Professional Documents
Culture Documents
Nej M CPC 0900640
Uploaded by
Carolina Polo TorresOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nej M CPC 0900640
Uploaded by
Carolina Polo TorresCopyright:
Available Formats
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
case records of the massachusetts general hospital
Founded by Richard C. Cabot Nancy Lee Harris, m.d., Editor Eric S. Rosenberg, m.d., Associate Editor Jo-Anne O. Shepard, m.d., Associate Editor Alice M. Cort, m.d., Associate Editor Sally H. Ebeling, Assistant Editor Christine C. Peters, Assistant Editor
Case 23-2009: A 13-Year-Old Boy with Headache, Nausea, Seizures, and Hypertension
Michael J.G. Somers, M.D., Amita Sharma, M.D., P. Ellen Grant, M.D., Alexander R. Guimaraes, M.D., Ph.D., and Eveline E. Schneeberger, M.D.
Pr e sen tat ion of C a se
A 13-year-old boy was admitted to the hospital because of headache, nausea, seizures, renal failure, and hypertension. The patient had been well until approximately 3 weeks earlier, when intermittent left-sided headaches and fatigue developed, followed by nasal congestion and anorexia. He began to nap daily after school. During the week before admission, nausea and vomiting occurred approximately every other day. Five days before admission, facial and periorbital swelling developed. He saw his primary care physician. A test for streptococcal pharyngitis was reportedly negative; amoxicillin was prescribed for presumed sinusitis. He continued to feel unwell and was not as energetic as usual, although he was able to play lacrosse 3 days before admission. He reported constipation and mild epigastric and periumbilical abdominal pain, he vomited intermittently, and he slept much of the day. On the morning of admission, nausea, vomiting, and abdominal pain developed while the patient was at school. At 11:15 a.m., his mother took him to the doctors office. Blood was drawn for laboratory tests, and he was sent to another hospital for a radiograph of his abdomen. En route to the car, at approximately noon, he reported numbness of the right leg and dizziness, and he became disoriented, with difficulty walking and coordinating his legs, but with no clear weakness; the episode lasted 5 minutes. During the car ride, he returned to his baseline mental status; numbness of the right leg persisted. At the hospital, radiography was performed, laboratory-test results revealed azotemia, and he was referred to the emergency department of another hospital. He began vomiting. On examination in the emergency department, the patient was awake, oriented, and vomiting intermittently. The blood pressure was 170/120 mm Hg, the pulse 63 beats per minute, the temperature 37C, the respiratory rate 16 breaths per minute, the oxygen saturation 98% while he was breathing ambient air, and the weight 45.5 kg. The skin was pale and facial edema was present; the remainder of the examination was normal. Laboratory-test results are shown in Table 1. Screening tests for mononucleosis and hepatitis A, B, and C were negative. Labetalol and
n engl j med 361;4 nejm.org july 23, 2009
From the Division of Nephrology, Childrens Hospital (M.J.G.S.); the Departments of Pediatrics (A.S.), Radiology (P.E.G., A.R.G.), and Pathology (E.E.S.), Massachusetts General Hospital; and the Departments of Pediatrics (M.J.G.S., A.S.), Radiology (P.E.G., A.R.G.), and Pathology (E.E.S.), Harvard Medical School all in Boston.
N Engl J Med 2009;361:389-400.
Copyright 2009 Massachusetts Medical Society.
389
The New England Journal of Medicine Downloaded from nejm.org on September 22, 2012. For personal use only. No other uses without permission. Copyright 2009 Massachusetts Medical Society. All rights reserved.
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
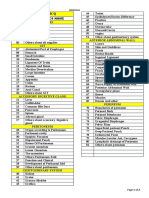
Table 1. Hematologic and Biochemical Laboratory Data.* Variable Hematocrit (%) Hemoglobin (g/dl) Red cells (per mm3) White cells (per mm3) Platelets (per mm3) Mean corpuscular volume (m3) Mean corpuscular hemoglobin (pg/red cell) Mean corpuscular hemoglobin concentration (g/dl) Red-cell distribution width (%) Erythrocyte sedimentation rate (mm/hr) Activated partial-thromboplastin time (sec) Prothrombin time (sec) International normalized ratio Sodium (mmol/liter) Potassium (mmol/liter) Chloride (mmol/liter) Carbon dioxide (mmol/liter) Urea nitrogen (mg/dl) Creatinine (mg/dl) Glucose (mg/dl) Bilirubin (mg/dl) Total Direct Protein (g/dl) Total Albumin Globulin Phosphorus (mg/dl) Magnesium (mmol/liter) Calcium (mg/dl) Parathyroid hormone (pg/ml) Alkaline phosphatase (U/liter) Aspartate aminotransferase (U/liter) Alanine aminotransferase (U/liter) Lactate dehydrogenase (U/liter) Lipase (U/dl) Amylase (U/liter) Troponin I (ng/ml) Thyrotropin (IU/ml) Thyroxine, free (ng/dl) 1.36.0 3100 0.00.4 6.08.3 3.35.0 2.64.1 3.04.5 0.71.0 8.510.5 1060 15350 1040 1055 193 (ref 30300) 32 20 701 (ref 95180) 2.5 166 (ref 25125) 0.02 4.86 (ref 0.283.89) 0.71 (ref 0.581.64) 1.1 8.4 5.9 3.3 2.6 6.3 1.1 8.2 458 181 24 15 0.01.0 0.00.4 1.4 (ref 0.31.2) 1.6 0.4 135145 3.44.8 100108 23.031.9 825 0.61.5 70110 Reference Range, Age-Adjusted 37.049.0 13.016.0 4,500,0005,300,000 450013,500 150,000450,000 7898 25.035.0 31.037.0 11.514.5 017 (men) 22.134.0 10.313.2 23.6 (ref 25.039.0) 10.4 1.0 134 5.4 95 21 134 15.6 102 16.2 6,000 127,000 86.7 Day of Admission, Other Hospital 26.9 9.7 On Admission, This Hospital 24.5 9.3 2,910,000 8,100 114,000 84 32.1 38.0 15.8 48 32.6 14.2 1.3 134 6.4 (specimen not hemolyzed) 96 19.0 123 16.1 110
390
n engl j med 361;4
nejm.org
july 23, 2009
The New England Journal of Medicine Downloaded from nejm.org on September 22, 2012. For personal use only. No other uses without permission. Copyright 2009 Massachusetts Medical Society. All rights reserved.
case records of the massachusetts gener al hospital
Table 1. (Continued.) Variable Iron (g/dl) Iron-binding capacity (g/dl) Ferritin (ng/ml) 25-Hydroxyvitamin D (ng/ml) Thiocyanate (g/ml) Reference Range, Age-Adjusted 45160 228428 30300 >32, desired Unexposed nonsmokers, 1.04.0; unexposed smokers, 3.012.0 Day of Admission, Other Hospital On Admission, This Hospital 103 204 279 26 5.1
Arterial blood gas analysis Base excess (mmol/liter) pH Partial pressure of carbon dioxide (mm Hg) Partial pressure of oxygen (mm Hg) Bicarbonate (mmol/liter) 7.357.45 3542 80100 2430 Negative 1.6 7.48 29 120 22
* Ref denotes reference range. To convert the values for urea nitrogen to millimoles per liter, multiply by 0.357. To convert the values for creatinine to micromoles per liter, multiply by 88.4. To convert the values for glucose to millimoles per liter, multiply by 0.05551. To convert the values for phosphorus to millimoles per liter, multiply by 0.3229. To convert the values for magnesium to milligrams per deciliter, divide by 0.4114. To convert the values for calcium to millimoles per liter, multiply by 0.250. Reference values are affected by many variables, including the patient population and the laboratory methods used. The ranges used at Massachusetts General Hospital are age-adjusted for patients who are not pregnant and do not have medical conditions that could affect the results. They may therefore not be appropriate for all patients. The composition of the patients inspired gas was not reported.
ondansetron were administered, and the blood pressure decreased to 132/83 mm Hg. Computed tomography (CT) of the head showed a small, ill-defined focus of decreased density in the right parietal region and no other evidence of focal or diffuse lesions, hemorrhage, hydrocephalus, or focal bone lesions. After the CT scan, at approximately 3 p.m. and 4 p.m., he had two episodes of blank staring, one associated with incontinence, without shaking or body movement. After the episodes, he was somnolent but oriented. His mental status returned to normal after he slept. There was minimal urine output. He was transferred to the pediatric intensive care unit of this hospital. He did not have sore throat, rash, arthralgias, arthritis, myalgias, photosensitivity, epistaxis, hemoptysis, shortness of breath, hematuria, or fever. He had been born via vaginal delivery after a fullterm gestation. At 3 weeks of age, he required surgery for pyloric stenosis. One year before admission, on routine examination, the blood pressure was 100/70 mm Hg and pubertal development had begun. He had received all immunizations and took no medications. He had no aln engl j med 361;4
lergies. He lived with his parents and brothers, who were healthy. Both grandfathers had had prostate cancer, and there was a family history of migraine headaches. There was no family history of an autoimmune disorder. On examination, the patient was intermittently somnolent but arousable and oriented. The weight was 45 kg and the blood pressure ranged between 150/60 and 170/115 mm Hg; the pulse was 80 beats per minute, the temperature 36.5C, the respiratory rate between 10 and 20 breaths per minute, and the oxygen saturation 93 to 98% while he was breathing ambient air. The physical examination was unchanged. Laboratory-test results are shown in Tables 1 and 2. Specimens of blood and urine were cultured. The electrocardiogram showed normal sinus rhythm with no peaked T waves. CT images from the other hospital were reviewed, and they were thought to show asymmetric ventricles, with the occipital horn of the lateral ventricle larger on the left side than on the right, a prominent temporal horn, and a normal third ventricle, and no evidence of acute stroke or hemorrhage. Radiographs of the chest and abdomen
july 23, 2009
nejm.org
391
The New England Journal of Medicine Downloaded from nejm.org on September 22, 2012. For personal use only. No other uses without permission. Copyright 2009 Massachusetts Medical Society. All rights reserved.
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
Table 2. Results of Urinalysis.* Analyte Sodium (mmol/liter) Potassium (mmol/liter) Chloride (mmol/liter) Urea nitrogen (mg/dl) Creatinine (mg/ml) Calcium (mg/dl) Glucose (g/dl) Color Turbidity pH Specific gravity Screening dipstick White cells Bilirubin Urobilinogen Nitrites Albumin Glucose Ketones Blood Leukoesterase Urine sediment Hyaline casts (per low-power field) Granular casts (per low-power field) Red cells (per high-power field) White cells (per high-power field) Squamous epithelial cells (per highpower field) Bacteria (per high-power field) Budding yeast (per high-power field) 02 02 Negative Negative Few 05 4 4 94 15 50100 510 Negative Few 02 Negative Negative Negative Negative Negative Negative Negative Negative Negative Negative Normal (ref normal) Negative 4+ Negative Negative 3+ Negative 1+ 1+ Negative Negative 3+ Trace Trace 3+ Reference Range, Age-Adjusted Diet-dependent Diet-dependent Diet-dependent Diet-dependent Diet-dependent Diet-dependent <0.05 Yellow Clear 5.09.0 1.0011.035 Yellow Hazy 6.5 1.025 Day of Admission, Other Hospital On Admission, This Hospital 38 68.8 49 275 1.83 2.7 Negative Yellow Turbid 5.5 1.031
* Ref denotes reference range. To convert the value for urea nitrogen to millimoles per liter, multiply by 0.357. To convert the value for creatinine to micromoles per liter, multiply by 8840. To convert the value for calcium to millimoles per liter, multiply by 0.250. To convert the value for glucose to millimoles per liter, multiply by 55.51. Reference values are affected by many variables, including the patient population and the laboratory methods used. The ranges used at Massachusetts General Hospital are age-adjusted for patients who are not pregnant and do not have medical conditions that could affect the results. They may therefore not be appropriate for all patients.
revealed increased perihilar markings with a butterfly pattern of vasculature suggestive of mild congestive heart failure and a moderate amount of stool in the colon with a nonobstructive gas pattern; they were otherwise normal. Analysis of the urine sediment by a nephrologist revealed red-cell, mixed-cellular, granular,
392
n engl j med 361;4
and waxy casts. An arterial catheter was inserted, and a continuous intravenous infusion of nitroprusside was begun, with a goal of systolic pressures below 140 mm Hg. Labetalol and ondansetron were continued, and hydralazine, calcium gluconate, insulin, and dextrose were given intravenously. Emergency hemodialysis was perjuly 23, 2009
nejm.org
The New England Journal of Medicine Downloaded from nejm.org on September 22, 2012. For personal use only. No other uses without permission. Copyright 2009 Massachusetts Medical Society. All rights reserved.
case records of the massachusetts gener al hospital
formed. Fluid was restricted to 1 liter per day, and methylprednisolone and ranitidine were begun. Mannitol, midazolam, and fentanyl citrate were added. Magnesium was administered as needed to maintain a level greater than 1.0 mmol per liter. Indirect immunofluorescence testing for antineutrophil cytoplasmic antibodies (ANCAs) and antiglomerular basement membrane antibodies was negative. On the second hospital day, tests for lupus anticoagulant were negative, and levels of IgG and IgM anticardiolipin antibodies were normal. Ultrasonography of the kidney revealed mildly increased echogenicity of the renal parenchyma, most marked in the upper pole of the left kidney, moderate free fluid in the pelvis, and no hydronephrosis or solid-appearing mass lesions. The right kidney was 9.4 cm in length and the left kidney 10.3 cm in length. Cultures of the blood and urine were sterile. On the third day, analysis of a specimen of urine revealed a protein level of 27,280 mg per liter (reference range, 0 to 135) and a creatinine level of 2.3 mg per milliliter (20,332 mol per liter). Magnetic resonance imaging (MRI) of the brain showed areas of increased T2-weighted signal intensity in the subcortical white matter in the frontal, parietal, and occipital regions, with a predominantly normal signal on diffusionweighted imaging. A diagnostic procedure was performed.
frontal, parietal, and occipital regions, corresponding to areas of low attenuation seen on CT, which appear to represent increased fluid in the subcortical white-matter region, with very little mass effect. These areas were bright on both T2-weighted (Fig. 1C) and fluid-attenuated inversion recovery images (Fig. 1D). On diffusion-weighted imaging, most of the T2-weighted bright areas had normal signal intensity, which indicated that they represented edema, with only small areas of increased signal on diffusion-weighted imaging, which suggested necrosis. Dr. Somers: This child presented with hematuria and proteinuria, severe azotemia, and oliguria leading to volume overload. This constellation of findings constitutes a nephritic pattern of renal disease. The analysis of urine sediment supports this pattern of kidney injury, with dysmorphic erythrocytes, pyuria, and cellular and granular casts. The marked renal insufficiency and hypertension and the accompanying proteinuria make diffuse glomerular involvement likely.
Duration of kidney insufficiency
Differ en t i a l Di agnosis
Dr. Michael J.G. Somers: May we review the radiology studies? Dr. Alexander R. Guimaraes: A chest film on admission showed clear lungs, normal heart size, and a mild increase in interstitial opacities, features compatible with mild congestive heart failure. There were no pleural effusions. An abdominal radiograph showed a normal pattern of bowel gas, no evidence of free air, and a moderate amount of stool throughout the colon, which was not dilated. Ultrasonography performed on the second day (Fig. 1A) showed diffuse echogenicity and a moderate increase in the size of both kidneys. A sagittal view showed a moderate amount of fluid in the pelvis. Dr. P. Ellen Grant: MRI of the brain on the third day showed areas of increased signal intensity (Fig. 1B) in the subcortical white matter in the
n engl j med 361;4
The duration of the renal insufficiency is useful information in sorting out the differential diagnosis of the renal failure. The elevated serum creatinine level precludes new-onset kidney injury. With normal muscle turnover, this child generates about 15 mg of creatinine per kilogram of body weight per day that would normally be excreted in the urine. With a normal glomerular filtration rate (GFR) and adequate hydration, this creatinine burden is excreted, resulting in a stable serum creatinine level. With a lack of renal function, the creatinine generally rises by 2 mg per kilogram of body weight per day. His serum creatinine level of 16 mg per deciliter could thus reflect a complete lack of glomerular filtration for about a week, a slow chronic decline, or a chronic decline with superimposed acute decline. A review of the history and results of laboratory tests offer clues to the chronicity of this process. The degree of metabolic acidosis, hypocalcemia, and hyperphosphatemia is moderate, which suggests that the duration of severely reduced renal function is relatively short. In contrast, there is pronounced hyperkalemia, which may suggest a problem in addition to the decline in the GFR. The effects of a decreased GFR on homeostasis of growth hormone, parathyroid hormone, and erythropoietin also affect clinical facjuly 23, 2009
nejm.org
393
The New England Journal of Medicine Downloaded from nejm.org on September 22, 2012. For personal use only. No other uses without permission. Copyright 2009 Massachusetts Medical Society. All rights reserved.
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
Figure 1. Imaging Studies. An ultrasound image of the abdomen (Panel A) shows a sagittal view of the right kidney. The kidney is enlarged and diffusely echogenic without evidence of hydronephrosis. These findings are nonspecific but can be seen with renal RETAKE 1st ICM failure from a variety of causes. MRI of theAUTHOR Somers of increased signal intensity on fluid-attenuated inverbrain shows areas 2nd REG F FIGURE 1a-d white matter in the frontal, parietal, and occipital regions, sion recovery (FLAIR) images (Panel B) in the subcortical 3rd CASE TITLE on CT, with very little mass Revised These areas were bright on both corresponding to areas of low attenuation seen effect. EMail Line 4-C T2 -weighted (Panel C) and FLAIR (Panel D) images. SIZE
Enon
ARTIST: mst
FILL
H/T Combo
H/T
33p9
tors such as growth rate, bone cell mass. The childs last routine examination JOB: 36104 showed normal adolescent development, but comparing his recent rate of growth with normal ranges might reveal a new delay in growth. His markedly elevated parathyroid hormone level and the hypocalcemia and hyperphosphatemia suggest chronic renal insufficiency. The hemoglobin level of less than 10 g per deciliter indicates anemia and may be related to renal failure, but in combination with mild thrombocytopenia, an
394
AUTHOR, PLEASE NOTE: Figure has been redrawn and type has been reset. Please check carefully. health, and red- elevated serum lactate
dehydrogenase level, and indirect hyperbilirubinemia, it also suggests conISSUE: 7-23-09 comitant microangiopathy, a process that could contribute to severe hyperkalemia.
Causes of Nephritis
There are four broad categories of renal disease that can lead to the acute nephritic pattern: acute interstitial nephritis, acute glomerulonephritis, chronic glomerulonephritis with exacerbation, and the hemolyticuremic syndrome. Although idio-
n engl j med 361;4
nejm.org
july 23, 2009
The New England Journal of Medicine Downloaded from nejm.org on September 22, 2012. For personal use only. No other uses without permission. Copyright 2009 Massachusetts Medical Society. All rights reserved.
case records of the massachusetts gener al hospital
pathic interstitial nephritis occurs rarely, most episodes in children arise from drug hypersensitivity. Commonly implicated medications include penicillins, cephalosporins, and nonsteroidal antiinflammatory agents.1 Clinical and laboratory manifestations vary widely. Onset is about a week after exposure, fever and rash are common, edema and hypertension are less common, and renal dysfunction is variable. Eosinophilia and eosinophiluria can occur, and pyuria with white-cell casts is common. This boy has had no fever or rash and only brief exposure to amoxicillin. The urine sediment is more active and the renal insufficiency more pronounced than usual. Moreover, his renal impairment seems somewhat chronic and there may be a microangiopathy. Hypertension is a common characteristic of the three other categories of renal disease that present with a nephritic pattern. The degree of hypertension can be pronounced, as in this boy who presented with probable hypertensive encephalopathy according to both clinical features and radiographic imaging.2 Headache, drowsiness, vomiting, visual changes, and seizures are common, whereas focal neurologic deficits are less frequent. This boys presentation and imaging fit the picture of a hypertensive encephalopathy driven by renal disease.
Rapidly Progressive Glomerulonephritis
lupus; anticardiolipin antibodies are the usual cause of a lupus-induced thrombotic microangiopathy.6 HenochSchnlein purpura is also unlikely, since most children with this syndrome have skin findings and 70% have gastrointestinal and joint symptoms; these are all absent in this boy.7 Taken together, there is not compelling evidence of a rapidly progressive glomerulonephritis related to either acute or chronic nephritis.
The HemolyticUremic Syndrome
This childs profound renal insufficiency raises the specter of a rapidly progressive glomerulonephritis. The data suggest renal disease with a duration of no more than several months. The severe and rapid renal impairment, oliguria, edema, and hypertension are classic clinical features of a rapidly progressive glomerulonephritis. Immunecomplex diseases such as postinfectious nephritis, IgA nephropathy and HenochSchnlein purpura, and lupus nephritis constitute at least two thirds of cases.3-5 To help make a specific diagnosis, the clinician should assess complement levels and perform serologic tests for ANCA-associated disease and lupus. This patient has no history of recent infection to suggest postinfectious nephritis. ANCA-associated and antiglomerular basement membrane disease are unlikely because of the negative serologic tests. The child does not have the diagnostic criteria for lupus, and he had a negative test for anticardiolipin antibodies, a test that is positive in up to three quarters of patients with
n engl j med 361;4
As a result, we turn to the hemolyticuremic syndrome as a possible cause of this childs renal injury. The suggestion of thrombotic microangiopathy in the initial laboratory-test results makes the hemolyticuremic syndrome an attractive unifying diagnosis, but it is important to determine whether the microangiopathy is a primary process causing the renal dysfunction and hypertension or whether it is secondary to chronic glomerulopathy or hypertension. Other than in cases of lupus, thrombotic microangiopathy is rare in children with chronic glomerular diseases, and when this entity has been described, it has been in children with a nephrotic pattern of renal disease. This leads to speculation that either the procoagulant state or endothelial injury linked to nephrosis caused the hemolyticuremic syndrome.8 Since this child has no apparent preexisting glomerular disease and does not have the nephrotic syndrome, it is unlikely that his hemolyticuremic syndrome is linked to chronic glomerulopathy. By activating the reninangiotensinaldosterone system and causing shear stress, malignant hypertension contributes to endothelial-cell injury and promotes thrombotic microangiopathy.9 A history of severe hypertension with end-organ damage such as retinopathy or cardiac changes would increase the clinical suspicion that the microangiopathy is linked to blood pressure.10 Patients with such hypertension-mediated thrombotic microangiopathy have hematuria, proteinuria, and renal insufficiency, and although most have anemia, a hemoglobin level below 10 g per deciliter is unusual,11 as is an elevated serum lactate dehydrogenase or bilirubin level, thrombocytopenia, heavy proteinuria, or a severe decrease in GFR, all of which are prominent features in this child. Table 3 summarizes conditions causing thrombotic microangiopathy and renal injury in children. This child has the classic triad of the hemolytic uremic syndrome: microangiopathic anemia, thromjuly 23, 2009
nejm.org
395
The New England Journal of Medicine Downloaded from nejm.org on September 22, 2012. For personal use only. No other uses without permission. Copyright 2009 Massachusetts Medical Society. All rights reserved.
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
Table 3. Thrombotic Microangiopathies Commonly Leading to Renal Injury. Variable Clinical characteristics Prodromal illness Possible Diarrhea, usually enterohemorrhagic Escherichia coli Variable Rare Common Variable Variable Common Common None Variable Thrombotic Thrombocytopenic Purpura Typical Hemolytic Uremic Syndrome Atypical Hemolytic Uremic Syndrome
Fever Neurologic abnormalities Acute oliguria or anuria Severe hypertension Early laboratory findings Severe thrombocytopenia (platelets, 25,000/mm3) Severe anemia (hemoglobin, 6 g/dl) Severe azotemia (blood urea nitrogen, >100 mg/dl [36 mmol/liter]) Genetic associations
Common Common Rare Possible Common Possible Possible ADAMTS 13 deficiency or autoantibody
Variable Variable Rare Common Variable Variable Variable Complement regulatory factor mutation or autoantibody (factor H, factor I, membrane cofactor protein) Variable No <50 50 <80
Utility of plasma infusion or plasmapheresis Prognosis Rapid resolution of acute illness Chronic renal failure within 1 year of onset (% of patients) Progression to end-stage renal disease (% of patients) Recurrence post-transplantation (% of patients)
Yes No 25 <50 <50
No Yes 5 20 0
bocytopenia without coagulopathy, and renal failure. A negative Coombs test, a blood smear with morphologic evidence of hemolysis, and serial measurements of markers of hemolysis, such as lactate dehydrogenase and haptoglobin, would be useful data to support a diagnosis of the hemolyticuremic syndrome. The absence of fever, the absence of neurologic abnormalities not associated with hypertension, and severe renal insufficiency make thrombotic thrombocytopenic purpura less likely, as would normal levels of von Willebrand factorcleaving protease (ADAMTS 13); the levels are deficient in most cases of thrombotic thrombocytopenic purpura.12 The hemolyticuremic syndrome in children is classified into two categories: typical hemolytic uremic syndrome with a diarrheal prodrome (D+), and atypical hemolyticuremic syndrome unassociated with diarrhea (D). Up to 90% of chil396
n engl j med 361;4
dren with the hemolyticuremic syndrome have typical disease, generally presenting before they are school age, with acute onset occurring after bloody diarrhea precipitated by verotoxin-producing bacteria such as Escherichia coli O157:H7.13 Although many affected children have severe acute kidney injury, the majority regain effective function.14 Atypical hemolyticuremic syndrome occurs at any age, and the onset tends to be insidious, often with marked hypertension; relapses occur that lead ultimately to end-stage renal disease.14 There is no specific prodromal illness, although atypical hemolyticuremic syndrome may occur after or concurrently with illness, and 30 to 40% of pediatric cases are associated with severe pneumococcal disease.3 Some types of Streptococcus pneumoniae produce a neuraminidase that cleaves sialic acid residues from renal endothelial cells,
july 23, 2009
nejm.org
The New England Journal of Medicine Downloaded from nejm.org on September 22, 2012. For personal use only. No other uses without permission. Copyright 2009 Massachusetts Medical Society. All rights reserved.
case records of the massachusetts gener al hospital
thereby exposing the ThomsenFriedenreich (T) antigen to an anti-T immunoglobulin commonly found in the plasma, leading to endothelial damage and thrombotic microangiopathy.15 Atypical hemolyticuremic syndrome may also occur after exposure to drugs that mediate endothelial-cell damage by various mechanisms, such as quinine, mitomycin C, oral contraceptives, and the calcineurin inhibitors cyclosporine and tacrolimus.7 This patient had no known exposure to S. pneumoniae or relevant drugs. In the past decade, up to half of the cases in children have been shown to involve abnormalities of complement factor H (CFH), factor I, or membrane cofactor protein (MCP).16 Either a gene mutation or an autoantibody directed against one of these regulatory proteins leads to an inability to dampen alternative complement-cascade activity, mediating renal endothelial-cell injury and the initiation of thrombotic microangiopathy. Mutations in CFH often lead to severe disease.17 Few cases of factor Ilinked disease have been described, and MCP-associated disease seems to manifest as the least severe phenotype.16 It is not clear what triggers the onset of disease in children with these genetic predispositions. Approaches to therapy include plasma infusion to introduce functional factors and plasmapheresis to remove autoantibodies. In this child with the hemolyticuremic syndrome triad but no diarrheal prodrome, atypical hemolyticuremic syndrome must be considered. The absence of previous drug exposure, specific infection, or systemic illness puts atypical hemolyticuremic syndrome associated with complement dysregulation high on the list of disorders in the differential diagnosis. A percutaneous renal biopsy will help clarify the diagnosis.
of capillary loops (Fig. 2A). Multiple arterioles had swollen endothelial cells with luminal fibrin and platelets and fragmented red cells within the lumens and in the walls (Fig. 2A, inset). Immunofluorescence microscopy revealed focal, trace, and irregular staining in the mesangium for IgM and the complement protein C3. No fibrin was detected in a relatively small number of examined glomeruli. However, staining for IgM, C3, C1q, and fibrin was detected in the walls of several small arteries and arterioles, some of which appeared to be thrombosed (Fig. 2B). Tubular reabsorption droplets stained for IgG, albumin, and kappa and lambda light chains, indicating the presence of increased glomerular permeability. Electron microscopical examination showed widespread collapse of glomerular capillary lumens, with wrinkling of glomerular basement membranes and podocyte foot-process effacement (Fig. 2C). Glomerular endothelial cells were swollen, with widespread loss of fenestrae, a feature consistent with endothelial-cell injury. Endothelialcell injury was also present in arterioles and small arteries. These showed partial occlusion of vascular lumens by the swollen endothelial cells, scattered platelets intermixed with fibrin, and red cells. Deposition of fibrin, fragmented red cells, and leukocytes were noted in arterial walls. These pathological features indicate thrombotic microangiopathy, a descriptive term that encompasses the vascular pathology observed in the hemolyticuremic syndrome and thrombotic thrombocytopenic purpura. The pathological features do not permit distinction between these two entities or between typical and atypical hemolyticuremic syndrome.
Pathophysiology of the Hemolyticuremic syndrome
Thrombotic microangiopathy follows endothelialcell injury in multiple vascular beds. It may be Atypical hemolyticuremic syndrome. caused by autoantibodies targeting components of the coagulation or complement pathways, including antiphospholipid, antiADAMTS 13, and Dr . Mich a el J.G. Somer ss anti-CFH antibodies, or by genetic mutations in Di agnosis components of these pathways, including ADAMTS Atypical hemolyticuremic syndrome. 13, CFH, MCP, and factor I. In the hemolytic uremic syndrome, endothelial-cell damage is especially prominent in the kidney. The injury may Pathol o gic a l Discussion be mediated by bacterial toxin, as in typical hemoDr. Eveline E. Schneeberger: A renal-biopsy specimen lyticuremic syndrome, or by drugs, as in some was obtained. Most glomeruli displayed collapse cases of atypical hemolyticuremic syndrome.
Cl inic a l Di agnosis
n engl j med 361;4
nejm.org
july 23, 2009
397
The New England Journal of Medicine Downloaded from nejm.org on September 22, 2012. For personal use only. No other uses without permission. Copyright 2009 Massachusetts Medical Society. All rights reserved.
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
Figure 2. Renal-Biopsy Specimens. In the first biopsy specimen (Panel A), the majority of glomeruli appeared collapsed, with only a few red cells present in glomerular capillaries. Fibrinoid necrosis with entrapped red-cell fragments (inset) is present in a number of RETAKE 1st AUTHOR Somers ICM arterioles. Immunofluorescence microscopy (Panel B) shows infiltration of a small artery by fibrin and a luminal 2nd 2a-d thrombus. Electron microscopy of aREG F FIGURE glomerulus (Panel C) shows collapse of glomerular capillaries and swollen en3rd CASE trapped red cells. There is widespread podocyte foot-process effacement. TITLE dothelial cells, with loss of fenestrae and Revised EMail Line 4-C In the second biopsy, obtained 12 weeks later (Panel D), glomeruli are collapsed, partially sclerosed, or both. This SIZE Enon H/T is accompanied by focal interstitial fibrosisARTIST: mst atrophy. The H/T and tubular lumens of many arterioles are obliterated by FILL 33p9 Combo intimal fibrosis (inset).
AUTHOR, PLEASE NOTE: Figure has been redrawn and type has been reset. Please check carefully.
Atypical hemolyticuremic syndrome due to abJOB: 36104 normalities in the complement pathway results from complement-mediated endothelial injury. Normally, a small amount of C3b is deposited on all cells that are in contact with plasma. The concerted actions of MCP and plasma CFH, together with the proteolytic action of factor I, lead to the inactivation of deposited C3b on endothelial cells, thereby preventing propagation of the C3bamplification loop. Mutations in any one of these factors leads to a failure to control C3 amplifica-
tion, ISSUE: 7-23-09 endothelial-cell lysis and the resulting in development of thrombotic microangiopathy.18 Dr. Amita Sharma: In this patient, we strongly suspected the diagnosis of atypical hemolytic uremic syndrome. Determination of plasma levels of C3, CFH, complement factor I (CFI), complement factor H receptor (CFHR), CFHR1, CFHR3, and complement factor B (CFB); the expression of MCP; and screening for anti-CFH antibodies is indicated in the evaluation of all patients with atypical hemolyticuremic syndrome. This patient
398
n engl j med 361;4
nejm.org
july 23, 2009
The New England Journal of Medicine Downloaded from nejm.org on September 22, 2012. For personal use only. No other uses without permission. Copyright 2009 Massachusetts Medical Society. All rights reserved.
case records of the massachusetts gener al hospital
had normal antigenic levels of factor H, factor I, and MCP. Genotyping of CFH, CFI, and MCP and, if possible, CFB and C3 is indicated, even if plasma levels are normal. Since mutations are predisposing rather than causal, the risk of the development of the hemolyticuremic syndrome in a patient with a mutation cannot be quantified. However, patients should be monitored during high-risk periods, such as when they have viral infections, and advised to avoid known precipitants such as oral contraceptives.19 Identification of the specific mutation is also important because of differences in mortality, renal function, the response to therapy, and the outcome of renal transplantation.20 Genetic testing in this patient disclosed a heterozygous, missense mutation (S1191L) on short consensus repeat 20 of CFH. CFH consists of 20 contiguous modules called short consensus repeats. The first four repeats include the major C3b binding site and regulate the fluidphase function. The defects in CFH can be classified as one of two types. In type I, the mutations lead to quantitative deficiency, whereas in type II (present in 25 to 75% of cases), the protein level is normal but one or more of its functions may be affected. The type II mutation seen in this patient led to decreased binding of C3b to endothelial cells, with intact fluid-phase function and normal protein levels in plasma.21-23 Current treatment of atypical hemolyticuremic syndrome involves plasma exchange or plasma infusion.24 Since CFH is synthesized predominantly in the liver, kidney transplantation alone does not correct the deficiency. Combined liver and kidney transplantation with perioperative plasma infusion or exchange to elevate the level of wild-type complement regulators has been successful.25 Living-donor transplantation from family members is contraindicated, because of both the high risk of graft loss due to recurrent hemolyticuremic syndrome, and the risk that related donors may share the recipients genetic predisposition. The development of functional complement regulatory proteins by means of recombinant technology would also allow for infusions of these proteins as a new therapeutic approach to prevent disease activation or reactivation after transplantation. This patient was treated initially with plasma exchange and subsequently with plasma infusion. Approximately 8 weeks after initial presentation, he remained dependent on dialysis and had onn engl j med 361;4
going hemolysis. These factors prompted a repeat renal biopsy. Dr. Schneeberger: The second biopsy specimen, obtained 12 weeks later, showed global sclerosis of one third of the glomeruli. The other glomeruli showed wrinkled and segmentally thickened glomerular basement membranes and segmental collapse of glomerular capillaries (Fig. 2D). Many of the arteries were occluded by fibrous connective tissue (Fig. 2D, inset), and one had a fresh thrombus. Tubular atrophy and interstitial fibrosis involved approximately 30% of the cortex. Immunofluorescence studies showed minimal focal staining for IgM, C3, and fibrin in the glomeruli and some afferent arterioles. Electron microscopical examination of a single glomerulus revealed features similar to those observed in the first biopsy. Dr. Sharma: Since examination of the biopsy specimen showed viable renal tissue, aggressive plasma exchange was instituted, angiotensinconvertingenzyme inhibitors were added for control of hypertension, and hemodialysis was continued. However, after another 6 weeks, the patients hypertension remained difficult to control, and hemolysis persisted. The family preference and likelihood that hemodialysis may have been contributing to ongoing hemolysis made us switch to peritoneal dialysis. With peritoneal dialysis, hemolysis ceased, and with the decline in renal function, hypertension was easy to control with monotherapy. It has been 2 years since his initial presentation, and he is doing well on peritoneal dialysis. The family is weighing the risk of combined liver and kidney transplantation against continued dialysis while awaiting the development of novel therapies that may use monoclonal antibodies or recombinant proteins to alter complement-cascade dysregulation. Dr. Nancy Lee Harris (Pathology): Would you consider genetic testing of family members? Dr. Somers: Genetic testing is indicated for relatives of an affected person who are considering donating a kidney to that person. The role of more widespread genetic screening for relatives is unclear at this point.
A nat omic a l Di agnosis
Atypical hemolyticuremic syndrome with complement factor H mutation.
Dr. Guimaraes reports receiving grant support from AstraZeneca. No other potential conflict of interest relevant to this article was reported.
july 23, 2009
nejm.org
399
The New England Journal of Medicine Downloaded from nejm.org on September 22, 2012. For personal use only. No other uses without permission. Copyright 2009 Massachusetts Medical Society. All rights reserved.
case records of the massachusetts gener al hospital
References
1. Alon U. Tubulointerstitial nephritis.
In: Avner ED, Harmon WE, Niaudet P, eds. Pediatric nephrology. 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2004:817-31. 2. Prasad N, Gulati S, Gupta RK, et al. Spectrum of radiological changes in hypertensive children with reversible posterior leucoencephalopathy. Br J Radiol 2007;80:422-9. 3. A clinico-pathologic study of crescentic glomerulonephritis in 50 children: a report of the Southwest Pediatric Nephrology Study Group. Kidney Int 1985;27: 450-8. 4. Jardim HM, Leake J, Risdon RA, Barratt TM, Dillon MJ. Crescentic glomerulonephritis in children. Pediatr Nephrol 1992;6:231-5. 5. Niaundet P, Levy M. Glomerulonephrites a croissants diffuse. In: Royer P, Habib R, Mathiew H, Broyer M, eds. Nephrologie pediatrique. 3rd ed. Paris: Flammarion, 1983:381-94. 6. Garg S, Kurien A. Lupus anticoagulant and anticardiolipin antibodies in SLE with secondary antiphospholipid antibody syndrome. Turk J Hematol 2007;24: 69-74. 7. Coppo R, Amore A. Henoch-Schonlein purpura. In: Avner ED, Harmon WE, Niaudet P, eds. Pediatric nephrology. 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2004:851-63. 8. Morita S, Sakai T, Okamoto N, et al. Hemolytic uremic syndrome associated with immunoglobulin A nephropathy: a case report and review of cases of hemolytic uremic syndrome with glomerular disease. Intern Med 1999;38:495-9. 9. Shibagaki Y, Fujita T. Thrombotic mi-
croangiopathy in malignant hypertension and hemolytic uremic syndrome (HUS)/ thrombotic thrombocytopenic purpura (TTP): can we differentiate one from the other? Hypertens Res 2005;28:89-95. 10. Rifkin BS, Brewster UC. Thrombotic microangiopathy associated with malignant hypertension. Mayo Clin Proc 2006; 81:593. 11. Zhang B, Xing C, Yu X, Sun B, Zhao X, Qian J. Renal thrombotic microangiopathies induced by severe hypertension. Hypertens Res 2008;31:479-83. 12. Tsai HM. Is severe deficiency of ADAMTS-13 specific for thrombotic thrombocytopenic purpura? Yes. J Thromb Haemost 2003;1:625-31. 13. Noris M, Remuzzi G. Non-shiga toxin-associated hemolytic uremic syndrome. In: Zipfel P, ed. Complement and kidney disease. Basel, Switzerland: BirkhauserVerlag, 2005:65-83. 14. Amirlak I, Amirlak B. Haemolytic uraemic syndrome: an overview. Nephrology (Carlton) 2006;11:213-8. 15. Klein PJ, Bulla M, Newman RA, et al. Thomsen-Friedenreich antigen in haemolytic-uraemic syndrome. Lancet 1977;2: 1024-5. 16. Kavanagh D, Goodship TH, Richards A. Atypical haemolytic uraemic syndrome. Br Med Bull 2006;77-78:5-22. 17. Skerka C, Jozsi M. Role of complement and factor H in hemolytic uremic syndrome. In: Zipfel PF, ed. Complement and kidney disease. Basel, Switzerland: Birkhauser-Verlag, 2005:85-109. 18. Jokiranta TS, Jaakola VP, Lehtinen MJ, Prepalo M, Meri S, Goldman A. Structure of complement factor H carboxylterminus reveals molecular basis of atypi-
cal haemolytic uremic syndrome. EMBO J 2006;25:1784-94. 19. Kavanagh D, Richards A, FremeauxBacchi V, et al. Screening for complement system abnormalities in patients with atypical hemolytic uremic syndrome. Clin J Am Soc Nephrol 2007;2:591-6. 20. Caprioli J, Noris M, Brioschi S, et al. Genetics of HUS: the impact of MCP, CFH, and IF mutations on clinical presentation, response to treatment, and outcome. Blood 2006;108:1267-79. 21. Heinen S, Jozsi M, Hartmann A, et al. Hemolytic uremic syndrome: a factor H mutation (E1172Stop) causes defective complement control at the surface of endothelial cells. J Am Soc Nephrol 2007; 18:506-14. 22. Pickering MC, de Jorge EG, MartinezBarricarte R, et al. Spontaneous hemolytic uremic syndrome triggered by complement factor H lacking surface recognition domains. J Exp Med 2007;204:1249-56. 23. Sthl AL, Vaziri-Sani F, Heinen S, et al. Factor H dysfunction in patients with atypical hemolytic uremic syndrome contributes to complement deposition on platelets and their activation. Blood 2008; 111:5307-15. 24. Lapeyraque AL, Wagner E, Phan V, et al. Efficacy of plasma therapy in atypical hemolytic uremic syndrome with complement factor H mutations. Pediatr Nephrol 2008;23:1363-6. 25. Jalanko H, Peltonen S, Koskinen A, et al. Successful liver-kidney transplantation in two children with aHUS caused by a mutation in complement factor H. Am J Transplant 2008;8:216-21.
Copyright 2009 Massachusetts Medical Society.
Lantern Slides Updated: Complete PowerPoint Slide Sets from the Clinicopathological Conferences
Any reader of the Journal who uses the Case Records of the Massachusetts General Hospital as a teaching exercise or reference material is now eligible to receive a complete set of PowerPoint slides, including digital images, with identifying legends, shown at the live Clinicopathological Conference (CPC) that is the basis of the Case Record. This slide set contains all of the images from the CPC, not only those published in the Journal. Radiographic, neurologic, and cardiac studies, gross specimens, and photomicrographs, as well as unpublished text slides, tables, and diagrams, are included. Every year 40 sets are produced, averaging 50-60 slides per set. Each set is supplied on a compact disc and is mailed to coincide with the publication of the Case Record. The cost of an annual subscription is $600, or individual sets may be purchased for $50 each. Application forms for the current subscription year, which began in January, may be obtained from the Lantern Slides Service, Department of Pathology, Massachusetts General Hospital, Boston, MA 02114 (telephone 617-726-2974) or e-mail Pathphotoslides@partners.org.
400
n engl j med 361;4
nejm.org
july 23, 2009
The New England Journal of Medicine Downloaded from nejm.org on September 22, 2012. For personal use only. No other uses without permission. Copyright 2009 Massachusetts Medical Society. All rights reserved.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Today! 2 Activity Book AKDocument10 pagesToday! 2 Activity Book AKMark Arenz Corixmir80% (5)
- Method Statement of T-Beams PDFDocument14 pagesMethod Statement of T-Beams PDFKAmi KaMranNo ratings yet
- TMJDocument38 pagesTMJAnonymous 6kAmeZzINo ratings yet
- Dynamic Test Report of DECR-S Excitation Devices: ExperimenterDocument14 pagesDynamic Test Report of DECR-S Excitation Devices: ExperimenterSalmanEjazNo ratings yet
- Looking For Cochlear Dead Regions A Clinical Experience With TEN TestDocument9 pagesLooking For Cochlear Dead Regions A Clinical Experience With TEN TestVinay S NNo ratings yet
- Las Mapeh 9 q2 w6 HealthDocument8 pagesLas Mapeh 9 q2 w6 HealthJemalyn Hibaya Lasaca100% (1)
- B11 - Overload Relays (Ref) ENDocument20 pagesB11 - Overload Relays (Ref) ENAhmed AbazaNo ratings yet
- Aljac Sampler: Environmentally Acceptable, Operationally Efficient and Safe, Eliminating Any Product LossDocument3 pagesAljac Sampler: Environmentally Acceptable, Operationally Efficient and Safe, Eliminating Any Product LossT. LimNo ratings yet
- C.E. 324 - Ethics - 1.0Document103 pagesC.E. 324 - Ethics - 1.0dela rosaNo ratings yet
- Vein Type DepositDocument7 pagesVein Type DepositHarisArmadiNo ratings yet
- Vocal TractDocument16 pagesVocal TractniroelNo ratings yet
- Van Pham Tieng Anh Co Ban Nang CaoDocument18 pagesVan Pham Tieng Anh Co Ban Nang CaoookuroooNo ratings yet
- Fact Sheeton Canola OilDocument15 pagesFact Sheeton Canola OilMonika ThadeaNo ratings yet
- Scan&SolveDocument24 pagesScan&SolveAtul ChauhanNo ratings yet
- A MCQ: Si - No Sub Topics NameDocument2 pagesA MCQ: Si - No Sub Topics NameInzamamul Haque ShihabNo ratings yet
- Lake Superior RoadmapDocument2 pagesLake Superior RoadmapWDIV/ClickOnDetroitNo ratings yet
- Economics 526 - Mathematics For Economists: Day(s) Time LocationDocument5 pagesEconomics 526 - Mathematics For Economists: Day(s) Time LocationGaurav JakhuNo ratings yet
- A Guide To Maintenance Metrics-ProgramDocument5 pagesA Guide To Maintenance Metrics-ProgramLy QuanNo ratings yet
- Assay - Alumina and Magnesia Oral SuspensionDocument3 pagesAssay - Alumina and Magnesia Oral SuspensionmaimaiNo ratings yet
- Strength of Materials: 2. Assume Missing Data, If Any, SuitablyDocument2 pagesStrength of Materials: 2. Assume Missing Data, If Any, SuitablynvnrevNo ratings yet
- Netrunner AllCardsDocument154 pagesNetrunner AllCardsIvo PantaleaoNo ratings yet
- PX 150 UsaDocument138 pagesPX 150 UsaramiroNo ratings yet
- Manual de Servico Samsung Sgh-I677-Eplis-11Document10 pagesManual de Servico Samsung Sgh-I677-Eplis-11Anselmo Antunes0% (1)
- Power and Propulsion PDFDocument13 pagesPower and Propulsion PDFahmedalgaloNo ratings yet
- IKEA - Huntsman Positive List - 27 May 2016 - EN - FINAL - v1Document30 pagesIKEA - Huntsman Positive List - 27 May 2016 - EN - FINAL - v1Flávia DutraNo ratings yet
- Essentials of o Ste 00 DaveDocument112 pagesEssentials of o Ste 00 DaveGeki Iovan100% (1)
- Corrosion Resistant Steels: Stainless Steel AlloysDocument11 pagesCorrosion Resistant Steels: Stainless Steel AlloysPraveen SamarthiNo ratings yet
- Obs and Gynae PassmedDocument7 pagesObs and Gynae PassmedrahulNo ratings yet
- Listening DictationDocument3 pagesListening DictationThảo ĐinhNo ratings yet
- bNSG9000 Datasheet 2Document3 pagesbNSG9000 Datasheet 2RobertNo ratings yet