressure should be recorded.
• Korotkoff’s phase V (disappearance of sound) should be used for the diastolic
reading.
• Two or more readings, separated by 2 minutes, should be averaged, and more
taken if they differ by more than 5mmHg.
Vital Signs : Oral Temperatures thermometers to accurately
Studies evaluating measure- record the person’s oral
Temperature ments from the different areas temperature. One study found
The largest volume of research of the mouth recommend using that with healthy adults, using
identified during the literature either the right or left posterior a two minute insertion time
search addressed various sublingual pocket, as these resulted in 27% of the
aspects of temperature result in higher recorded temperature readings having
measurement. These studies temperatures. an error of at least 0.3°C. A
highlight the large range of study assessing thermometer
methods and body sites that Evaluation of the impact of insertion time in afebrile and
are used for the measurement oxygen therapy on oral febrile adults, suggested a six
of temperature (see table temperatures have reported minute insertion time as a
three). Because of the volume contradictory results regarding compromise between optimal
of research, comparisons of its statistical significance, time and clinical practicality
different temperature however no study reported a while another recommended a
measurement methods will be clinically significant effect. seven minute insertion time to
summarised as a separate Similarly, different rates of ensure the majority of afebrile
systematic review. Summarised oxygen flow, from 2 litres to 6 and febrile temperatures are
in this practice information litres per minute, and warmed correctly recorded. However, a
sheet are studies addressing or cooled inspired gas, were survey of nurses showed that
aspects of oral, rectal axillary found not to have an influence most left the mercur y
and tympanic temperatures. on oral temperature thermometer in the mouth for
measurements. Two studies less than 3 minutes.
General Issues found that rapid respiratory
While much attention has rates had a small influence on Axillary Temperature
focused on measurement oral temperatures, but these There has been only limited re-
accuracy, one study evaluated results were contradicted by search focusing on axillary
touch as a screen for fever and another study that found temperatures. One study
found that while mothers and neither rapid or deep evaluated axillary temperature
medical students overestimated breathing, alone or in measurements in elderly fe-
the incidence of fever when combination, had any males, and found great varia-
using touch, they rarely missed significant effect on oral tion between individuals.
its presence in a child. The temperatures. While the mean axillary tem-
results of this study perhaps peratures were approximately
challenge the current focus of Studies have shown that 36°C, the wide range of tem-
research on the accuracy of drinking hot or cold water has peratures encountered pre-
measurements using tenths of a significant impact on vented the identification of a
a degree, when simple touch recorded oral temperatures, single figure that could be con-
is an accurate measure for and it has been suggested sidered the “normal” axillary
fever. The use of temperature waiting 15 to 20 minutes after temperature. Another study
as a discharge criterion for an drinks to ensure accuracy. evaluated the influence of in-
ambulatory surgical unit has Smoking does not change oral travenous infusions, via upper
been studied, but results temperature measurements. limbs of neonates, on axillary
suggest it is not useful in temperatures and found there
differentiating readiness for Researchers have evaluated the was little significance in terms
discharge. time required for mercury of the temperature accuracy.
volume 3, issue 3, page 4, 1999
Tympanic Temperature
There has been considerable research addressing tympanic temperature measurements ranging from the
influence of infection and cerumen on measurement accuracy, to optimal technique. Studies have evaluated
the impact of otitis media on tympanic temperatures and suggest it has little effect. While some studies have
reported a statistically significant difference in tympanic temperatures between ears in people with unilateral
otitis media, this difference was approximately 0.1°C and so of little clinical importance. The presence of
cerumen does influence tympanic temperature readings, and while results are variable, they suggest a
significant proportion of the temperature readings taken from the occluded ear will be more than 0.3°C
lower than the ear that is not occluded.
Studies evaluating technique suggest an ear tug should be used during the measurement of tympanic
temperatures, as this is reported to straighten the external auditory canal. Failure to use the ear tug means
infrared thermometers are only partially directed at the tympanic membrane. The tug technique in adults
has been described as pulling the pinna (auricle of ear) in an upward and backward direction, and in
infants it is pulling the pinna in a backward direction.
Evaluations of the impact of ambient temperatures on tympanic temperatures suggest that while a hot
environment can significantly affect readings, cold appears to have little effect.
Cost analyses of the different temperature measurement methods suggest infrared measurements may be
the most cost effective despite the greater initial costs. These savings are the result of the rapid reading
capabilities of these instruments, and the labour cost savings that result.
Rectal Temperature
Many studies have compared the different methods of temperature measurement, and commonly rectal
temperatures are used as the standard comparison. However, these studies will be summarised in a separate
systematic review. The most common reported issue related to rectal temperature measurement is that of
rectal perforation, which appears to be a risk primarily for the newborn and very young. Other reported
complications include peritonitis secondary to rectal perforation, and one case of intra-spinal migration of
a rectal thermometer in a two year old, which broke during routine rectal temperature measurement. A ten
year review of hospital records identified 16 children admitted to a surgical unit with broken or retained
rectal thermometers. In response to this problem axillary temperature measurements have been recommended
in preference to the rectal measurements. With the advent of infrared tympanic thermometers, these
complications are likely to become less common.
Table Three
Temperature Measurement
The different body areas that have A wide range of instruments have been
been used for the measurement of used to measure these temperatures,
body temperature include: and include:
• mouth • glass mercury thermometer
• axilla • electronic thermometer
• tympanic membrane
• pulmonary artery catheter
• rectum
• skin surface • endotracheal tube with temperature
• pulmonary artery probe
• nose • urinary catheter with temperature
• groin probe
• oesophagus • liquid crystal thermometer strip
• trachea
• disposable thermometers
• urinary bladder
• urine • infrared (tympanic) thermometers
volume 3, issue 3, page 5, 1999
Implications For Practice
While much research has been undertaken on specific aspects of patient observations, such as the accuracy of individual
measurements, there is little research addressing the broader issues of the most effective and efficient way to monitor patient
progress. However, there is a need for clinical areas to determine the role of patient observations within their setting, with
particular reference to the four traditional vital sign parameters, to ensure:
1. observations are appropriate as determined by the patient’s clinical status;
2. available technologies are utilised appropriately, to complement or even replace less effective methods of patient
observation; and
3. inappropriate observations, based on habit rather than need, should be minimised.
Other issues identified during the systematic review that impact on clinical practice include:
1. the term “observations” should be used in preference to “vital signs”, as this better reflects the diversity of what may
constitute patient monitoring;
2. the rectum should not be the first site of choice for the measurement of temperature;
3. normal vital sign parameters do not guarantee normal physiologic status;
4. education programs will likely be effective in improving health care workers blood pressure measurement technique; and
5. while many factors can have a small influence on the accuracy of vital sign measurements, there may be a cumulative
effect, and so organisations should promote a standardised method for all measurements.
Recommendations
Because of the lack of evidence relating to most of the broader issues of patient observation, these recommendations have
been generated by the expert panel, and have been rated level IV evidence (expert opinion)
• The specific patient observations, their frequency and duration, should be based on clinical assessment rather than protocol
alone.
• Patient observations should be performed as often as indicated by the patient’s clinical status.
• Beginner practitioners should validate their clinical assessment with a more experienced practitioner.
• Vital signs should not be used as a way to ensure frequent visits by the nurse.
• When visual checks or inspection of the patient are all that is indicated by the patient’s clinical status, this should be an
acceptable form of patient observation.
• Health care workers should be trained to perform patient observations in a standardised manner within each institution, and
be made aware of the risks and limitations associated with this activity.
• Pulse oximetry should be considered a vital sign in situations where accurate assessment and monitoring is critical.
Other issues of importance noted by the panel of experts include:
• Clinical areas should identify who has responsibility for determining the frequency and nature of patient observations.
• Trends in observations will likely be more important than single measures.
• What happens to the information after it is collected is as important as the accuracy of individual parameters.
Acknowledgements
For further information contact: This publication was produced based on a
• The Joanna Briggs Institute for Evidence Based Nursing and Midwifery, Margaret Graham systematic review of the research literature
Building, Royal Adelaide Hospital, North Terrace, South Australia, 5000. undertaken by The Joanna Briggs Institute
http://www.joannabriggs.edu.au, ph: (08) 8303 4880, fax: (08) 8303 4881 under the guidance of a review panel of
• NHS Centre for Reviews and Dissemination, Subscriptions Department, Pearson Professional, clinical experts, and was led by Mr. David
PO Box 77, Fourth Avenue, Harlow CM19 5BQ UK. Evans – Coordinator of Reviews, The Joanna
• AHCPR Publications Clearing House, PO Box 8547, Silver Spring, MD 20907 USA. Briggs Institute; Mr. Brent Hodgkinson –
Research Officer, The Joanna Briggs Institute;
“The procedures described in Best and Ms Judith Berry – Nursing Director, The
Practice must only be used by Royal Adelaide Hospital. The Joanna Briggs
Disseminated collaboratively by: people who have appropriate Institute would like to acknowledge and
expertise in the field to which the thank the review panel members whose
procedure relates. The applicability expertise was invaluable throughout this
of any information must be activity. The review panel members were:
established before relying on it. • Ms Judith Berry
While care has been taken to ensure • Ms Heidi Silverston
that this edition of Best Practice • Mr Peter Le-Gallou
summarises available research and • Ms Deb Henrys
expert consensus, any loss,
• Ms Kathy Read
damage, cost, expense or liability
• Ms Lee Hussie
suffered or incurred as a result of
reliance on these procedures • Ms Sue Edwards
(whether arising in contract, • Ms Annette Heinmann
negligence or otherwise) is, to the • Ms Hazel Morrison
extent permitted by law, excluded”. • Mr Lyell Brougham
volume 3, issue 3, page 6, 1999
You might also like
- Documentation of Vital Signs During The Post-Operative PhaseDocument43 pagesDocumentation of Vital Signs During The Post-Operative PhaseYam Esor OsomrofNo ratings yet
- Assessment 2 Vital Signs Normal ValuesDocument4 pagesAssessment 2 Vital Signs Normal Valuesthannikkotte12345No ratings yet
- Smart Health Monitoring Systems - An Overview of Design and Modeling - Baig - 2013Document14 pagesSmart Health Monitoring Systems - An Overview of Design and Modeling - Baig - 2013Shâmara Stéfany GuimarãesNo ratings yet
- D XplainDocument10 pagesD XplainAnuragNo ratings yet
- Intermittent Positive Pressure Breathing (IPPB) PDFDocument10 pagesIntermittent Positive Pressure Breathing (IPPB) PDFKellie PacanowskiNo ratings yet
- MastectomyDocument53 pagesMastectomyAngelica RelanaNo ratings yet
- WHO: World Health Statistics 2016Document136 pagesWHO: World Health Statistics 2016The Independent Magazine100% (1)
- Fluid and Electrolyte Imbalance QuizDocument2 pagesFluid and Electrolyte Imbalance QuizteabagmanNo ratings yet
- Lesson 6 11midtermDocument28 pagesLesson 6 11midtermREIMOND VINCE MENDOZANo ratings yet
- Jean Lèonard Marie Poiseuille PPT FINALDocument12 pagesJean Lèonard Marie Poiseuille PPT FINALDirkMyburghNo ratings yet
- Operating Room Attire 2018Document5 pagesOperating Room Attire 2018andrea rabangNo ratings yet
- Introduction To Community and Public HealthDocument21 pagesIntroduction To Community and Public HealthSanaNo ratings yet
- ICTM111 PDF 02 - Healthcare System, Health System Framework & PH Health SystemDocument4 pagesICTM111 PDF 02 - Healthcare System, Health System Framework & PH Health SystemJamNo ratings yet
- CHAPTER 24-Nursing InformaticsDocument6 pagesCHAPTER 24-Nursing InformaticsAdrian MallarNo ratings yet
- 13.knowledge and Practices of Universal Precautions Among Basic B. Sc. Nursing StudentsDocument10 pages13.knowledge and Practices of Universal Precautions Among Basic B. Sc. Nursing StudentsPutri Alin Kende RiaralyNo ratings yet
- CPG Management of Ischaemic Stroke (2nd Edition)Document64 pagesCPG Management of Ischaemic Stroke (2nd Edition)umiraihana1100% (1)
- DOH Administrative Order 2020-0008Document20 pagesDOH Administrative Order 2020-0008qmmc.adjudicatormd100% (1)
- CanserDocument50 pagesCansertarek ahmed100% (1)
- Role of ICT For HealthDocument29 pagesRole of ICT For HealthDejen AgaziuNo ratings yet
- Ambulance and Emergency Equipment - Catalogue - en PDFDocument28 pagesAmbulance and Emergency Equipment - Catalogue - en PDFSteven BrownNo ratings yet
- Shortness of BreathDocument49 pagesShortness of BreathMetkaNo ratings yet
- Florence Nightingale: TranscriptDocument4 pagesFlorence Nightingale: TranscriptJuan Carlos PASQUEL G.No ratings yet
- Heimlich Maneuver PDFDocument7 pagesHeimlich Maneuver PDFMark DomingoNo ratings yet
- Trans - Mls 101 - Chapter 4Document3 pagesTrans - Mls 101 - Chapter 4Camille De CastroNo ratings yet
- Prelim To Finals RT 203 1Document71 pagesPrelim To Finals RT 203 1Leopardas, Lynn Clemard C.100% (1)
- Ethics in Biomedical Engineering PDFDocument2 pagesEthics in Biomedical Engineering PDFCarrieNo ratings yet
- Hospital Management Information System ProjectDocument4 pagesHospital Management Information System ProjectAlfredo Jimenez CharlesNo ratings yet
- Psychosocial Aspect of PainDocument21 pagesPsychosocial Aspect of PainLaiba WarisNo ratings yet
- Dr. Teodora Tiglao Mother of Philippine Public HealthDocument4 pagesDr. Teodora Tiglao Mother of Philippine Public HealthJamie CastilloNo ratings yet
- Nursing Informatics: Click To Edit Master Subtitle StyleDocument87 pagesNursing Informatics: Click To Edit Master Subtitle StyleColeen VillegasNo ratings yet
- Technical Specifications For Dialysis MachineDocument2 pagesTechnical Specifications For Dialysis MachineJohn Son G100% (1)
- Questionnares NeuroDocument29 pagesQuestionnares NeuroKirk Patrick MojicaNo ratings yet
- Chapter 001Document8 pagesChapter 001Lisa SzyszkaNo ratings yet
- Laundering Honour Trainer S NotesDocument6 pagesLaundering Honour Trainer S Notessmokeytonga100% (1)
- Lesson 9: Hospital Information SystemDocument11 pagesLesson 9: Hospital Information SystemClarisse De GuzmanNo ratings yet
- Group 3: BSSW As3-1Document25 pagesGroup 3: BSSW As3-1Jenecile ParambitaNo ratings yet
- Chapter 9 - Security, Privacy, Etchic & ErgonomicDocument38 pagesChapter 9 - Security, Privacy, Etchic & ErgonomicNur Amira NadiaNo ratings yet
- His Module 4 - Overview of Health InformaticsDocument11 pagesHis Module 4 - Overview of Health InformaticsLYKS DelesNo ratings yet
- 01 Cytogenetics Introduction History PDFDocument2 pages01 Cytogenetics Introduction History PDFDanNo ratings yet
- Relationships Between Patient Satisfaction, Quality, Outcomes and Ownership Type in US Hospitals An Empirical StudyDocument357 pagesRelationships Between Patient Satisfaction, Quality, Outcomes and Ownership Type in US Hospitals An Empirical StudyHandsome Rob100% (1)
- Protokol Critical ApraisalDocument16 pagesProtokol Critical ApraisalMustika ayu lestariNo ratings yet
- Problem Set 3Document19 pagesProblem Set 3Alomenu Samuel100% (1)
- Chapter 1 - Project and It's BackgroundDocument15 pagesChapter 1 - Project and It's Backgroundcharimaine hernandezNo ratings yet
- Automatic Anesthesia Controller Using Heart Beat Sensor-MEDICAL ELECTRONICS PROJECTSDocument6 pagesAutomatic Anesthesia Controller Using Heart Beat Sensor-MEDICAL ELECTRONICS PROJECTSR.ASHOKKUMAAR100% (2)
- Electronics in Biomedical and InstrumentationDocument9 pagesElectronics in Biomedical and InstrumentationchanlalNo ratings yet
- Rheumatic Heart Disease: Emmanuel Edafe Consultant Interventional Cardiologist, NduDocument36 pagesRheumatic Heart Disease: Emmanuel Edafe Consultant Interventional Cardiologist, NduPrincewill SeiyefaNo ratings yet
- A Project Proposal On Hospital Management System in JavaDocument2 pagesA Project Proposal On Hospital Management System in JavaPirzada SwatiNo ratings yet
- Syllabus For BPKMCH NEPALDocument7 pagesSyllabus For BPKMCH NEPALDeep SharmaNo ratings yet
- Ms-08 Comlete Book - Unit - 9Document305 pagesMs-08 Comlete Book - Unit - 9anandjaymishra0% (1)
- Synopsis On Wearable Bio SensorsDocument5 pagesSynopsis On Wearable Bio Sensorsajay_467409877No ratings yet
- Bachelor of Nursing Science With HonourDocument10 pagesBachelor of Nursing Science With HonourNURUL FARADILA BINTI OTHMAN STUDENTNo ratings yet
- Introduction To Patient SafetyDocument54 pagesIntroduction To Patient Safetyrejoicedear2020No ratings yet
- Concept II-Vital StatisticsDocument10 pagesConcept II-Vital Statisticsjpoti100% (1)
- Overview of Health InformaticsDocument2 pagesOverview of Health InformaticsERESTALL SENNDI GRACE OLIVERASNo ratings yet
- Differences Between Skeletal, Smooth and Cardiac MuscleDocument10 pagesDifferences Between Skeletal, Smooth and Cardiac MuscleksbabarNo ratings yet
- Arcega, Romar Rico H. Bsn-Iii NCM 116 1. What Educational Topics Should The Nurse Provide The Family About Home Care For The Patient After Stroke?Document1 pageArcega, Romar Rico H. Bsn-Iii NCM 116 1. What Educational Topics Should The Nurse Provide The Family About Home Care For The Patient After Stroke?R Hornilla ArcegaNo ratings yet
- ICTDocument10 pagesICTShanmugapriyaVinodkumarNo ratings yet
- Interventii AMDocument7 pagesInterventii AMgary_vlaicu3850No ratings yet
- The Level of EvidanceDocument6 pagesThe Level of EvidanceyoezufNo ratings yet
- 5 Semne VitaleDocument7 pages5 Semne VitaleCamelia GrigorașNo ratings yet
- AAT "Disaster Management" EMS Kit For Up To 3 Stretchers: 1 FunctionDocument4 pagesAAT "Disaster Management" EMS Kit For Up To 3 Stretchers: 1 FunctionElsye FitriasariNo ratings yet
- ECG Rhythm InterpretationDocument27 pagesECG Rhythm InterpretationElsye FitriasariNo ratings yet
- ECG Rhythm Interpretation: Acute Myocardial InfarctionDocument25 pagesECG Rhythm Interpretation: Acute Myocardial InfarctionElsye FitriasariNo ratings yet
- EkgDocument21 pagesEkgElsye FitriasariNo ratings yet
- MCQ Psy Exam Group BDocument17 pagesMCQ Psy Exam Group BsalamredNo ratings yet
- Blood Transfusion Policy 6.3Document90 pagesBlood Transfusion Policy 6.3raNo ratings yet
- Cell Power ECourseDocument25 pagesCell Power ECoursekeithmac100% (1)
- Q 7Document21 pagesQ 7Buii AhNo ratings yet
- Common Pediatric Illnesses in The Er UrgentDocument46 pagesCommon Pediatric Illnesses in The Er UrgentDr mohamedNo ratings yet
- GigaMune Rep-Seq Technical NoteDocument2 pagesGigaMune Rep-Seq Technical NoteAndro HsuNo ratings yet
- Application of Pharmaceutical GelatinDocument4 pagesApplication of Pharmaceutical GelatinShakrie AbdullahNo ratings yet
- 6 DOH Sample FormsDocument136 pages6 DOH Sample FormsSir Cris CapiliNo ratings yet
- GRIFTDocument15 pagesGRIFTjellyjohnNo ratings yet
- Saep 1141Document66 pagesSaep 1141shaban100% (2)
- List of Minimum Requirements For Hospital ForDocument3 pagesList of Minimum Requirements For Hospital ForTayyab Tahir Minhas67% (3)
- Without Grain 100 Delicious Recipes For Eating A Grain-Free - Gluten-Free - Wheat-Free Diet PDFDocument211 pagesWithout Grain 100 Delicious Recipes For Eating A Grain-Free - Gluten-Free - Wheat-Free Diet PDFChuôngGió100% (1)
- FORM LPLPO & Permintaan TRIBULANDocument640 pagesFORM LPLPO & Permintaan TRIBULANMARTININo ratings yet
- STG Final Dec 2020Document1,215 pagesSTG Final Dec 2020Bereket GGNo ratings yet
- Anaesthesiology NAGY TESZTKÖNYVDocument1,064 pagesAnaesthesiology NAGY TESZTKÖNYVoroszgabor100% (10)
- Development - of - CVS-5Document20 pagesDevelopment - of - CVS-5Ahsan IslamNo ratings yet
- Apamarga Kshara SwitraDocument6 pagesApamarga Kshara SwitraSamhitha Ayurvedic ChennaiNo ratings yet
- Vortex Laser Reiki 1Document17 pagesVortex Laser Reiki 1Volkan VVolkan100% (3)
- Clinical Management of TB and HIVDocument154 pagesClinical Management of TB and HIVapi-3781623100% (3)
- Antifungal DrugsDocument28 pagesAntifungal DrugsKhairunnisa RasyidinNo ratings yet
- NHIS Variable SummaryDocument4 pagesNHIS Variable SummaryJin SiclonNo ratings yet
- (Doc24.vn) Bai-Tap-Tieng-Anh-10-Thi-Diem-Co-Dap-AnDocument14 pages(Doc24.vn) Bai-Tap-Tieng-Anh-10-Thi-Diem-Co-Dap-AnTạ Quang ĐứcNo ratings yet
- Part 6 Anesthesiology: Anesthesiology and Its DevelopmentDocument24 pagesPart 6 Anesthesiology: Anesthesiology and Its DevelopmentburhaninhoNo ratings yet
- Spectrum BrochureDocument16 pagesSpectrum BrochuredimdamflyNo ratings yet
- Good Clinical Practice PDFDocument4 pagesGood Clinical Practice PDFdamera_vineetNo ratings yet
- PeritonitisDocument6 pagesPeritonitisDiane ArgoteNo ratings yet
- Cesarean SectionDocument16 pagesCesarean Sectionjannnjennn67% (3)
- New Eco Ink MsdsDocument7 pagesNew Eco Ink MsdsankitleedsNo ratings yet
- VP Business Operations in Central South NJ Resume Diane MalkinDocument1 pageVP Business Operations in Central South NJ Resume Diane MalkinDianeMalkinNo ratings yet
- Trends in Oncology Business DevelopmentDocument25 pagesTrends in Oncology Business DevelopmentSheltie ForeverNo ratings yet