Professional Documents
Culture Documents
Are Proton Pump Inhibitors More Effective Than Histamine
Uploaded by
nthie_unguCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Are Proton Pump Inhibitors More Effective Than Histamine
Uploaded by
nthie_unguCopyright:
Available Formats
Are proton pump inhibitors more effective than histamine-2 receptor antagonists for stress ulcer prophylaxis?
Stress-related gastrointestinal (GI) mucosal damage (also known as stress ulcers) can be detected endoscopically in the majority of critically ill patients; however, the incidence of clinically significant gastrointestinal bleeding as a result of this damage is approximately 1.5% to 1,2 4%. Patients who develop gastrointestinal bleeding have an increased risk of death and longer lengths of stay in the intensive care unit (ICU). Pathophysiology Gastrointestinal mucosal damage in critically ill patients is believed to be due to a number of factors, and is not completely understood. However, hypoperfusion of the gastrointestinal tract is 2,3 believed to be a primary cause of injury. The hypoperfusion may reduce the synthesis of the protective mucus layer which is also eroded by toxins or refluxed bile salts that are not rapidly removed due to decreased gastrointestinal motility. The acidic environment of the stomach contributes to the damage. Continued hypoperfusion impairs mucosal healing while reperfusion also contributes by enhancing the inflammatory response. Risk Factors A 1994 study by Cook and colleagues identified 2 primary risk factors for clinically relevant gastrointestinal bleeding in critically ill patients: greater than 48 hours of mechanical ventilation 1 and coagulopathy. Other risk factors include hypotension, renal or hepatic failure, sepsis, trauma (especially head or spinal cord injury), burns (>35% of body surface area), and a history of 2,3 gastrointestinal bleeding. Prophylaxis Antacids, sucralfate, histamine-2 receptor antagonists (H2RAs), and proton pump inhibitors (PPIs) have been evaluated for the prevention of stress ulcers in critically ill patients. Despite years of experience with these agents, and numerous clinical trials, the optimal prophylactic agent remains unknown. In 1999, the American Society of Health-System Pharmacists (ASHP) developed a clinical practice 4 guideline for stress ulcer prophylaxis. They recommended prophylaxis for patients who are mechanically ventilated for more than 48 hours, those with a history of gastrointestinal bleeding or ulcer within the past year, and in patients with 2 or more of the following: sepsis, ICU stay longer than 1 week, occult bleeding lasting 6 or more days, or use of high-dose corticosteroids. The recommended prophylactic agents included sucralfate for patients with gastric access via the oral, nasogastric, or gastrostomy route, and H2RAs for other critically ill patients at risk for stress ulcers. At the time of this guideline, there was minimal information on PPIs for stress ulcer prophylaxis; thus, they are not a recommended therapy. The ASHP guidelines are currently being updated with 5 an anticipated release date later this year. In 2008, the Eastern Association for the Surgery of Trauma (EAST) published clinical practice 6 guidelines for stress ulcer prophylaxis. They recommended prophylaxis for all patients who are mechanically ventilated, have coagulopathy, traumatic brain injury, or major burn injury. In addition, prophylaxis for patients in the ICU was recommended for patients with multiple trauma, sepsis, acute renal failure, an Injury Severity Score greater than 15, or patients using high-dose corticosteroids. The authors considered the efficacy of H2RAs, PPIs, and sucralfate to be equivalent. The 2008 Surviving Sepsis Campaign guidelines also included a statement on stress ulcer 7 prophylaxis. They recommended the use of either an H 2RA or a PPI. However, H2RAs were given a higher evidence grade (1A versus 1B). An update to these guidelines is anticipated in 2012. Generally, antacids are no longer used for stress ulcer prophylaxis. A 1996 meta-analysis determined that antacids did reduce the risk of bleeding compared with no therapy but this 8 difference was not significant. In addition, antacids were significantly inferior to H2RAs. The relative lack of efficacy coupled with an undesirable safety profile has eliminated antacids as 2,3 useful agents for stress ulcer prophylaxis in critically ill patients. In that same meta-analysis, 7 sucralfate did significantly reduce bleeding compared with no therapy. It also lowered the risk of pneumonia and improved mortality. However, sucralfate is not commonly used for stress ulcer prophylaxis. In fact, a 2004 survey of critical care physicians indicated that 87% prescribe either 9 an H2RA or PPI for stress ulcer prophylaxis. Differentiating the efficacy and safety of the H2RAs and PPIs has been attempted in numerous 10,11 clinical trials and meta-analyses. Two large recent meta-analyses have been published. Both meta-analyses showed a lower incidence of upper GI bleeding with PPIs compared with H 2 RAs; however, in the 2010 meta-analysis this difference was not statistically significant while it was
significant in the 2012 analysis. Characteristics of these meta-analyses are shown in the table below. Table. Recent meta-analyses evaluating PPIs and H2RAs for stress ulcer prophylaxis. 10 11 Barkun 2012 Lin 2010 Study inclusion criteria Randomized controlled trials in adult, critically ill patients at risk for GI bleeding PPIs versus H2RAs Clinically relevant outcomes (studies that only evaluated gastric pH were excluded) Randomized controlled trials in adult, critically ill patients PPIs versus H2RAs Clinically relevant outcomes (studies that only evaluated gastric pH were excluded) Studies that did not explicitly state whether the patients were in the ICU were excluded 7* 936 Patients with upper GI bleeding Pneumonia ICU mortality The incidence of GI bleeding was 11/540 (2.04%) with PPIs and 31/396 (7.83%) with H2RAs (pooled risk difference -0.04 (95% CI -0.09 to 0.01; p=0.08) The incidence of pneumonia was similar between groups; 10.8% with PPIs versus 10.4% with H2RAs (pooled risk difference 0.0; 95% CI -0.04 to 0.05; p=0.86) ICU mortality was also similar between groups 16.7% with PPIs versus 15% with H2RAs (pooled risk difference 0.02; 95% CI -0.04 to 0.08; p=0.5) PPIs and H2RAs have similar incidence of stress-related mucosal bleeding, pneumonia, and ICU mortality.
Number of studies Number of patients Primary outcome Other outcomes Results
13 1587 Clinically significant upper GI bleeding Nosocomial pneumonia All-cause mortality ICU days
The incidence of GI bleeding was reduced with PPIs compared to H2RAs (OR 0.30; 95% CI 0.17 to 0.54; NNT 39) The incidence of nosocomial pneumonia was similar with PPIs and H2RAs (OR 1.05; 95% CI 0.69 to 1.62) All cause mortality was similar with PPIs and H2RAs (1.19; 95% CI 0.84 to 1.68) The number of days in the ICU was similar with PPIs and H2RAs (WMD=-0.12 days; 95% CI -1.90 to 1.66) PPIs reduce the incidence of stress-related mucosal bleeding compared with H2RAs in critically ill patients with similar incidence of nosocomial pneumonia and mortality.
Conclusion
*All 7 studies were included in the 2012 meta-analysis. Abbreviations: CI=confidence interval, GI=gastrointestinal, H 2RAs=histamine-2 receptor antagonists, ICU=intensive care unit, NNT=number needed to treat, OR=odds ratio, PPIs=proton pump inhibitors, WMD=weighted mean difference. There were a number of different PPIs evaluated in the studies, but the most common PPIs were 10,11 intravenous pantoprazole or omeprazole (intravenous or oral). Intravenous cimetidine or ranitidine were the most commonly used H2RAs. It appears clear from these meta-analyses that there is no significant difference between these classes of drugs in mortality or pneumonia; however, whether PPIs offer a significant advantage in reducing stress ulcer bleeding is unclear. Additional concerns with the use of PPIs in place of H2RAs are their cost and association with Clostridium difficile-associated diarrhea. Neither of these issues was addressed in the above meta-analyses; however, a recent meta-analysis of case-control or cohort studies suggests a 12 strong association between PPI use andClostridium difficile-associated diarrhea.
Summary Stress ulcer prophylaxis with PPIs or H2RAs is commonly provided to critically ill patients at risk for gastrointestinal bleeding. A recent meta-analysis of 13 studies found a significant reduction in stress ulcer bleeding with PPIs in critically ill patients compared with H 2RAs. However, PPIs did not reduce the length of stay in the ICU or improve mortality compared with H2RAs. The primary limitation to choosing PPIs over H2RAs are cost related. Updated clinical practice guidelines are anticipated in late 2012. References: 1. Cook DJ, Fuller HD, Guyatt GH, et al for the Canadian Critical Care Trials Group. Risk factors for gastrointestinal bleeding in critically ill patients. N Engl J Med. 1994;330(6):377-381. 2. Ali T, Harty RF. Stress-induced ulcer bleeding in critically ill patients. Gastroenterol Clin N Am. 2009;38(2):245-265. 3. Quenot JP, Thiery N, Barbar S. When should stress ulcer prophylaxis be used in the ICU? Curr Opin Crit Care. 2009;15(2):139-143. 4. ASHP. ASHP therapeutic guidelines on stress ulcer prophylaxis. Am J Health-Syst Pharm. 1999;56(4):347-379. 5. Therapeutic Guidelines. American Society of Health-System Pharmacists Web site.http://www.ashp.org/Import/PRACTICEANDPOLICY/ PolicyPositionsGuidelinesBestPractices/BrowsebyDocumentType/TherapeuticGuidelines.aspx. Accessed July 10, 2012. 6. Guillamondegui OD, Gunter OL, Bonadies JA, et al. Practice management guidelines for stress ulcer prophylaxis. Eastern Association for the Surgery of Trauma.http://www.east.org/tpg/stressulcer.pdf. Published 2008. Accessed June 30, 2012. 7. Dellinger RP, Levy MM, Carlet JM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36(1):296-327. 8. Cook DJ, Reeve BK, Guyatt GH, et al. Stress ulcer prophylaxis in critically ill patients.JAMA. 1996;275(4):308-314. 9. Daley RJ, Rebuck JA, Welage LS, Rogers FB. Prevention of stress ulceration: current trends in critical care. Crit Care Med. 2004;32(10):2008-2013. 10. Barkun AN, Bardou M, Martel M. Proton pump inhibitors vs. histamine 2 receptor antagonists for stress-related mucosal bleeding prophylaxis in critically ill patients: a meta-analysis. Am J Gastroenterol. 2012;107(4):507-520. 11. Lin PC, Chang CH, Hsu PI, Tseng PL, Huang YB. The efficacy and safety of proton pump inhibitors vs histamine-2 receptor antagonists for stress ulcer bleeding prophylaxis among critical care patients: a meta-analysis. Crit Care Med. 2010;38(4):1197-1205. 12. Janarthanan S, Ditah I, Adler DG, Ehrinpreis MN. Clostridium difficile-associated diarrhea and proton pump inhibitor therapy: a meta-analysis. Am J Gastroenterol. 2012;107(7):1001-1010.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Smoking (Teaching Plan)Document28 pagesSmoking (Teaching Plan)SimeonDomingoTorresSy100% (1)
- Adult ADHD Self-Report Scale (ASRS-v1.1) Symptom ChecklistDocument2 pagesAdult ADHD Self-Report Scale (ASRS-v1.1) Symptom ChecklistMihaela VișanNo ratings yet
- The Tell-Tale Heart: Unnamed Man and His Defense MechanismsDocument6 pagesThe Tell-Tale Heart: Unnamed Man and His Defense MechanismsMasyita Rizkia RachmaNo ratings yet
- Philippines: Food Product and Safety RegulationDocument24 pagesPhilippines: Food Product and Safety RegulationCelrose FernandezNo ratings yet
- Sullivan's Interpersonal Model of Personality DevelopmentDocument42 pagesSullivan's Interpersonal Model of Personality DevelopmentPamDavidGabriel75% (4)
- Commentary Biowaiver Monographs For Immediate Release Solid Oral Dosage Forms: PrednisoloneDocument20 pagesCommentary Biowaiver Monographs For Immediate Release Solid Oral Dosage Forms: PrednisolonePrisca WicitaNo ratings yet
- Consumer Plan - Bear BrandDocument9 pagesConsumer Plan - Bear BrandJoyce Pablo67% (9)
- Audits of Emergency Trolleys' Contents in Selected Hospitals in BotswanaDocument8 pagesAudits of Emergency Trolleys' Contents in Selected Hospitals in BotswanaNthie UnguNo ratings yet
- Bilas LambungDocument12 pagesBilas LambungNthie UnguNo ratings yet
- Does Regular Repositioning Prevent Pressure UlcersDocument9 pagesDoes Regular Repositioning Prevent Pressure Ulcersnthie_unguNo ratings yet
- The Eschar Trial: Should It Change Practice?: David D. I. Wright, MB, BSC, FrcsDocument5 pagesThe Eschar Trial: Should It Change Practice?: David D. I. Wright, MB, BSC, FrcsNthie UnguNo ratings yet
- BMC Health Services ResearchDocument9 pagesBMC Health Services ResearchNthie UnguNo ratings yet
- National Pressure Ulcer Advisory Panel's Updated Pressure Ulcer Staging SystemDocument8 pagesNational Pressure Ulcer Advisory Panel's Updated Pressure Ulcer Staging SystemNthie UnguNo ratings yet
- Knowledge, Attitudes, Practices and Status of Oral Health Among Diabetic Patients at Kikuyu HospitalDocument2 pagesKnowledge, Attitudes, Practices and Status of Oral Health Among Diabetic Patients at Kikuyu HospitalNthie UnguNo ratings yet
- Oral Health & Diabetes: What Is Gum Disease?Document4 pagesOral Health & Diabetes: What Is Gum Disease?Nthie UnguNo ratings yet
- Album Find The Way-Sandhy SandoroDocument1 pageAlbum Find The Way-Sandhy SandoroNthie UnguNo ratings yet
- "Bundle" Up To Prevent Pressure UlcersDocument4 pages"Bundle" Up To Prevent Pressure UlcersNthie UnguNo ratings yet
- Herbs: (Caulophyllum Thalictroides)Document6 pagesHerbs: (Caulophyllum Thalictroides)Nthie UnguNo ratings yet
- Lifeline Supreme BrochureDocument5 pagesLifeline Supreme BrochureSumit BhandariNo ratings yet
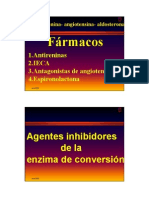
- Inhibidores de La ECADocument16 pagesInhibidores de La ECAFarmaFMNo ratings yet
- Treatment Efficacy Summary: Dysarthria (Neurological Motor Speech Impairment)Document1 pageTreatment Efficacy Summary: Dysarthria (Neurological Motor Speech Impairment)Mara CadinoiuNo ratings yet
- DAFTAR PUSTAKA Gangguan CemasDocument3 pagesDAFTAR PUSTAKA Gangguan CemaselsahewuniNo ratings yet
- Subtype Incidence Courde and Prognosis: 1. Risk Factors For NHLDocument5 pagesSubtype Incidence Courde and Prognosis: 1. Risk Factors For NHLKeepItSecretNo ratings yet
- Breast ImagingDocument14 pagesBreast ImagingMelissa TiofanNo ratings yet
- Question 1hDocument3 pagesQuestion 1hItharshan IndreswaranNo ratings yet
- CD 007154Document22 pagesCD 007154Anonymous m0vrFqAsNo ratings yet
- SDB Seifen eDocument4 pagesSDB Seifen eMathias CoekaertsNo ratings yet
- 2013 SC Decisions PDFDocument520 pages2013 SC Decisions PDFInes Hamoy JunioNo ratings yet
- Bell Palsy: Nelson Textbook of Pediatrics 19 EditionDocument11 pagesBell Palsy: Nelson Textbook of Pediatrics 19 EditionTommy YauNo ratings yet
- 1746 Pharma Biotech Water Requirements GBDocument2 pages1746 Pharma Biotech Water Requirements GBnavas1972No ratings yet
- Savings CardDocument1 pageSavings CardAvinash MalladhiNo ratings yet
- Barefoot Earthing (OnFitness Magazine)Document4 pagesBarefoot Earthing (OnFitness Magazine)JohanNo ratings yet
- Effectiveness of Myofunctional Therapy in Ankyloglossia: A Systematic ReviewDocument18 pagesEffectiveness of Myofunctional Therapy in Ankyloglossia: A Systematic Reviewmistic0No ratings yet
- The Benefit of Heat and Moisture Ex Changers Corrected)Document27 pagesThe Benefit of Heat and Moisture Ex Changers Corrected)Liew Hock Man CindyNo ratings yet
- Eblr Paper-1 2Document8 pagesEblr Paper-1 2api-536557582No ratings yet
- Dosis Oseltamivir CDCDocument3 pagesDosis Oseltamivir CDCivonne marinNo ratings yet
- Sand Brochure July 2016Document2 pagesSand Brochure July 2016Jack CianfaglioneNo ratings yet
- Flyer Ascnp-Asean 3rd Announcement USDDocument2 pagesFlyer Ascnp-Asean 3rd Announcement USDAmaliYah ILmNo ratings yet
- Perianal Surgical Conditions: Fitsum ArgawDocument51 pagesPerianal Surgical Conditions: Fitsum ArgawWorku KifleNo ratings yet
- SaravanaDocument21 pagesSaravanaRasu Kutty100% (1)