Professional Documents
Culture Documents
6 Pleural Effusion Nursing Care Plans
Uploaded by
jamieboyRNOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
6 Pleural Effusion Nursing Care Plans
Uploaded by
jamieboyRNCopyright:
Available Formats
Pleural effusion is an accumulation of fluid in the pleural space.
Pleural fluid normally seeps
continually into the pleural space from the capillaries lining the parietal pleura and is reabsorbed
by the visceral pleural capillaries and lymphatic system. Any condition that interferes with either
secretion or drainage of this fluid leads to pleural effusion.
Causes of pleural effusion can be grouped into four major categories:
Increased systemic hydrostatic pressure (e.g., heart failure)
Reduced capillary oncotic pressure (e.g., liver or renal failure)
Increased capillary permeability (e.g., infection or trauma)
Impaired lymphatic function (e.g., lymphatic obstruction caused by tumor)
See other nursing care plans here
Nursing Care Plans
1 Ineffective Breathing Pattern
Ineffective breathing pattern occurs when inspiration and expiration does not provide adequate
ventilation. Pleural inflammation causes sharp localized pain that increases deep of breathing,
coughing and movement. This can result to shallow and rapid breathing pattern. Distal airways
and alveoli may not expand optimally with each breath, increasing the possibility of atelectasis
and impaired gas exchange.
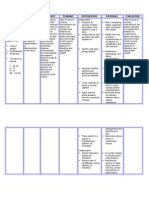
Nursing Nursing Expected
Assessment Planning Rationale
Diagnosis Interventions Outcome
Subjective: Ineffectiv Short Term: - Establish - To gain pt/ Short
e After 3 hours rapport - SO’s trust and Term: The
Dyspnea Breathing of nursing Monitor and cooperation - patient shall
Pattern interventions record vital To obtain have
Objectives: RT the patient signs baseline data demonstrate
Decreased will d appropriate
The patient Lung demonstrate - Assess breath - To note for coping
manifested the Volume appropriate sounds, respiratory behaviors
following: Capacity coping respiratory abnormalities and methods
as behaviors rate, depth and that may to improve
Tachypnea evidenced and methods rhythm indicate early breathing
Presence of by to improve respiratory pattern.
crackles on tachypnea breathing - Elevate head compromise
both lung , presence pattern. of the pt. and hypoxia Long term:
fields upon of
auscultation crackles Long term: - Provide - To promote The patient
use of on both relaxing lung expansion shall have
accessory lung fields After 1 to 2 applied
muscles and
RR of 28 dyspnea days of environment - To promote techniques
nursing adequate rest that
The patient may interventions - Administer periods to limit improved
manifest the , the patient supplemental fatigue breathing
following: would be oxygen as pattern and
able to apply ordered - To maximize be free from
Cyanosis techniques oxygen signs and
Orthopnea that would -Assisst client available for symptoms of
Diaphoresis improve in the use of cellular uptake respiratory
breathing relaxation distress AEB
pattern and technique -To provide respiratory
be free from relief of rate within
signs and - Administer causative normal
symptoms of prescribed factors range,
respiratory medications as absence of
distress. ordered - For the cyanosis,
pharmacologica effective
-Maximize l management breathing
respiratory of the patient’s and minimal
effort with condition use of
good posture accessory
and effective -To promote muscles
use if wellness during
accessory breathing.
muscles. - to limit fatigue
-Encourage
adequate rest
periods
between
activities
2 Impaired Gas Exchange
Impaired gas exchange is a state in which there is excess or deficit oxygenation and carbon
dioxide elimination. The compensatory mechanism of lungs is to lose effectiveness of its defense
mechanisms and allow organisms to penetrate the sterile lower respiratory tract where
inflammation develops. Disruption of mechanical defenses and ciliary motility leads to
colonization of lungs and subsequent infection. Inflamed and fluid-filled alveolar sacs cannot
exchange oxygen and carbon dioxide effectively. The release of endotoxins by the microbes can
lodge in the brain, affecting the respiratory center in medulla resulting to altered oxygen supply.
Nursing Nursing Inter- Expected
Assessment Planning Rationale
Diagnosis ventions Outcome
Subjective: Impaired Short term: - Establish rapport - - To gain Short term:
(none) Gas After 1 hour Monitor and record pt./SO’s trust The patient
Objective: Exchange of nursing vital signs and cooperation shall have
R/T Alveolar interventions, - To obtain verbalized
The patient –Capillary the pt will - Monitor respiratory baseline data understandin
manifested Membrane verbalize rate, depth and g of the
Changes understandin rhythm - To assess for interventions
Several and g of the rapid or shallow given to
episodes of respiratory interventions - Assess pt’s general respiration that improve
pallor fatigue given to condition occur because patient’s
Secondary to improve of hypoxemia condition.
Tachypnea Pleural patient’s - Auscultate breath and stress
Effusion condition. sounds, note areas of Long term:
Restlessnes decreased/adventitiou - To note for
s Long term: s breath sounds as etiology The patient
well as fremitus precipitating shall manifest
nasal After 1-2 factors that can no signs of
flaring days of - Elevate head of the lead to impaired respiratory
nursing pt. gas exchange distress.
depth of interventions,
breathing the pt. will - Note for presence of -To evaluate
demonstrate cyanosis degree of
Use of improved compromise
accessory ventilation -Encourage frequent
muscles for and adequate position changes and - To enhance
breathing oxygenation deep-breathing lung expansion
of tissues exercises
The pt. may AEB absence - To assess
manifest the of symptoms -Provide supplemental inadequate
ff: of respiratory oxygen at lowest systemic
distress. concentration oxygenation or
Confusion indicated by hypoxemia
laboratory results and
Cyanosis client symptoms/ -To promote
situation optimum chest
Diaphoresis expansion
- Review laboratory
results To correct/
improve
- Provide health existing
teaching on how to deficiencies
alleviate pt’s
condition - To determine
pt’s
Administer prescribed oxygenation
medications as
ordered status
- To empower
SO and pt
For the
pharmacologica
l management
of the patient’s
condition
3 Activity Intolerance
Presence of a space-occupying liquid in the pleural space, the lung recoils, inward, the chest wall
recoils outward, and the diaphragm is depressed inferiorly. This may lead to decrease lung
volume and may result to significant hypoxemia and can only be relieved by thoracentesis. Due
to inadequate ventilation there would be limitations in activity as tolerance to activity may occur.
Assessmen Nursing Nursing Inter- Expected
Planning Rationale
t Diagnosis ventions Outcome
Subjective: Activity Short Term: Establish Rapport To gain Short
(none) intolerance After 3-4 Monitor and record clients Term: The
related to hours of Vital Signs participation patient
Objective: insufficien nursing and shall have
t oxygen interventions Assess patient’s cooperation used
Patient for , the patient general condition in the nurse identified
manifested: activities will use patient techniques
of daily identified Adjust client’s daily interaction to improve
generalized living techniques to activities and reduce To obtain activity
weakness improve intensity of level. baseline data intolerance
activity Discontinue
limited intolerance activities that cause To note for Long
range of undesired any Term:
motion as Long Term: psychological abnormalitie
observed changes s and The patient
After 2-3 deformities shall have
use of days of Instruct client in present reported
accessory nursing unfamiliar activities within the measurable
muscles interventions and in alternate ways body increase in
during , the patient of conserve energy activity
breathing will report To prevent intolerance
measurable Encourage patient to strain and .
(+) DOB increase in have adequate bed overexertion
activity rest and sleep
intolerance. Provide the patient To conserve
with a calm and quiet energy and
environment promote
safety
Assist the client in
ambulation to relax the
body
Note presence of
factors that could to provide
contribute to fatigue relaxation
Ascertain client’s to prevent
ability to stand and risk for falls
move about and that could
degree of assistance lead to injury
needed or use of
equipment fatigue
affects both
Give client the client’s
information that actual and
provides evidence of perceived
daily or weekly ability to
progress participate in
activities
Encourage the client
to maintain a positive to determine
attitude current status
and needs
Assist the client in a associated
semi-fowlers position with
participation
Elevate the head of in needed or
the bed desired
activities
Assist the client in
learning and to sustain
demonstrating motivation
appropriate safety of client
measures
to enhance
Instruct the SO not to sense of well
leave the client being
unattended
to promote
Provide client with a easy
positive atmosphere breathing
Instruct the SO to to maintain
monitor response of an open
patient to an activity airway
and recognize the
signs and symptoms to prevent
injuries
to avoid risk
for falls
to help
minimize
frustration
and
rechannel
energy
to indicate
need to alter
activity level
4 Acute Pain
Pain may be considered as Pleuritic chest pain. Pleuritic chest pain derives from inflammation of
the parietal pleura, the site of pleural pain fibers. Occasionally, this symptom is accompanied by
an audible or palpable pleural rub, reflecting the movement of abnormal pleural tissues.
Nursing Nursing Inter- Expected
Assessment Planning Rationale
Dx ventions Outcome
Subjective: Acute Short Term: Assess patient To identify Short Term:
(none) pain After 3-4 pain for intensity, Patient shall
hours of intensity using precipitating factors have
Objective: nursing a pain rating and location to verbalized a
interventions scale, for assist in accurate decrease in
Patient , the location and diagnosis. pain from a
manifested: patient’s for Assessing response scale of 7 to
pain will precipitating determines 3.
(+) DOB decrease factors. Assess effectiveness of
from 7 to 3 the response to medication and Long Term:
Complains to as verbalized medications whether further
chest pain on by the every 5 interventions are The patient
the shall have
patient. minutes required.
thoracostom demonstrate
y site Long Term: Provide To provide d activities
comfort nonpharmacologica and
Facial After 2-3 measures. l pain management. behaviors
grimaces days of that will
upon nursing Establish a A quiet prevent the
movement interventions quiet environment recurrence of
, the patient environment. reduces the energy pain.
Reports of will demands on the
pain on the demonstrate Elevate head patient.
thoracostom activities and of bed.
y area, behaviors Elevation improves
described as that will Monitor vital chest expansion and
sharp prevent the signs, oxygenation.
provoked by recurrence of especially
breathing pain. pulse and Tachycardia and
non- blood pressure, elevated blood
radiating, every 5 pressure usually
with a pain minutes until occur with angina
scale of 7 out pain subsides. and reflect
of 10 compensatory
Teach patient mechanisms
Patient may relaxation secondary to
manifest: techniques and sympathetic
how to use nervous system
Restlessness them to reduce stimulation.
stress.
Confusion Anginal pain is
often precipitated
Irritability by emotional stress
that can be relieved
non-
pharmacological
measures such as
relaxation.
Other nursing diagnoses:
5 Impaired Skin Integrity RT Surgical Procedure [Thoracentesis]
6 Disturbed Body Image RT Insertion of Chest Thoracostomy Tube
You might also like
- 6 Pleural Effusion Nursing Care PlansDocument7 pages6 Pleural Effusion Nursing Care PlansShaina Fe RabaneraNo ratings yet
- 6 Pleural Effusion Nursing Care PlansDocument8 pages6 Pleural Effusion Nursing Care Plansmonisha100% (2)
- NCP For Pleural EffusionDocument4 pagesNCP For Pleural EffusionLilian Linogao71% (7)
- NCP (Pulmonary Embolism)Document3 pagesNCP (Pulmonary Embolism)Nica Respondo75% (12)
- Ncp's FOR PLEURAL EFFUSIONDocument4 pagesNcp's FOR PLEURAL EFFUSIONHania Polangi100% (1)
- Nursing Care Plan - Pulmonary EmbolismDocument3 pagesNursing Care Plan - Pulmonary EmbolismPui_Yee_Siow_6303100% (10)
- NCP Pleural EffusionDocument7 pagesNCP Pleural EffusionEjie Boy Isaga100% (2)
- Nursing Care Plan For A Patient With Pleural EffusionDocument5 pagesNursing Care Plan For A Patient With Pleural Effusionmac042250% (4)
- Asthma Impaired Gas ExchangeDocument2 pagesAsthma Impaired Gas ExchangeNedeve Ozned100% (5)
- Nursing Care Plan For Low SelfDocument3 pagesNursing Care Plan For Low Selfmaimai32426394% (17)
- Acute Respiratory DistressDocument2 pagesAcute Respiratory Distressminaanne100% (3)
- Nursing Care Plan (NCP)Document3 pagesNursing Care Plan (NCP)Sha PinedaNo ratings yet
- CAD Discharge PlanDocument2 pagesCAD Discharge PlanmamiudamNo ratings yet
- NCP Difficulty of Breathing R/T SecretionDocument3 pagesNCP Difficulty of Breathing R/T Secretionherscentasiascribd50% (8)
- Nursing Diagnosis For AsthmaDocument6 pagesNursing Diagnosis For AsthmaTINAIDA33% (3)
- NCP - Impaired Gas ExchangeDocument1 pageNCP - Impaired Gas ExchangeRryje Salleva100% (1)
- Asthma Risk For Activity IntoleranceDocument1 pageAsthma Risk For Activity IntoleranceWdy Tanakht Sparrow100% (4)
- NCP - CapDocument4 pagesNCP - CapSherryNo ratings yet
- NCP - TBDocument2 pagesNCP - TBPahw BaluisNo ratings yet
- Nursing Care Plan For Pneumonia With Diagnosis InterventionsDocument4 pagesNursing Care Plan For Pneumonia With Diagnosis InterventionsJazzmin Angel ComalingNo ratings yet
- Nursing Care Plan Patient EndotrachealDocument2 pagesNursing Care Plan Patient EndotrachealCyrus De Asis67% (6)
- Impaire Spontaneous VentilationDocument4 pagesImpaire Spontaneous VentilationSkyla FiestaNo ratings yet
- Ineffective Breathing Pattern Pneumonia Nursing Care PlanDocument1 pageIneffective Breathing Pattern Pneumonia Nursing Care PlanJasonlee BaluyotNo ratings yet
- Impaired Gas ExchangeDocument2 pagesImpaired Gas ExchangeHanya Bint PotawanNo ratings yet
- NCP - AnxietyDocument1 pageNCP - AnxietyNovie Carla100% (1)
- Nursing Care Plan For Covid-19 PatientDocument4 pagesNursing Care Plan For Covid-19 PatientAkande83% (6)
- Assessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveDocument3 pagesAssessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveMaverick LimNo ratings yet
- Nursing Diagnosis Nursing Intervention Rationale: Prioritized Nursing Problem For AtelectasisDocument2 pagesNursing Diagnosis Nursing Intervention Rationale: Prioritized Nursing Problem For AtelectasisFatima Zainab Matlih IdjiraniNo ratings yet
- Pleural EffusionDocument5 pagesPleural EffusionTerizla MobileNo ratings yet
- NCP EmphysemaDocument9 pagesNCP Emphysemahermesdave188% (8)
- Nursing Care Plan For A Patient With Pleural EffusionDocument4 pagesNursing Care Plan For A Patient With Pleural EffusionTrixie Anne GamotinNo ratings yet
- Nursing Care Plan Hemorrhagic StrokeDocument8 pagesNursing Care Plan Hemorrhagic StrokeJeffrey Dela Cruz50% (4)
- Knowledge Deficit - RegorDocument3 pagesKnowledge Deficit - RegorAdrian MallarNo ratings yet
- NCP - CopdDocument3 pagesNCP - CopdhystericoNo ratings yet
- Nursing Care Plans of Bronchial AsthmaDocument8 pagesNursing Care Plans of Bronchial AsthmaKannanNo ratings yet
- NCPDocument2 pagesNCPJhel NabosNo ratings yet
- COLON CANCER NCP-impaired nutrITIONDocument3 pagesCOLON CANCER NCP-impaired nutrITIONNicole cuencosNo ratings yet
- Myocarditis NCP 2Document8 pagesMyocarditis NCP 2astro_aaron117375% (4)
- Nursing Care PlanDocument1 pageNursing Care Planapi-38118511380% (10)
- NCP Knowledge DeficitDocument2 pagesNCP Knowledge DeficitRose Ann100% (1)
- NCP - Acute Pain Stomach CancerDocument2 pagesNCP - Acute Pain Stomach CancerJohn Michael TaylanNo ratings yet
- NCP For RS-HF (Cor PulmonaleDocument5 pagesNCP For RS-HF (Cor PulmonaleMika Saldaña100% (1)
- Nursing Measures To Maintain Normal Respiratory Function and OxygenationDocument2 pagesNursing Measures To Maintain Normal Respiratory Function and Oxygenationlodeth100% (2)
- Nursing Care Plan: Epidural Hematoma Post CraniotomyDocument14 pagesNursing Care Plan: Epidural Hematoma Post CraniotomyTepperoni78% (23)
- PowerlessnessDocument2 pagesPowerlessnessArlan Abragan0% (2)
- NCP Lung CancerDocument4 pagesNCP Lung CancerShizuen Mn83% (12)
- Nursing Care Plan Ineffective Breathing Pattern Hepatic MassDocument2 pagesNursing Care Plan Ineffective Breathing Pattern Hepatic MassRheegell Ellar-Fuertes100% (3)
- Ncp-Impaired S.i.-NavidasDocument4 pagesNcp-Impaired S.i.-NavidasFran LanNo ratings yet
- Pleural Effusion NCPsDocument7 pagesPleural Effusion NCPsJaja Nagallo100% (2)
- NCP Pleural EffusionDocument7 pagesNCP Pleural EffusionKristian Karl Bautista Kiw-isNo ratings yet
- NCP Nasal PolypsDocument3 pagesNCP Nasal Polypsnickanel60% (5)
- NCP For MGDocument1 pageNCP For MGSandra MedinaNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanRachelleNo ratings yet
- KwejtaheroadDocument6 pagesKwejtaheroad4258m5pb8vNo ratings yet
- Nursing Care Plan: Lipa City CollegesDocument13 pagesNursing Care Plan: Lipa City CollegesVincent Maralit MaterialNo ratings yet
- Case Pres Ncps FinalDocument13 pagesCase Pres Ncps FinalMariejoy YadaoNo ratings yet
- NCP Pagalanan PablicoDocument15 pagesNCP Pagalanan PablicoRyrey Abraham PacamanaNo ratings yet
- Nursing Care Plan: Lopez, Maria Sofia B. 9/29/2020 3-BSN-B Prof. ZoletaDocument5 pagesNursing Care Plan: Lopez, Maria Sofia B. 9/29/2020 3-BSN-B Prof. ZoletaSofiaLopezNo ratings yet
- AssessmentDocument2 pagesAssessmentEjoy Rayos AdawagNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument4 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationTrisha SuazoNo ratings yet
- Top 10 NLE Passers (May 2014)Document2 pagesTop 10 NLE Passers (May 2014)Coolbuster.NetNo ratings yet
- Nursing Care Plan - HemodialysisDocument2 pagesNursing Care Plan - HemodialysisjamieboyRN100% (2)
- Top Schools For May 2014 NLEDocument17 pagesTop Schools For May 2014 NLECoolbuster.NetNo ratings yet
- 2013 December Passers NURS1213seDocument220 pages2013 December Passers NURS1213seHarley Justiniani Dela CruzNo ratings yet
- List of Successful Examinees in The May 2014 Nurse Licensure ExaminationDocument225 pagesList of Successful Examinees in The May 2014 Nurse Licensure ExaminationofwwatchNo ratings yet
- December 2013 NLE Room Assignments - Legazpi CityDocument53 pagesDecember 2013 NLE Room Assignments - Legazpi CityjamieboyRNNo ratings yet
- PRC Program of Examination For The December 2013 Philippine Nursing Board Exam (NLE)Document2 pagesPRC Program of Examination For The December 2013 Philippine Nursing Board Exam (NLE)PhilippineNursingDirectory.comNo ratings yet
- December 2013 NLE Room Assignments - PampangaDocument40 pagesDecember 2013 NLE Room Assignments - PampangajamieboyRNNo ratings yet
- December 2013 NLE Room Assignments - Davao CityDocument150 pagesDecember 2013 NLE Room Assignments - Davao CityjamieboyRNNo ratings yet
- PRC Room Assignment For December 2013 Nursing Board Exam (Cebu)Document150 pagesPRC Room Assignment For December 2013 Nursing Board Exam (Cebu)PhilippineNursingDirectory.comNo ratings yet
- Dec 2013 NLE Rooms Cebu (Removal)Document1 pageDec 2013 NLE Rooms Cebu (Removal)Coolbuster.NetNo ratings yet
- PRC Room Assignment For December 2013 Nursing Board Exam (Cagayan de Oro)Document103 pagesPRC Room Assignment For December 2013 Nursing Board Exam (Cagayan de Oro)PhilippineNursingDirectory.comNo ratings yet
- December 2013 NLE Room Assignments - Examinees From Tacloban CityDocument22 pagesDecember 2013 NLE Room Assignments - Examinees From Tacloban CityjamieboyRNNo ratings yet
- December 2013 NLE Room Assignments - Iloilo CityDocument131 pagesDecember 2013 NLE Room Assignments - Iloilo CityjamieboyRNNo ratings yet
- December 2013 NLE Room Assignments - Zamboanga (Removal)Document1 pageDecember 2013 NLE Room Assignments - Zamboanga (Removal)jamieboyRNNo ratings yet
- PRC Room Assignment For December 2013 Nursing Board Exam - For Removals (Manila)Document1 pagePRC Room Assignment For December 2013 Nursing Board Exam - For Removals (Manila)PhilippineNursingDirectory.comNo ratings yet
- December 2013 NLE Room Assignments - ManilaDocument503 pagesDecember 2013 NLE Room Assignments - ManilajamieboyRNNo ratings yet
- DOH Nurse Deployment Project 2014 Application FormDocument1 pageDOH Nurse Deployment Project 2014 Application FormjamieboyRNNo ratings yet
- June 2013 NLE ResultsDocument325 pagesJune 2013 NLE ResultsjamieboyRNNo ratings yet
- PRC Room Assignment For December 2013 Nursing Board Exam (Tuguegarao)Document68 pagesPRC Room Assignment For December 2013 Nursing Board Exam (Tuguegarao)PhilippineNursingDirectory.comNo ratings yet
- June 2013 Pharmacist Board Exam Results - TopnotchersDocument1 pageJune 2013 Pharmacist Board Exam Results - TopnotchersjamieboyRNNo ratings yet
- December 2012 NLE Performance of SchoolsDocument21 pagesDecember 2012 NLE Performance of SchoolsjamieboyRNNo ratings yet
- June 2013 NLE Topnotchers and Top SchoolsDocument19 pagesJune 2013 NLE Topnotchers and Top SchoolsCoolbuster.NetNo ratings yet
- Guidelines Nurse Deployment Project 2014Document4 pagesGuidelines Nurse Deployment Project 2014jamieboyRNNo ratings yet
- PRC 2014 Exam ScheduleDocument7 pagesPRC 2014 Exam ScheduleCoolbuster.NetNo ratings yet
- December 2012 NLE CEBU Schedule of Registration & OathtakingDocument1 pageDecember 2012 NLE CEBU Schedule of Registration & OathtakingjamieboyRNNo ratings yet
- June 2013 Pharmacist Board Exam ResultsDocument28 pagesJune 2013 Pharmacist Board Exam ResultsjamieboyRN0% (1)
- June 2013 Pharmacist Board Exam Results - Performance of SchoolsDocument2 pagesJune 2013 Pharmacist Board Exam Results - Performance of SchoolsjamieboyRNNo ratings yet
- June 2013 NLE TopnotchersDocument3 pagesJune 2013 NLE TopnotchersNoypistuffNo ratings yet
- December 2012 NLE ResultsDocument339 pagesDecember 2012 NLE ResultsjamieboyRNNo ratings yet
- Case 10: Placenta Previa: ST ND RDDocument6 pagesCase 10: Placenta Previa: ST ND RDMengda ZhangNo ratings yet
- Useful AbbreviationsDocument2 pagesUseful AbbreviationsTracyNo ratings yet
- RA For Installation & Dismantling of Loading Platform A69Document8 pagesRA For Installation & Dismantling of Loading Platform A69Sajid ShahNo ratings yet
- 3a. Antisocial Personality DisorderDocument19 pages3a. Antisocial Personality DisorderspartanNo ratings yet
- Name: Ponce, Christian Neil P. Subject: CHN2 Course and Year: Bsn3 Block1. Code:N113Document3 pagesName: Ponce, Christian Neil P. Subject: CHN2 Course and Year: Bsn3 Block1. Code:N113Novelyn PuaNo ratings yet
- Uworld ENT NotesDocument4 pagesUworld ENT Notes808kailuaNo ratings yet
- Drug StudyDocument2 pagesDrug Studyunkown userNo ratings yet
- Maharishi Ayurveda - GlaserDocument21 pagesMaharishi Ayurveda - GlaserAMTRNo ratings yet
- rd-15 Bartholin Cyst and Abscess 10-12 PDFDocument2 pagesrd-15 Bartholin Cyst and Abscess 10-12 PDFdevidanthonyNo ratings yet
- Lesson 2 Progression and OverloadDocument2 pagesLesson 2 Progression and OverloadisaiacNo ratings yet
- Spindler 2021 CVDocument5 pagesSpindler 2021 CVapi-550398705No ratings yet
- Drug Education PaperDocument10 pagesDrug Education Paperapi-506661800No ratings yet
- Traumatic Brain InjuryDocument50 pagesTraumatic Brain InjuryDavide LeeNo ratings yet
- Records and ReportsDocument13 pagesRecords and ReportsBaishali DebNo ratings yet
- Exploring TheDocument20 pagesExploring TheMiroslava DjordjevicNo ratings yet
- Summer Training Project Report On EMPLOYEE MOTIVATION OF BHEL EMPLOYEESDocument81 pagesSummer Training Project Report On EMPLOYEE MOTIVATION OF BHEL EMPLOYEESrachitgarg7667% (3)
- Queen - My Melancholy Blues (Piano Sheet Music)Document27 pagesQueen - My Melancholy Blues (Piano Sheet Music)Kamil Iżykowski0% (3)
- RRLDocument12 pagesRRLEmilyne Joy Mendoza CabayaNo ratings yet
- Research PaperDocument10 pagesResearch PaperAyyat FatimaNo ratings yet
- Ocular Melanoma - Lex and TommyDocument16 pagesOcular Melanoma - Lex and Tommyapi-447472585No ratings yet
- Presentation 1Document11 pagesPresentation 1api-300463091No ratings yet
- 2022 December BlueprintDocument38 pages2022 December BlueprintNonoy JoyaNo ratings yet
- Health Education Feb. 23, 2024Document2 pagesHealth Education Feb. 23, 2024Ma. Jhysavil Arcena100% (1)
- Job Descriptions: Outreach Team Leader & Volunteer Trainer/ CoordinatorDocument7 pagesJob Descriptions: Outreach Team Leader & Volunteer Trainer/ CoordinatorJuan GallowayNo ratings yet
- Health Insurance in India-An Overview: K.Swathi, R.AnuradhaDocument4 pagesHealth Insurance in India-An Overview: K.Swathi, R.AnuradhaAnkit YadavNo ratings yet
- Immigrant WomanDocument58 pagesImmigrant WomanD. A.No ratings yet
- Increasing Height Through Diet, Exercise and Lifestyle AdjustmentDocument2 pagesIncreasing Height Through Diet, Exercise and Lifestyle AdjustmentEric KalavakuriNo ratings yet
- Types of Hospitals: Gynecology Services & Other Facilities Pharmacy LaboratoryDocument6 pagesTypes of Hospitals: Gynecology Services & Other Facilities Pharmacy LaboratoryMaham ShahidNo ratings yet
- DOH DILG Joint AO 2020-0001 On LIGTAS COVID and Community-Based Management of COVID-19Document44 pagesDOH DILG Joint AO 2020-0001 On LIGTAS COVID and Community-Based Management of COVID-19Albert DomingoNo ratings yet