Professional Documents
Culture Documents
Severe, Radiating Abdominal Pain and Near Syncope in An Elderly Man
Uploaded by
Azis KazeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Severe, Radiating Abdominal Pain and Near Syncope in An Elderly Man
Uploaded by
Azis KazeCopyright:
Available Formats
Severe, Radiating Abdominal Pain and Near Syncope in an Elderly Man An 85-year-old man is presented to the emergency department
(ED) by ambulance with severe abdominal pain that began suddenly 2 hours before presentation. The pain is mainly in his back and radiates toward his left inguinal region. The patient felt light-headed at the onset of the pain to the extent that he had to grip the sink to steady himself. He also reports significant nausea, although he has not vomited. He has no urinary symptoms. His medical history includes type 2 diabetes, hypertension, hyperlipidemia, ischemic heart disease, and intermittent claudication of his lower extremities. His medications include metformin, ramipril, simvastatin, aspirin, and a glyceryl trinitrate pump spray. He smoked 10-20 cigarettes a day for over 60 years but stopped 5 years ago. The physical examination reveals tenderness in the left iliac fossa and left costovertebral angle. His vital signs are remarkable for a heart rate of 105 beats/min and a blood pressure of 110/90 mm Hg. The patient is prescribed further analgesia and 1 L of colloid is administered. He is then referred to the surgical assessment unit (SAU) as a case of possible ureteric colic, with an abdominal radiograph taken during transit (Figure 1). On arrival to the SAU, the patient and his abdominal film are reviewed by the on-call surgical doctor. After assessment of his airway, breathing, circulation, level of consciousness, and exposure for examination of his abdomen, oxygen is given via a face mask, intravenous access is obtained at 2 sites, and a urinary catheter is inserted. Blood is drawn for laboratory analysis, including blood urea nitrogen, electrolytes, a full blood count, coagulation panel, and cross matching. The patient's electrolytes, complete blood cell count, and coagulation panel result are unremarkable. Arterial blood gas analysis is obtained and reveals a metabolic acidosis. Intravenous fluids are continued and the patient is sent for an urgent CT scan of the abdomen. Once completed, he is transferred by ambulance to a regional center for immediate intervention.
Discussion The CT scan revealed the presence of an abdominal aortic aneurysm (AAA) with a calcified wall and mural thrombus, with extraluminal blood indicating a rupture of the aneurysm (Figure 2). An aneurysm is defined as a focal increase in the diameter of a vessel to greater than 50% of normal; anything less is considered arteriomegaly. The abdominal aorta is approximately 2 cm in diameter, and an AAA is usually said to be present when a segment of aorta has a diameter of greater than 3 cm. AAA has a prevalence of 1.3%-8.9% in men and 1.0%-2.2% in women aged more than 55 years. It is responsible for 1%-3% of all deaths among men aged 65-85 years in developed countries. The incidence is higher in selected groups, with 5% of patients with coronary artery disease and up to 50% of those with popliteal or femoral artery aneurysms being found to have concomitant AAA. Recently published data from a 7-year prospective study of a cohort of 4345 patients, which identified 119 cases of AAA, has identified male
gender and increasing age as strong risk factors for the development of AAA. Another study demonstrated an association between short leukocyte telomere length and AAA, further supporting the notion that vascular biological aging is indeed an etiology of AAA. Smoking, hypertension, and hypercholesterolemia are also associated with a significantly increased risk for AAA. Interestingly, diabetes is usually protective against aneurysm formation. AAA may cause a variety of symptoms, including abdominal, back, and/or groin pain; however, the vast majority of AAAs is asymptomatic. Symptoms are usually a result of rapid aneurysm sac expansion or rupture. Pain may be mild to severe. A patient may present reporting a mass or swelling in the abdomen, or an awareness of the pulsation of the AAA. Complications of AAA include internal thrombosis, distal embolization, and aortoenteric fistula. AAA rupture is the most significant, immediate cause of mortality. Complaints of feeling light-headed or syncope, in association with back or abdominal pain, should alert the clinician to the possibility of AAA rupture. It is estimated that 50% of patients die soon after rupture, and of those surviving to surgery, the mortality is approximately 54%. The majority of early deaths result from free intraperitoneal rupture and exsanguination. Extraperitoneal rupture is associated with a more favorable course, as the bleeding may be temporarily tamponaded by peri-aortic tissue. Given the asymptomatic nature of most AAAs, as well as the dismal outcome after rupture, significant attention has been paid to screening for AAA. The first study to examine AAA screening across a large population was the MASS study. This study involved a population sample of 67,800 men aged 65-74 years of age, in which patients were randomly assigned to receive either screening ultrasonography or no intervention. Over 10 years, 155 deaths related to AAA occurred in the screening group vs 296 in the group which did not receive screening. This equates to a relative risk reduction of 48% (95% confidence interval 37%57%). This study also reported that the cost-effectiveness of such a screening program was favorable. A Cochrane review in 2007 found evidence of a significant reduction in mortality from AAA rupture in men aged 65-79 years who undergo screening. These findings have prompted the initiation of screening programs in several nations. For example, in the United Kingdom, the National Health Service (NHS) AAA screening program invites all men for a screening ultrasound in the year that they turn 65. Men over 65 who have not been screened or treated for AAA will be able to personally make a request for screening. So far, no study has demonstrated the cost-effectiveness of a similar screening program in women. In the United States, the SAAAVE Act allows for a AAA screening ultrasound in patients with a family history of AAA or a history of smoking more than 100 cigarettes, as long as they participate in their "Welcome to Medicare" physical examination within 6 months of turning 65. Multiple imaging modalities, including CT and ultrasonography, have been used to both screen and detail AAA. Three dimensional (3D) reconstruction CT (Orthogonal CT) provides a truly accurate model of aneurysm architecture. Angulation of the aneurysm can make traditional axial CT images misleading, and when ultrasound and CT are compared against orthogonal CT, ultrasound produces the most accurate estimation of size overall. Traditional CT can be used if the aorta cannot be visualized with ultrasound after repeated efforts.
Decision-making regarding operative management vs observation for AAA is informed mainly by the results of the UKSAT trial and the ADAM trial. The UKSAT randomized 1090 small aneurysms (4.0-5.5 cm) to operation or surveillance. No significant difference in overall mortality was demonstrated for those offered early surgery. Similar findings were found in the ADAM trial, and these 2 studies led to the recommendation that surgical repair should be considered in all aneurysms over 5.5 cm, while those patients with AAAs less than 5.5 cm should be enrolled on an ultrasonographic surveillance program. Surgical AAA repair should also be considered when the aneurysm expands by more than 0.6-0.8 cm in a single 12-month period. The threshold for surgical repair in women is typically 5.0 cm, given a relatively smaller normal aortic size compared with men. These recommendations are rooted in the physics of transmural pressure and the higher rupture rates associated with larger aneurysms. The law of LaPlace states that the tension in the wall of a sphere is proportional to the product of the transmural pressure across the wall and the radius of the sphere, and inversely proportional to the thickness of its wall; it can also be interpreted as stating that in a long pliable tube the site of largest diameter requires the least pressure to distend. This explains why an aneurysm tends to enlarge and why larger aneurysms rupture more frequently (it is because of the higher wall tension). As a result of the tendency of larger aneurysms to expand at a faster rate, AAAs of 4.5-5.4 cm in diameter will need 6-month ultrasound follow-up, and AAAs of 3-4.5 cm in diameter need yearly ultrasound follow-up; these intervals are practiced in the NHS (United Kingdom). Around 90% of detected aneurysms will be below the threshold of 5.5 cm required for intervention and will undergo surveillance to monitor expansion into the interventional range. A number of approaches designed to limit expansion have been suggested. Large studies have indicated that propranolol does not inhibit aneurysm expansion. A number of studies agree that tobacco use is associated with an increased rate of aneurysm expansion. Level B and C evidence is available to suggest that 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors (statins) may inhibit aneurysm expansion. There are animal data but no human data demonstrating that angiotensin-converting enzyme inhibitors or losartan, an angiotensin receptor blocker, will decrease the rate of AAA expansion, when used to treat concomitant hypertension. Optimizing glycemic control is also associated with a reduction in the rate of expansion of AAA in diabetic patients. It seems prudent that weight loss, regular exercise if possible, and a healthy diet should also be encouraged. Open surgical repair or endovascular aneurysm repair (EVAR) are the current operative options available. EVAR is a less-invasive approach to addressing AAA. EVAR involves transluminal placement of a modular stent-graft system into the AAA via remote arterial access (usually, the femoral artery) under local, regional, or, most commonly, general anesthetic. Concerns about the proximity of the renal arteries and other vessels to the aneurysm have been overcome by the use of fenestrated grafts. However, the proximal neck of the aneurysm is considered unfavorable anatomically for EVAR if 1 or more of the following situations exist: angulation > 60, diameter > 30 mm, short length < 15 mm, conical shape, and extensive thrombus or calcification. In addition, surgical access through the femoral vessels in the groin can be difficult in the setting of extensive iliac artery occlusive disease or vessel tortuosity, thereby limiting the applicability of this procedure in some patients or requiring the use of adjunctive, open surgical, or endovascular techniques to gain access to the aorta.
The EVAR 1 trial randomly assigned 1082 elective patients (patients from multiple centers that were also fit for open repair) to either open repair or EVAR. The 30-day operative mortality was 1.6% in the EVAR group and 4.6% in the open-repair group. However, EVAR patients were at a significantly higher risk for graft complication (hazard ratio [HR], 4.39) and graft-related intervention (HR, 2.86) during follow-up; there was no difference in all-cause or aneurysm-related mortality after 8 years of follow-up between the groups, with the initial benefit from EVAR erased in long-term follow-up. Since the study, there has been a steady increase in the proportion of EVAR compared with open repair performed in the United Kingdom (from 28% in 2000 to 57% in 2006) and elsewhere. The EVAR 2 trial randomly assigned 338 patients (from 1999 to 2003) aged over 60 years with at least 5.5-cm aneurysms who were unfit for open repair to no intervention or EVAR. This study demonstrated a considerable 30-day mortality (9%) in those treated with EVAR compared with no intervention, and showed no significant difference between the EVAR group and the no intervention group for all-cause mortality (HR, 1.21). These findings are in contrast with a number of more recent studies, which claim that there are appreciable long-term benefits from EVAR in patients unfit for surgery, at a cost of a small 30-day mortality rate of between 1.6% and 2.9%. Some of the longer benefit may be due to a statistically higher rate of antiplatelet and statin prescription in the newer studies, as well as the increased expertise available in higher-volume centers, and newer-generation grafts. The Cronenwett model suggests that patients with AAAs > 5.5 cm with low operative risk and poor anatomic suitability for EVAR who are less than 70 years should have open repair, and those at high risk operatively with excellent anatomy for EVAR and who are older than 70 years should have EVAR. These two extreme examples seem obvious, and many patients will fall between the two; informed patient preference and local expertise will influence the final treatment in such cases. The Society for Vascular Surgery practice guidelines for the Care of Patients with AAA include specific recommendations for surveillance following repair, as follows: Surveillance during the first year post surgery should include CT angiography at 1 month and 12 months. If no endoleak or AAA enlargement is documented after the first year, color duplex ultrasound is suggested as an alternative to CT imaging for annual postoperative surveillance of EVAR. Color duplex ultrasonography and a noncontrast CT scan are recommended as a substitute for CT angiography for post-EVAR surveillance of patients with renal insufficiency. Noncontrast CT scanning of the entire aorta is recommended at 5-year intervals after open surgical repair or EVAR. Open repair of AAA is of proven durability with a 36-year population-based study confirming that the vast majority of patients (91.6%) remain free of any significant graftrelated complication during their remaining lifetime. The noted complications included anastomotic pseudoaneurysm, graft thrombosis, graft enteric erosion/fistula, graft infection, anastomotic hemorrhage, colonic ischemia, and atheroembolism. Two point six percent of patient complications were recognized within 30 days of the procedure, and the later complications were noted at a median of 6.1 years. Clinical and radiologic follow-up should be geared to recognize these complications and should follow the recommendations detailed by such bodies as the Society for Vascular Surgery. As noted previously, persons
with AAA are at risk for synchronous and metachronous aneurysm elsewhere, and followup should take this into account. EVAR does not have the risks of anastomotic pseudoaneurysm, anastomotic hemorrhage, but it does have those of graft migration and endoleak in addition to the other risks. Endoleak describes the situation of incomplete isolation of the aneurysm sack by the graft, leading to continued flow and pressurization of the sac. Again, follow-up should be planned according to the recommendations for detecting these complications. Emergency repair of ruptured or leaking aneurysms can be performed with EVAR if anatomic conditions are optimal and the patients hemodynamic status allows; if not, open repair should be used as proximal aortic control can be obtained swiftly. If these conditions are met, data suggest benefits for such patients undergoing EVAR, such as a reduction in the mortality, prolonged intensive care requirement and total hospital stay compared with open repair. Highly symptomatic but unruptured aneurysms can be managed with EVAR and open repair in the same manner as asymptomatic aneurysms (but on a more urgent basis), the threshold is often less than 5.5 cm for repair in these cases.
1. You are examining a patient with a known AAA. At the most recent visit, the AAA seems to have expanded. At what size should an asymptomatic AAA cease being under surveillance and be considered for repair? Answer: > 5.5 cm The UKSAT and the ADAM trials led to the practice that aneurysms less than 5.5 cm are surveyed with ultrasound and those larger than 5.5 cm are repaired. The NHS screening program surveys AAAs of 3-4.4 cm yearly and those between 4.5 cm and 5.5 cm biannually. The normal aorta is around 2 cm in diameter, and it is considered aneurysmal when more than 3 cm.
2. You are considering management options for a patient with an AAA requiring surgical intervention. What complication of EVAR is not commonly seen in open repair of AAA? Answer: Endoleak The term endoleak describes when a graft fails to isolate the aneurysm sac, leading to continued pressurization and aneurysm sac expansion. Type I endoleak occurs at the proximal or distal edge of the endograft, if the proximal or distal seal zones between the stent-graft and blood vessel wall are not adequate. Type II endoleak results from a blood vessel that is filling the original aneurysm sac in a retrograde fashion. Type III endoleak results from a leak between overlapping, modular components of a stent-graft system. Type IV endoleak is very similar to type III endoleak, in that it results from blood flowing from within the endograft through the stent, but this time it results from a flaw in the graft material itself. Type V endoleaks have been described as being due to "endotension" with an enlarging aneurysm sac without a visible endoleak, which can be dealt with by reinforcing the indwelling stent graft or re-lining the graft.
You might also like
- Cardiology PDFDocument8 pagesCardiology PDFTran Chi TienNo ratings yet
- AAFP Board Review ClinchersDocument53 pagesAAFP Board Review ClinchersJessica E Isom100% (2)
- Clinical Surgery Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2From EverandClinical Surgery Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2No ratings yet
- Coronary Atery Disease-Htn-Thrombo QuestionsDocument38 pagesCoronary Atery Disease-Htn-Thrombo Questionssrivari sriniNo ratings yet
- A Clinician's Guide To Nuclear MedicineDocument409 pagesA Clinician's Guide To Nuclear Medicineayodeji7886% (7)
- Abdominal Aortic AneurysmDocument44 pagesAbdominal Aortic AneurysmAkhilMuraleedharan100% (2)
- Question 1 of 10: AAFP Board Review Clinchers Cardio Quiz 1Document60 pagesQuestion 1 of 10: AAFP Board Review Clinchers Cardio Quiz 1pramesh1No ratings yet
- Abdominal Aortic AneurysmDocument20 pagesAbdominal Aortic AneurysmPortia Rose RodriguezNo ratings yet
- Detailed Lesson Plan in Science 5 1st QuarterDocument8 pagesDetailed Lesson Plan in Science 5 1st QuarterAndrewNo ratings yet
- Emergency MedicineDocument150 pagesEmergency MedicineDev MartelNo ratings yet
- Hypertension LecturesDocument65 pagesHypertension LecturesAdebisiNo ratings yet
- Abdominal Aortic AneurysmDocument37 pagesAbdominal Aortic Aneurysmannu300No ratings yet
- Complementary and Alternative Medical Lab Testing Part 3: CardiologyFrom EverandComplementary and Alternative Medical Lab Testing Part 3: CardiologyRating: 1 out of 5 stars1/5 (1)
- Cardiac surgery 5th year 2017-محلولDocument11 pagesCardiac surgery 5th year 2017-محلولIbrahim BarhamNo ratings yet
- Ultrasound Imaging of The AbdomenDocument224 pagesUltrasound Imaging of The AbdomenAsztalos Attila100% (9)
- Thyroid Encyclopedia: Encyclopedia of Thyroid Disease, Thyroid Conditions and Thyroid CancerFrom EverandThyroid Encyclopedia: Encyclopedia of Thyroid Disease, Thyroid Conditions and Thyroid CancerNo ratings yet
- Abdominal Aortic Aneurysms Nejm 2014Document8 pagesAbdominal Aortic Aneurysms Nejm 2014api-236974953No ratings yet
- Abdominal Aortic AneurysmDocument7 pagesAbdominal Aortic AneurysmLuke MaciasNo ratings yet
- Chi Ru RgicalDocument10 pagesChi Ru RgicalRamona SturzuNo ratings yet
- AAA Aafp 2015Document6 pagesAAA Aafp 2015Leonardo MedinaNo ratings yet
- AAA Screening - Spanos 2017Document3 pagesAAA Screening - Spanos 2017Vlad NeagoeNo ratings yet
- Abdominal Aortic Aneurysms: Clinical PracticeDocument8 pagesAbdominal Aortic Aneurysms: Clinical PracticeCristian C BecerraNo ratings yet
- Estenosis Aortica 2016 Aafp 2016Document8 pagesEstenosis Aortica 2016 Aafp 2016Antonio MoncadaNo ratings yet
- Dissertation Abdominal Aortic AneurysmDocument6 pagesDissertation Abdominal Aortic AneurysmBuyThesisPaperCanada100% (1)
- Vascular Emergencies: Susan L. Drinkwater, Vikas A. Pandey, and Alun H. DaviesDocument17 pagesVascular Emergencies: Susan L. Drinkwater, Vikas A. Pandey, and Alun H. DaviesHarshpreet KaurNo ratings yet
- $grand Case Super RevisionDocument51 pages$grand Case Super RevisionweenaNo ratings yet
- Application Brief: Abdominal Aortic AneurysmDocument6 pagesApplication Brief: Abdominal Aortic AneurysmVisualSonicsNo ratings yet
- Abdominal Aortic AneurysmDocument4 pagesAbdominal Aortic Aneurysmgian_piliNo ratings yet
- Abdominal Aortic AneurysmDocument44 pagesAbdominal Aortic Aneurysmalebelucci69No ratings yet
- 26 2 KatzDocument2 pages26 2 KatznoemaraleNo ratings yet
- Introduction of Case Study BristyDocument11 pagesIntroduction of Case Study BristyJoy Chakraborty RoniNo ratings yet
- Managment or Aortic Abdominal Aneurysm NEJMDocument9 pagesManagment or Aortic Abdominal Aneurysm NEJMJohn MolinaNo ratings yet
- Diagnosis and Management of Splanchnic Ischemia: Ioannis E Koutroubakis, MD, PHD, Assistant Professor of MedicineDocument12 pagesDiagnosis and Management of Splanchnic Ischemia: Ioannis E Koutroubakis, MD, PHD, Assistant Professor of MedicineIgorCotagaNo ratings yet
- Abdominal Pain in Elderly PersonsDocument14 pagesAbdominal Pain in Elderly PersonsamirunNo ratings yet
- Screening Guidelines and Treatment Options For Abdominal Aortic AneurysmsDocument36 pagesScreening Guidelines and Treatment Options For Abdominal Aortic AneurysmsmazriyahyaNo ratings yet
- Lectura 8Document8 pagesLectura 8Daniela Andrea Tello GuaguaNo ratings yet
- American College of Surgeons (ACS)Document8 pagesAmerican College of Surgeons (ACS)perkakas78No ratings yet
- Chronic Mesenteric Ischemia: Open Surgery Versus Percutaneous Angioplasty and StentingDocument9 pagesChronic Mesenteric Ischemia: Open Surgery Versus Percutaneous Angioplasty and StentingIgorCotagaNo ratings yet
- Avoiding Revascularization With Lifestyle Changes: The Multicenter Lifestyle Demonstration ProjectDocument5 pagesAvoiding Revascularization With Lifestyle Changes: The Multicenter Lifestyle Demonstration ProjectNag Mallesh RaoNo ratings yet
- Abdominal Aortic Aneurysm: Gilbert R. Upchurch, JR., M.D., and Timothy A. Schaub, M.DDocument7 pagesAbdominal Aortic Aneurysm: Gilbert R. Upchurch, JR., M.D., and Timothy A. Schaub, M.DleesaNo ratings yet
- Death Case II DizaDocument29 pagesDeath Case II DizaJayarasti KusumanegaraNo ratings yet
- Ruptured Abdominal Aortic Aneurysm Identified On Point-Of-Care Ultrasound in The Emergency DepartmentDocument3 pagesRuptured Abdominal Aortic Aneurysm Identified On Point-Of-Care Ultrasound in The Emergency DepartmentRachmadityaa PancaraniNo ratings yet
- Abdominal Aortic AneurysmDocument9 pagesAbdominal Aortic AneurysmIlyes FerenczNo ratings yet
- Screening Program of AaaDocument7 pagesScreening Program of AaaShaastieNo ratings yet
- AASLD Practice Guidelines For Ascites in CirrhosisDocument9 pagesAASLD Practice Guidelines For Ascites in CirrhosisSalman AlfathNo ratings yet
- Management of Abdominal Aortic AneurysmsDocument9 pagesManagement of Abdominal Aortic Aneurysmspogesil46No ratings yet
- Abdominal Aortic Aneurysm: A Comprehensive ReviewDocument5 pagesAbdominal Aortic Aneurysm: A Comprehensive Reviewnico rifandhaNo ratings yet
- Aortic Aneurysm-Dr AbhishekDocument90 pagesAortic Aneurysm-Dr Abhisheksarath chandranNo ratings yet
- Surgery FINAL 2023Document140 pagesSurgery FINAL 2023TayaNo ratings yet
- Dream Trial Journal PresentationDocument30 pagesDream Trial Journal PresentationRam Kumar ShresthaNo ratings yet
- Case Alcohol Abuse and Unusual Abdominal Pain in A 49-Year-OldDocument7 pagesCase Alcohol Abuse and Unusual Abdominal Pain in A 49-Year-OldPutri AmeliaNo ratings yet
- Seminar AaaDocument13 pagesSeminar AaaShaastieNo ratings yet
- Peripheral Artery Disease: Clinical PracticeDocument11 pagesPeripheral Artery Disease: Clinical Practiceapi-311409998No ratings yet
- Epidemiological Aspects On Abdominal Aortic Aneurysms (AAA)Document17 pagesEpidemiological Aspects On Abdominal Aortic Aneurysms (AAA)Janey Ceniza تNo ratings yet
- Upper GI BleedDocument8 pagesUpper GI BleedbbyesNo ratings yet
- JURNALDocument7 pagesJURNALHarlina NurlitaNo ratings yet
- Step by Step: Clinical Problem-SolvingDocument5 pagesStep by Step: Clinical Problem-SolvingMirin ApuniusNo ratings yet
- Liver Abscess DissertationDocument4 pagesLiver Abscess DissertationPayForAPaperAtlanta100% (1)
- Aortoiliac DiseaseDocument110 pagesAortoiliac DiseaseAmr AbdelghaffarNo ratings yet
- Blunt Abdominal InjuryDocument6 pagesBlunt Abdominal InjuryPeter KayNo ratings yet
- Joseph 2016 CardioDocument30 pagesJoseph 2016 CardioCarlos Daniel da Silva AlonsoNo ratings yet
- ChangDocument3 pagesChangAmirullah AbdiNo ratings yet
- Abdominal Aortic Aneurysm: History & ExamDocument47 pagesAbdominal Aortic Aneurysm: History & ExamMicija CucuNo ratings yet
- United European Gastroenterology Journal 2014 Sonnenberg 5 9Document5 pagesUnited European Gastroenterology Journal 2014 Sonnenberg 5 9Ricardo MarquezNo ratings yet
- Endoscopy in The ElderlyDocument7 pagesEndoscopy in The ElderlyFebyan AbotNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 4: VascularFrom EverandComplementary and Alternative Medical Lab Testing Part 4: VascularNo ratings yet
- 010 Physiology MCQ ACEM Primary CardiovascularDocument9 pages010 Physiology MCQ ACEM Primary Cardiovasculargaurav mittalNo ratings yet
- Basic Principle, Operation and Maintenance: Aqeel Ahmed KhanDocument18 pagesBasic Principle, Operation and Maintenance: Aqeel Ahmed KhanchanlalNo ratings yet
- Coronary Artery Disease (Metabilism)Document137 pagesCoronary Artery Disease (Metabilism)Al-nazer Azer AlNo ratings yet
- The Heart and Blood Vessels WorksheetDocument3 pagesThe Heart and Blood Vessels WorksheetGeorgia SimmsNo ratings yet
- DynaMed Plus - Stroke (Acute Management)Document126 pagesDynaMed Plus - Stroke (Acute Management)Sarah Shafa MarwadhaniNo ratings yet
- BMC Pediatrics Rheumatic FeverDocument15 pagesBMC Pediatrics Rheumatic FeverMobin Ur Rehman KhanNo ratings yet
- PalpitationsDocument3 pagesPalpitationsJessica Febrina WuisanNo ratings yet
- Question BankDocument6 pagesQuestion Bankkoang lual gachNo ratings yet
- Sp088influence of Telmisartan and Amlodipine Combi PDFDocument3 pagesSp088influence of Telmisartan and Amlodipine Combi PDFKumarsai DurusojuNo ratings yet
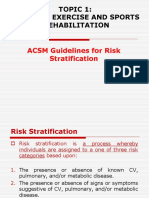
- Chapter 1.2 Algorithym of Risk StratificationDocument26 pagesChapter 1.2 Algorithym of Risk StratificationMUHAMMAD DANISH AMIN BIN BORHANUDDINNo ratings yet
- Unlicensed-A-V Fistula CareDocument29 pagesUnlicensed-A-V Fistula CareMuhammad HaneefNo ratings yet
- CPRDocument1 pageCPRjanet roosevelt100% (1)
- 1.4 The Lymphatic SystemDocument10 pages1.4 The Lymphatic SystemFerguson TehNo ratings yet
- How To Write A Proposal EssayDocument3 pagesHow To Write A Proposal Essaypilav0wutyk3100% (2)
- Vasopressor Use in Adult Patients: Nadia Ferguson-Myrthil, PharmdDocument6 pagesVasopressor Use in Adult Patients: Nadia Ferguson-Myrthil, PharmdWILLIAM RICARDO CASTAÑEDA VARGASNo ratings yet
- Cardiac Arrhythmias I: Atrioventricular Conduction Disturbances and BradyarrhythmiasDocument73 pagesCardiac Arrhythmias I: Atrioventricular Conduction Disturbances and Bradyarrhythmiasiman firmansyahNo ratings yet
- Entresto Marketing PlanDocument1 pageEntresto Marketing PlanSalmanAhmedNo ratings yet
- Naccarelli 2012 Electrocardiography of Arrhythmias A Comprehensive ReviewDocument1 pageNaccarelli 2012 Electrocardiography of Arrhythmias A Comprehensive Reviewraul gutierrezNo ratings yet
- Eur J Echocardiogr 2010 Walker E37Document4 pagesEur J Echocardiogr 2010 Walker E37Muhammad Haryadi AdeNo ratings yet
- Venous Stasis and ElephantaitisDocument3 pagesVenous Stasis and ElephantaitismcwnotesNo ratings yet
- Central Venous CatheterizationDocument20 pagesCentral Venous Catheterizationdrhiwaomer100% (3)
- Monitoreo Hemodinamico FuncionalDocument27 pagesMonitoreo Hemodinamico FuncionalGabriel Lopez MNo ratings yet
- 232781-2019-Bright Maritime Corp. v. RacelaDocument19 pages232781-2019-Bright Maritime Corp. v. RacelaAnne AjednemNo ratings yet