Professional Documents
Culture Documents
Anti Coagulants Anti Platelets Fibrinolytics
Anti Coagulants Anti Platelets Fibrinolytics
Uploaded by
Muhammad UsmanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anti Coagulants Anti Platelets Fibrinolytics
Anti Coagulants Anti Platelets Fibrinolytics
Uploaded by
Muhammad UsmanCopyright:
Available Formats
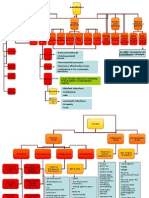
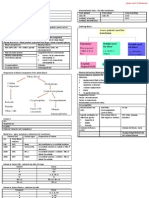
Anti-Coagulants, Anti-Platelets, Fibrinolytics Anti-Coagulants Parenteral (Rapid acting) Oral (Delayed acting) Standard Heparin Warf arin Low
Molecular Weight Heparin Fondaparinux (Pentasaccharide) Inhibits Function of Clotting Factors Inhibit Synthesis of Clotting Factors Help prevent thrombus formation No direct effect on a thrombus already formed
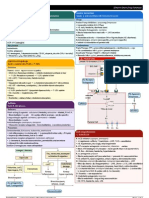
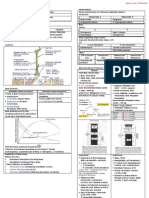
Standard Hepar in (Unfractionated Hepar in, Conventi onal Hepar in) Available in Mast Ce lls of Human T issue s Commercially from Porcine Intestinal Mucosa, Bovi ne Lung MOA Inhibit C lotting Factor Protease XIIa, XIa, IXa, IIa, Xa (12,11,9,2,10) (through action o n An tithromb in III) Binds to AT III, cause conformational change (for more rapid interaction wit h protea ses) AT III Inhibits C lotting Factor Proteases by forming complexes wit h them Pharmacokinetics Not absorbed from GIT (large molecule) (therefore given Parenta lly) IV IM SC Immediate onset Avoided Bioavailabi lity varie s action (Cause Hematoma) (onset action de layed 1-2 ho urs) Cleared from circulat ion by RES, Metaboli sed by Liver Half Life - (1-1 hour s)(effect disappears with in h ours) Do not cross Placenta (big molecule) (can be g iven in Pregnancy) Does not enter Breast Mi lk Clin ical App licatio n (Venous Thromb os is) Therapy Prophylaxis DVT, Pulmonary Emboli sm, Arteria l Thromb us & R isk (Immobilized, Surgical pt) Embolism, MI DVT No direct effect on Thromb us that has been Pulmonary Embol ism formed Does not guarantee Thrombos is does not occur Prevent Further Extensi on, Emboli sation of Formed Clot ( Ri sk 60-80%) Dose tha n Prop hylaxis Subcutaneous Adm inist ration Monito r Anticoagu lant Activity aPTT Adverse Effects Bleeding (ep istaxis, hematur ia, melena, ecchymosis) Heparin Induced Thrombocytopenia (HIT) Excess Anticoagulant Managed by Dose/ Discontin ue Heparin Antidote Protami ne Sulfate Heparin Induced Thrombocytope nia Low Mo lecular Weight Heparin (LMWH) (Enoxaparin, Daltepari n, Nadroparin) Fragments 1/3 of UFH size All Porcine ba sed MOA Inhibit Protea se Xa (via Anti-th rombin) Pharmacokinetics Smaller molecular size (compared to standard he parin) Better subcutaneou s b ioavailabi lity (compared to standard heparin) Half-Life - (les s frequent dos ing requ ired) Cleared Rena lly (Half-life in Re nal Fai lure require dose reduction) Clin ical App licatio n Therapy Prophylaxis Adverse Effects Bleeding (e specially if overdo se) Heparin ind uced thrombocytopenia ( i ncidence compared to standard he parin) Warfarin Vitamin K Antagon ist MOA Inhibit synthe si s of active Vitamin K depende nt clotti ng factors by liver (Factor VII, IX, X, II) Vitamin K Cofactor i n gamma carboxylation (needed fo r activation) of these factors duri ng synthes is (these factors ineffective i n coagulation) Pharmacokinetics Good GIT Absor ption (100% B ioavailab ility) Half-Life - ( >36 h ours) (da ily do sing is adequate) Transformed to Inactive Metabol ite by Liver Liver Disease (enhance anticoagulant effect, start d ose in liver fai lure) Duration of Action after drug d iscontinue d pe rsi st to 4-5 days Clin ical App licatio n Long term anticoagulant (eg. after Venou s Thr ombosi s) No effect on clotting factors already i n circulatio n Full Therapeut ic Effect Delayed 4-5 days (time balance between degradation of exist ing clotti ng factors, inh ibited synthes is of new factors) Monito r Anticoagu lant Effects Prothrombin Time International Normal ised Ratio (INR) (INR = Patient PT / Contr ol PT) Adverse Effects Bleeding (re lated to inten sity of a nticoagulation)( Antidote Vitamin K) Necrosis, Gangrene of Skin, Soft Ti ssue s Teratogenic (passes Placenta)(should not use in pregnancy) Drug Interactions Diet ( i n Vitamin K content - Warfar in effect), Compliance, Drugs, Herbs, Alcoho l Pharmacokinetic Pharmacodynamic Enzyme induction, En zyme Inhibit ion, Synergism Hepatic Disease Plasma Protein Bi nding Drugs Aspir in Drugs Inhib iting Enzyme Inducers Metabolism Plasma conc. Plasma conc. Decrease Effects Enhance Effect Fondaparin ux Synthetic Pentasaccharide MOA Selective Inhibitor of Activated Factor X Works by b indi ng to AT III, Potentiates Neutral isation of Factor Xa Interupts Bl ood C oagulation cascade, Inhibit Thromb in, Thrombus development Pharmacokinetics Excreted in Urine Half-Life - (17-21 hour s) (pro longed in Rena l Impairment) Clin ical Ind ication Similar to LMWH, Heparin
jslum.com | Medicine
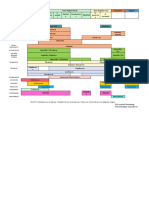
Anti-Platelets Cyclo-oxygenase ADP Receptor Inhibitors Inhibitors Aspirin Clopidogrel Inhibit Platelet Aggreg ation
Clin ical App licatio n Prevent 2 CVS events w ith h istory of vascular events (eg. Post MI, Stroke) Better at preventi ng Arter ial Th rombos is (not effective in preventi ng venous thrombo sis) Thromboxane A2, ADP sign ificant plate let aggregators Antiplate lets COX Inhibito rs Inhibit p latelet Thromboxane A2 production Aspir in
Fibrinolytics/ Thrombolytics Strep tokinase (widely used) Urokinase Tissue Plasminogen Activator (tPA) Increase Fibrinolysis
Fibrino lytic System Dissolves Intravascular Clot (due to action of Pla smin, an en zyme that dige st Fibr in) Plasminogen (inactive Precursor) Plasmin Enzyme that Digest Fi brin Clot s Fibrino lytics Promote Plasm in Formation (from Pla sminogen) Clin ical App licatio n Pulmonary Embol ism Myocardial Infarction (MI) (best w ithin 6 ho urs)(ASAP) All given Intravenous ly Contrain dicatio n Recent Surgery Bleeding Streptokina se Protein pr oduced by haemolytic st reptococci Adverse Effects Bleeding Allerg ic reactions (ant igenic) Anaphylaxis (rare ly) Fever (rarely) Tissue Pla smin ogen Activator Endogenously released from Endothe lial cells
ADP Inhibito rs Inhibit ADP-induced Platelet aggregation Ticlopidi ne Clopid ogrel
Cyclooxygenase Inhibito rs (eg. as pir in) (Ora lly)
In Platelet, major COX pro duct is TxA2 (induce platelet aggregation) Aspirin Inhibit Cyclooxygenase en zyme Irreversibly Inhibit synthe si s of Thr omboxane A2 Bleeding T ime Pr olonged Given Orally Daily ADP-Inhibitors (eg. Clo pid ogrel, Ticlopid ine) (Orally) Aspirin Alterna tive Unable to To lerate Aspir in (GI Intolerance, Hypersensitivity) Use with Aspir in (synergi sm) MOA Inhibit ADP Induced Platelet Aggregation Adverse Effects BM Suppres sion (eg. Neutropenia, Thrombocytopenia) GI Disturbances Haemorrhage
Differences - UFH, LMWH Structu re MOA UFH Larg e Molecular Weight Inhibit Proteases XIIa, XIa, IXa, IIa, Xa via Antithrombin aPTT Half-Life (about 1 hour) Do not cross placenta Not absorbed orally Protamine Sulfate LMWH Smaller Molecular Size Mainly Inhibit Protease Xa via Antithrombin aPTT not useful Half-Life (3-4 hours)( frequent dosing) Do not cross placenta Not absorbed orally No specific antidote SC Bioavailability better
Monitor Effects Kinetics
Antidote Kinetics
Differences Heparin, Warfarin Heparin Parenteral (IV, SC) Half-Life Monitoring by aPTT Rapid Anticoagulant effect Inhibit Proteases by action on Antithrombin III
Fetal Warfar in Syndr ome
Warfarin Oral Half-Life Monitoring by INR Delayed eff ects (days) Impair synthesis of Vitamin K dependent clotting factors
Infant wit h Hypoplastic nose Flat face Low nasal b ridge Altered Calcification
You might also like
- Antibiotic Study Cheat Sheet October 2018Document1 pageAntibiotic Study Cheat Sheet October 2018Nourhan100% (3)
- Mnemonics For AntibioticsDocument10 pagesMnemonics For AntibioticsShane AllenNo ratings yet
- Summary of All AnemiaDocument2 pagesSummary of All Anemiabenlarsena93% (14)
- Anticoagulants Drug TableDocument1 pageAnticoagulants Drug Tablecdp158767% (3)
- Mnemonics for Medicine: Differential Diagnoses and Other PearlsFrom EverandMnemonics for Medicine: Differential Diagnoses and Other PearlsRating: 5 out of 5 stars5/5 (3)
- Antibacterial Drugs SummaryDocument13 pagesAntibacterial Drugs SummaryNeo Ramagaga100% (1)
- Approach To Diagnosis of Haemolytic AnaemiasDocument2 pagesApproach To Diagnosis of Haemolytic AnaemiasGerardLumNo ratings yet
- Pharm-Drugs ChartsDocument21 pagesPharm-Drugs ChartsCandace Flowers100% (3)
- Soft Tissue InfectionsDocument3 pagesSoft Tissue InfectionsGerardLum100% (1)
- Pituitary Gland PathologyDocument4 pagesPituitary Gland PathologyGerardLumNo ratings yet
- History of Hemostasis in Neurosurgery Paulo Et Al 2018Document14 pagesHistory of Hemostasis in Neurosurgery Paulo Et Al 2018AlexNo ratings yet
- Drug Moa PK Use Se Ci Blood Coagulation: AnticoagulantsDocument4 pagesDrug Moa PK Use Se Ci Blood Coagulation: AnticoagulantsYusoff RamdzanNo ratings yet
- ChemotherapyDocument1 pageChemotherapyGerardLum100% (2)
- AntibioticsDocument6 pagesAntibioticsyezan27100% (8)
- Antibiotics Chart 2Document10 pagesAntibiotics Chart 2Vee MendNo ratings yet
- Cardiovascular Drug IntroductionDocument3 pagesCardiovascular Drug IntroductionSamah Khan100% (1)
- Acquired Bleeding DisordersDocument1 pageAcquired Bleeding DisordersGerardLumNo ratings yet
- 100 Essential Drugs1Document8 pages100 Essential Drugs1Sudip DevadasNo ratings yet
- Drugs For Diabetes MellitusDocument3 pagesDrugs For Diabetes MellitusGerardLum100% (1)
- Antibiotics Cheat SheetDocument2 pagesAntibiotics Cheat SheetAlejandro Rodas Salinas100% (1)
- Pharm Chemo Drugs SauldDocument6 pagesPharm Chemo Drugs Sauldneal100% (1)
- The Principles of Antibiotic Therapy: S. Aureus Streptococcus PneumoniaeDocument16 pagesThe Principles of Antibiotic Therapy: S. Aureus Streptococcus PneumoniaeDianne Chua100% (7)
- Acute Complications of Diabetes MellitusDocument1 pageAcute Complications of Diabetes MellitusGerardLum100% (1)
- Antibiotics Quick ReviewDocument5 pagesAntibiotics Quick Reviewpranjl100% (5)
- BED12 - Antibiotics PharmacologyDocument2 pagesBED12 - Antibiotics PharmacologyAmir AmirulNo ratings yet
- AntibioticsDocument6 pagesAntibioticsCyrus100% (1)
- Major Pharm ReviewDocument14 pagesMajor Pharm Reviewsarahpierre10100% (3)
- Anti-Arrhythmic Agents For Pharmacy PDFDocument41 pagesAnti-Arrhythmic Agents For Pharmacy PDFKelvinTMaikanaNo ratings yet
- Approximate Equivalents:: 0.100 Gmn. 1.00 GMDocument8 pagesApproximate Equivalents:: 0.100 Gmn. 1.00 GMakane ryuNo ratings yet
- Drug ChartDocument8 pagesDrug Chartstudentalwaysstudy100% (1)
- Antibiotics 101Document49 pagesAntibiotics 101Tony VoNo ratings yet
- Antibiotics and MnemonicsDocument8 pagesAntibiotics and MnemonicsMichael Howes100% (1)
- PharmacologyDocument13 pagesPharmacologyMa Carmela GuevarraNo ratings yet
- Antibiotic SummaryDocument4 pagesAntibiotic Summaryshazia100% (1)
- A.1. Community-Acquired: Use Antibiotics JudiciouslyDocument33 pagesA.1. Community-Acquired: Use Antibiotics JudiciouslymaxgroovesNo ratings yet
- Multiple Myeloma: LT Col Vivek AggarwalDocument42 pagesMultiple Myeloma: LT Col Vivek AggarwalShravan Rakaraddi100% (2)
- DiureticsDocument4 pagesDiureticsNazmul Islam AbirNo ratings yet
- List of Drugs Pharmacology 2Document13 pagesList of Drugs Pharmacology 2Maisarah Ab SamadNo ratings yet
- Antibiotics ChartDocument10 pagesAntibiotics Chartadom09No ratings yet
- Abx FinalDocument3 pagesAbx Finalyanks1120No ratings yet
- Adequacy Criteria: ExceptionsDocument3 pagesAdequacy Criteria: ExceptionsPranayNo ratings yet
- Musculoskeletal PharmacologyDocument18 pagesMusculoskeletal PharmacologyBLEEMAGE100% (2)
- Drug SummaryDocument5 pagesDrug Summarybriancripe100% (2)
- Pathophysiology of Calcium, Phosphate HomeostasisDocument5 pagesPathophysiology of Calcium, Phosphate HomeostasisGerardLum100% (1)
- Ninja - Anemias PDFDocument1 pageNinja - Anemias PDFErica Hyeyeon LeeNo ratings yet
- (CV2) Pharmacology of AnticoagulantsDocument6 pages(CV2) Pharmacology of AnticoagulantsHanifa Shereen B. AliNo ratings yet
- Acute Leukemia Best ArticleDocument8 pagesAcute Leukemia Best ArticleMahesh T MadhavanNo ratings yet
- Cancer DrugsDocument5 pagesCancer DrugsLinh HoangNo ratings yet
- WBC Neoplasms Review - PathologyDocument6 pagesWBC Neoplasms Review - Pathologylas100% (6)
- AntibioticsDocument9 pagesAntibioticsprince1500100% (1)
- AB ClassesDocument4 pagesAB Classesrayooona88100% (2)
- Ninja - Anti-HTN PDFDocument6 pagesNinja - Anti-HTN PDFErica Hyeyeon Lee100% (2)
- 2023.PharmacologyLab - Trans14.CancerChemotherapyPart1 2Document5 pages2023.PharmacologyLab - Trans14.CancerChemotherapyPart1 2Lloyd LinNo ratings yet
- AntibioticsDocument2 pagesAntibioticsPGI Custodio, Ed KristianNo ratings yet
- Pharmacology of Cardiac Function: Section of Pharmacology of the International Union of Physiological SciencesFrom EverandPharmacology of Cardiac Function: Section of Pharmacology of the International Union of Physiological SciencesOtto KrayerNo ratings yet
- Thrombosis and Bleeding Disorders: Theory and MethodsFrom EverandThrombosis and Bleeding Disorders: Theory and MethodsNils U. BangRating: 2 out of 5 stars2/5 (1)
- Fast Facts: Thrombotic Thrombocytopenic Purpura: Prompt action saves livesFrom EverandFast Facts: Thrombotic Thrombocytopenic Purpura: Prompt action saves livesNo ratings yet
- Soft Tissue TumoursDocument8 pagesSoft Tissue TumoursGerardLum100% (2)
- Urinary Tract InfectionDocument4 pagesUrinary Tract InfectionGerardLum100% (2)
- ThrombophiliaDocument3 pagesThrombophiliaGerardLum100% (1)
- Thyroid PhysiologyDocument2 pagesThyroid PhysiologyGerardLum100% (2)
- Renal Function in Disease StateDocument2 pagesRenal Function in Disease Statedamai140390No ratings yet
- Sexually Transmitted DiseasesDocument6 pagesSexually Transmitted DiseasesGerardLum100% (3)
- Prostate GlandsDocument3 pagesProstate GlandsDragan PetrovicNo ratings yet
- Renal Excretion of DrugsDocument3 pagesRenal Excretion of DrugsGerardLum100% (3)
- Pathology of Thyroid DiseasesDocument5 pagesPathology of Thyroid DiseasesGerardLum100% (3)
- Principles of Blood TransfusionDocument2 pagesPrinciples of Blood TransfusionGerardLum100% (3)
- Pathophysiology of Calcium, Phosphate HomeostasisDocument5 pagesPathophysiology of Calcium, Phosphate HomeostasisGerardLum100% (1)
- Overview of AnaemiaDocument2 pagesOverview of AnaemiaGerardLumNo ratings yet
- Pathology of TestesDocument4 pagesPathology of TestesGerardLum100% (1)
- Nocturnal EnuresisDocument1 pageNocturnal EnuresisGerardLumNo ratings yet
- Pathology of DiabetesDocument4 pagesPathology of DiabetesGerardLum100% (4)
- Pathogenesis Chronic Complications DiabetesDocument5 pagesPathogenesis Chronic Complications DiabetesGerardLum100% (1)
- Pathology GlomerulonephritisDocument4 pagesPathology GlomerulonephritisGerardLum100% (2)
- Paediatrics OrthopaedicsDocument5 pagesPaediatrics OrthopaedicsGerardLumNo ratings yet
- Obstructive UropathyDocument3 pagesObstructive UropathyGerardLum100% (1)
- Myeloproliferative DisordersDocument2 pagesMyeloproliferative DisordersGerardLumNo ratings yet
- Nsaids DrugsDocument2 pagesNsaids DrugsIrene Zae MwandotoNo ratings yet
- Lymph Node PathologyDocument4 pagesLymph Node PathologyGerardLum0% (1)
- Mechanism of MicturitionDocument4 pagesMechanism of MicturitionGerardLum100% (2)
- Introduction To TransplantationDocument3 pagesIntroduction To TransplantationGerardLumNo ratings yet
- Leukocytes Benign DisordersDocument3 pagesLeukocytes Benign DisordersGerardLum100% (3)
- Hemodynamic Disorders-RevisedDocument118 pagesHemodynamic Disorders-Revisedspringding0% (1)
- GS 201-250Document19 pagesGS 201-250Sara Abdul RahmanNo ratings yet
- Hemodynamic Disorders ThrombosisDocument106 pagesHemodynamic Disorders ThrombosisRamez AnaniNo ratings yet
- NCM 118 Altered Ventilatory FunctionDocument94 pagesNCM 118 Altered Ventilatory FunctionJezzabel Kyra BadayosNo ratings yet
- Summer ReviewerDocument49 pagesSummer ReviewerMarileth JeffersonNo ratings yet
- NCM 112 - Cardio 2 - Advance StudyDocument2 pagesNCM 112 - Cardio 2 - Advance StudyUzumaki KNo ratings yet
- Physio - Chapter 37Document4 pagesPhysio - Chapter 37Regina Ysabel SartagudaNo ratings yet
- PATHOPHYSIOLOGY LAB - Hanbook of Pathophysiology SevastreDocument192 pagesPATHOPHYSIOLOGY LAB - Hanbook of Pathophysiology Sevastredorina0101No ratings yet
- Deep Vein ThrombosisDocument24 pagesDeep Vein ThrombosisdinafiniNo ratings yet
- Drugs Affecting Blood CoagulationDocument51 pagesDrugs Affecting Blood CoagulationMoxie Macado100% (1)
- Agents Used in Blood DisordersDocument54 pagesAgents Used in Blood DisordersJing Lomboy AcostaNo ratings yet
- Sepsis and Septic ShockDocument70 pagesSepsis and Septic ShockLily SolNo ratings yet
- Coagulation DisordersDocument9 pagesCoagulation DisordersIS99057No ratings yet
- 5) Circulatory Disturbance BPT - 093303Document106 pages5) Circulatory Disturbance BPT - 093303Crystal GamingNo ratings yet
- Ryder 2001Document12 pagesRyder 2001Febria Valentine AritonangNo ratings yet
- Chapter 10 Blood AnatomyDocument5 pagesChapter 10 Blood AnatomyChiara Mae NiñalNo ratings yet
- DVT NotesDocument3 pagesDVT NotesTodd EvansNo ratings yet
- Streptokinase: PharmacologyDocument3 pagesStreptokinase: PharmacologyRegalado AguhayonNo ratings yet
- Англ тести фармDocument138 pagesАнгл тести фармRodriguez Vivanco Kevin DanielNo ratings yet
- 11 PathologyDocument26 pages11 PathologyRocky BullNo ratings yet
- Pulmonary EmbolismDocument23 pagesPulmonary EmbolismBianca Dizon50% (2)
- HEMOSTASISDocument12 pagesHEMOSTASISRyan PedregosaNo ratings yet
- Lecture On Hemodynamic and Thromboembolic DisordersDocument77 pagesLecture On Hemodynamic and Thromboembolic DisordersCharmaine Torio PastorNo ratings yet
- Dental Management of Patients Under Anticoagulant TherapyDocument15 pagesDental Management of Patients Under Anticoagulant TherapyThaer ZabenNo ratings yet
- The Body Matters Fyss - 2010 - English PDFDocument623 pagesThe Body Matters Fyss - 2010 - English PDFClauLopez99100% (1)
- Disseminated Intravascular Coagulation Is A Condition in Which Small Blood Clots DevelopDocument4 pagesDisseminated Intravascular Coagulation Is A Condition in Which Small Blood Clots DevelopRiaz JiwaNo ratings yet
- StrokeDocument28 pagesStrokeBEA RADANo ratings yet
- Anticoagulants and CoagulantsDocument31 pagesAnticoagulants and CoagulantsSandra PlausNo ratings yet
- 11-THROMBOLYTIC Drugs-Ishfaq 2016Document34 pages11-THROMBOLYTIC Drugs-Ishfaq 2016Eni Purwaeni100% (2)