Professional Documents
Culture Documents
Advanced Cardiac Life Support
Advanced Cardiac Life Support
Uploaded by
dendikarmenaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Advanced Cardiac Life Support
Advanced Cardiac Life Support
Uploaded by
dendikarmenaCopyright:
Available Formats
Advanced Cardiac Life Support
Basic Life Support Algorithm Assess Responsiveness No movement or response Call for code team and Defibrillator Open the airway, look, listen and feel for breathing) If Not Breathing, give 2 breaths that make chest rise Check pulse PULSE Give oxygen by bag mask. One breath every 5 to 6 seconds. Recheck pulse every 2 minutes Secure IV access Determine probable etiology of arrest based on history, physical exam, cardiac monitor, vital signs, and 12 lead ECG. Hypotension/shock, acute pulmonary edema. Go to fig 5 NO PULSE Initiate CPR at cycles of 30 compressions and 2 breaths until defibrillator arrives.
Defibrillator arrives. Check Rhythm Shockable rhythm? Shockable
Not shockable Asystole or Pulseless Electrical Activity Go to Fig 2
Arrhythmia
Ventricular Tachycardia or Ventricular Fibrillation Go to Fig 2
Bradycardia Go to Fig 3
Tachycardia Go to Fig 4
Fig 1 - Basic Life Support Algorithm
PULSELESS ARREST 1 Assess Airway, Breathing, Circulation, Differential Diagnosis; call for help Give CPR and oxygen Attach monitor/defibrillator Shockable 3 Ventricular Fibrillation or Ventricular Tachycardia 4 Give 1 shock Manual biphasic: 120-200 J Monophasic: 360 J Resume CPR 5 Give 5 cycles of CPR No 2 Check rhythm Shockable rhythm? Not Shockable 9 Asystole or Pulseless Electrical Activity 10 Resume CPR for 5 cycles When IV/IO available, give vasopressor Epinephrine 1 mg IV/IO or May give 1 dose of vasopressin 40 U IV/IO to replace first or second dose of epinephrine Consider atropine 1 mg IV/IO for asystole or slow PEA rate. Repeat every 3 to 5 min, up to 3 doses Give 5 cycles of CPR Check rhythm Shockable rhythm?
Check rhythm Shockable rhythm?
Shockable 6 Continue CPR Give 1 shock Manual biphasic: same as first shock or higher dose Monophasic: 360 J Resume CPR Give vasopressor during CPR Epinephrine 1 mg IV/IO. Repeat every 3 to 5 min or May give 1 dose of vasopressin 40 U IV/IO to replace first or second dose of epinephrine Give 5 cycles of CPR 7 No Check rhythm Shockable rhythm? 8 Shockable
If asystole, go to Box 10 If electrical activity, check pulse. If no pulse, go to No box 10 Ifpulse present, begin postresusitation care
Shockable Go to Box 4
Continue CPR Give 1 shock Manual biphasic: Same as first shock or higher dose. Monophasic: 360 J Resume CPR Consider antiarrhythmicsduring CPR: Amiodarone 300 mg IV/IO once, then 150 mg IV/IO once or Lidocaine 1-1.5 mg/kg first dose, then 0.5 to 0.75 mg/kg IV/IO, max 3 doses or 3 mg/kg Consider magnesium, loading dose 1 to 2 g IV/IO for torsades de pointes After 5 cycles of CPR, go to box 5 above
Fig 2 - Pulseless Arrest Algorithm
BRADYCARDIA
Bradycardia (<60 beats/min) and inadequate for clinical condition
Maintain patent Airway, assist Breathing as needed Give oxygen Monitor ECG, pulse oximeter and blood pressure
Secure IV access Review history
Signs or symptoms of Poor Perfusion caused by bradycardia? (eg, onfusion, delirium, lethargy, chest pain, hypotension or other signs of shock) Adequate Perfusion Observe and Monitor
Poor Perfusion
Reminders If pulseless arrest develops, go to Pulseless Arrest Algorithm Search for and treat possible contributing factors: Hypovolemia Hypoxia Hydrogen ion (acidosis) Hypo/hyperkalemia Hypoglycemia Hypothermia Toxins Tamponade, cardiac Tension pneumothorax Thrombosis (coronary or pulmonary) Trauma (hypovolemia, increased ICP)
Initiate transcutanous pacing for highdegree block (type II second or 3rd degree heart block, wide complex escape beats, MI/ischemia, denervated heart (transplant),new bundle branch block) Consider atropine 0.5 mg IV, repeat q5min to a total dose of 3 mg. Initiate pacing if bradycardia continues. Consider epinephrine 2-10 mcg/min IV infusion or dopamine 2-10 mcg/kg per min IV infusion while awaiting pacer or if pacing ineffective
Initiate transvenous pacing Treat contributing causes Obtain cardiology consultation
Fig 3 - Bradycardia Algorithm (with patient not in cardiac arrest).
TACHYCARDIA With Pulses Assess and support Airway, Breathing, Circulation Give 100% oxygen Monitor ECG and identify rhythm. Monitor oximeter, blood pressure Identify and treat reversible causes Review history and examine patient
Is the patient stable? Unstable includes, hypotension, heart failure, chest pain, decreased mental status, or other signs of shock Stable
Unstable
IMMEDIATE SYNCHRONIZED CARDIOVERSION Establish IV access and give midazolam (Versed) 2-5 mg IVP if patient is conscious; do not delay cardioversion Cardiovert atrial flutter with 50 J, paroxysmal supraventricular tachycardia 50 J, atrial fibrillation 100 J, monomorphic ventricular tachycardia100 J. Polymorphic V tachycardia 360 J unsynchronized. If pulseless arrests develops, see Pulseless Arrest Algorithm, figure 2.
Establish IV access Obtain 12-lead ECG Is QRS narrow (<0.12 sec)? Wide ( $0.12 sec) Narrow NARROW QRS: Is Rhythm Regular? Regular Irregular WIDE QRS: Is Rhythm Regular? Regular Irregular
Attempt vagal maneuvers Give adenosine 6 mg rapid IV push. If no conversion, give 12 mg rapid IV push; may repeat 12 mg dose once
Irregular Narrow-Complex Tachycardia Probable atrial fibrillation or possible atrial flutter or multifocal atrial tachycardia Control rate (eg, diltiazem, betablockers)
If ventrucular tachycardia or uncertain rhythm Amiodarone 150 mg IV over 10 min. Repeat as needed to max 2.2 g/24 hours Prepare for elective synchronized cardioversion If SVT with aberrancy Give adenosine 6 mg, rapid IV push (may repeat 12 mg once)
Does rhythm convert? Converts Does Not Convert
If atrial fibrillation with aberrrancy See Irregular Narrow-Complex Tachycardia If pre-excited atrial fibrillation (AF + WPW) Avoid AV nodal blocking agents (eg, adenosine, digoxin, diltiazem, verapamil) Consider amiodarone150 mg IV over 10 min If recurrent polymorphic VT, seek cardiology consultation If torsades de pointes, give magnesium load of 1-2 g over 560 min, then infuse 3-10 mg/min for 7-48h
If rhythm converts, probable reentry supraventricular tachycardia: Observe for recurrence Treat recurrence with adenosine or longer-acting AV nodal blocking agents (eg, diltiazem, betablockers)
If rhythm does NOT convert, possible atrial flutter, ectopic atrial tachycardia, or junctional tachycardia: Control rate (eg diltiazem, beta-blockers) Treat underlying cause
Treat contributing factors: Hypovolemia Hypoxia Hydrogen ion (acidosis) Hypo/hyperkalemia Hypoglycemia Hypothermia
Toxins Tamponade, cardiac Tension pneumothorax Thrombosis (coronary or pulmonary) Trauma (hypovolemia, increased ICP)
Figure 4 Tachycardia With Pulses
Acute Coronary Syndromes Algorithm Chest discomfort suggestive of ischemia
Immediate Emergency Department Assessment Check vital signs; evaluate oxygen saturation Establish IV access Obtain/review 12-lead ECG Perform brief, targeted history, physical exam Complete fibrinolytic checklist; check contraindications Obtain initial cardiac marker levels, initial electrolyte and coagulation studies Obtain portable chest x-ray
Immediate Emergency Department treatment Oxygen at 4 L/min; maintain O2 sat >90% Aspirin 160-325 mg (if not given by EMS) Nitroglycerine sublingual spray, or IV Morphine IV if pain not relieved by nitroglycerine
Review initial 12-lead ECG
ST elevation or new or presumably new LBBB; strongly suspicious for injury ST-Elevation MI (STEMI)
ST depression or dynamic T-wave inversion; strongly suspicious for ischemia High-Risk Unstable Angina/ Non-ST-Elevation MI (UA/NSTEMI)
Normal or nondiagnostic changes in ST segment or T wave Intermediate/Low-Risk Unstable Angina
Start adjunctive treatments as indicated Do not delay reperfusion beta-Adrenergic receptor blockers Clopidogrel Heparin (unfractionated or low molecular weight heparin)
Start adjunctive treatments as indicated Nitroglycerine beta-Adrenergic receptor blockers Clopidogrel Heparin (unfractionated or low molecular weight heparin) Glycoprotein IIb/IIIa inhibitor
Develops high or intermediate risk criteria (refractory chest pain, pulmonary edema, mitral regurgitation, hypotension, etc) OR Troponin-positive
Time from onset of symptoms #12 hours? #12 hours
$12 hours
Admit to monitored bed Assess risk status
Consider admission to ED chest pain unit or to monitored bed in ED Follow: Serial cardiac markers (including troponin) Repeat ECG/continuous ST segment monitoring Consider stress test
Reperfusion strategy Reperfusion goals: Door-to-balloon inflation (PCI) goal of 90 min Door-to-needle (fibrinolysis) goal of 30 min Continue adjunctive therapies and: ACE inhibitors/angiotensin receptor blocker within 24 hours of symptom onset HMGCoA reductase inhibitor (statin)
High-risk patient Refractory ischemic chest pain Recurrent/persistent ST deviation Ventricular tachycardia Hemodynamic instability Signs of pump failure Early invasie strategy, including catheterization and revascularization for shock within 48 hours of an AMI Continue ASA, heparin, and other therapies as indicated. ACE inhibitor/ARB HMGCoA reductase inhibitor (statin)
Develops high or intermediate risk criteria (refractory chest pain, pulmonary edema, mitral regurgitation, hypotension, etc) OR Troponin-positive
If no evidence of ischemia or infarction, can discharge with follow-up
Figure 6 - Acute Coronary Syndromes Algorithm
HYPOTENSION,SHOCK,ANDACUTEPULMONARYEDEMA Signs and symptoms of congestive heart failure, acute pulmonary edema. Assess ABCD's, secure airway, administer oxygen; secure IV access. Monitor ECG, pulse oximeter, blood pressure, order 12-lead ECG, portable chest X-ray Check vital signs, review history, and examine patient. Determine differential diagnosis. Determine underlying cause
Hypovolemia Administer Fluids, Blood Consider vasopressors Apply hemostasis; treat underlying problem
Pump Failure Determine blood pressure Systolic BP >100 mm Hg and diastolic BP normal Dobutamine 2.0-20 mcg/kg per min IV Furosemide IV 0.5-1.0 mg/kg Morphine IV 1-3 mg Nitroglycerin SL 0.4 mg tab q3-5min x3 Oxygen
Bradycardia or Tachycardia Bradycardia Go to Fig 3 Tachycardia Go to Fig 4
Systolic BP <70 mm Hg
Systolic BP 70-100 mm Hg
Diastolic BP >110 mm Hg
Norepinephrine 0.530 mcg/min IV or Dopamine 5-20 mcg/kg per min
Dopamine 2.5-20 mcg/kg per min IV (add norepinephrine if dopamine is >20 mcg/kg per min)
If ischemia and hypertension: Nitroglycerin10-20 mcg/min IV, and titrate to effect and/or Nitroprusside 0.1-5.0 mcg/kg/min IV
Figure 6 - Hypotension, Shock, and Acute Pulmonary Edema
You might also like
- AHA ELearning ACLS Precourse Self-Assessment and Precourse WorkDocument1 pageAHA ELearning ACLS Precourse Self-Assessment and Precourse Work9kjsntkrzcNo ratings yet
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsFrom EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsNo ratings yet
- ACLS MneumonicsDocument4 pagesACLS MneumonicsnaranothNo ratings yet
- Algorithm-ACLS Electrical Cardioversion 200612Document1 pageAlgorithm-ACLS Electrical Cardioversion 200612Kavya ShreeNo ratings yet
- Oral Station Scenario PDFDocument3 pagesOral Station Scenario PDFlotuss45No ratings yet
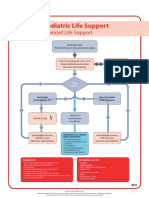
- Pediatric Advanced Life Support: I. PALS System Approach AlgorithmDocument19 pagesPediatric Advanced Life Support: I. PALS System Approach AlgorithmIsabel Castillo100% (1)
- SureFire CPR NRP Study GuideDocument18 pagesSureFire CPR NRP Study GuidelykaNo ratings yet
- Acls DrugsDocument10 pagesAcls DrugsChintami Octavia100% (1)
- Commonly Used IV Cardiac Medications For Adults Pocket Reference Card PDFDocument12 pagesCommonly Used IV Cardiac Medications For Adults Pocket Reference Card PDFYannis Zoldenberg100% (1)
- ECG TipsDocument7 pagesECG TipsMar Kristian Vero Lumen100% (1)
- General ConceptsDocument18 pagesGeneral ConceptsMoxie MacadoNo ratings yet
- Drip ChartDocument10 pagesDrip Chartmirzaocta100% (1)
- Acls Pharmacology OverviewDocument11 pagesAcls Pharmacology OverviewzoyaligNo ratings yet
- Shock: Shout For Help/Activate Emergency ResponseDocument6 pagesShock: Shout For Help/Activate Emergency ResponseandiyanimalikNo ratings yet
- ACLS Simplify AlgorithmDocument6 pagesACLS Simplify AlgorithmKristine Monforte Coma UritaNo ratings yet
- PalsDocument1 pagePalslordroentgenNo ratings yet
- Torsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandTorsade De Pointes, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Advanced Cardiac Life Support Quick Study Guide 2015 Updated GuidelinesFrom EverandAdvanced Cardiac Life Support Quick Study Guide 2015 Updated GuidelinesRating: 4 out of 5 stars4/5 (6)
- Pediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesFrom EverandPediatric Advanced Life Support Quick Study Guide 2015 Updated GuidelinesRating: 5 out of 5 stars5/5 (2)
- Cardiac Arrest, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCardiac Arrest, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- ECG & EKG Interpretation: How to interpret ECG & EKG, including rhythms, arrhythmias, and more!From EverandECG & EKG Interpretation: How to interpret ECG & EKG, including rhythms, arrhythmias, and more!No ratings yet
- EKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!From EverandEKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!No ratings yet
- Abnormal Slow Heart Beats, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandAbnormal Slow Heart Beats, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Heart Block, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHeart Block, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Rhythm Recognition - ACLS Medical Training 1Document9 pagesRhythm Recognition - ACLS Medical Training 1Catalina BorquezNo ratings yet
- ACLS Test Sinus BradycardiaDocument1 pageACLS Test Sinus BradycardiaFiya Sahrul0% (1)
- Cardiovascular Assessment Pocket Reference Card PDFDocument8 pagesCardiovascular Assessment Pocket Reference Card PDFerikaNo ratings yet
- ACLS Official GuideDocument11 pagesACLS Official GuideICU RSPGNo ratings yet
- Acls Drug OverviewDocument2 pagesAcls Drug OverviewShannon Davis100% (1)
- ACLS Study GuideDocument28 pagesACLS Study GuideNicole Berry100% (1)
- American Heart Association Guidelines For CPR 2015: Christopher RyalinoDocument50 pagesAmerican Heart Association Guidelines For CPR 2015: Christopher RyalinoLightNo ratings yet
- ACLS Training - Most Important Points To RememberDocument5 pagesACLS Training - Most Important Points To RememberEman ElzeftawyNo ratings yet
- ACLS PharmacologyDocument5 pagesACLS PharmacologyKuruva MallikarjunaNo ratings yet
- Dysrhythmia Advance Content Outline A1 - 2020.1.2Document3 pagesDysrhythmia Advance Content Outline A1 - 2020.1.2Kimberly Whiteside50% (2)
- ACLS Study Guide: Ecg Strip InterpretationDocument12 pagesACLS Study Guide: Ecg Strip InterpretationMariana Berger100% (1)
- (Advanced Cardiac Life Support) : ACLS Algorithms 2018Document18 pages(Advanced Cardiac Life Support) : ACLS Algorithms 2018cristina100% (1)
- ToxidromesDocument1 pageToxidromesMayer Rosenberg100% (7)
- Basic EKG InterpretationDocument4 pagesBasic EKG InterpretationPRaDo PATNo ratings yet
- Basic EKG Interpretation Exam AnswersDocument3 pagesBasic EKG Interpretation Exam AnswerstwdroppointNo ratings yet
- Megacode Testing Checklist Scenarios 4-7-10 Tachycardia, VF, PEA, PC...Document1 pageMegacode Testing Checklist Scenarios 4-7-10 Tachycardia, VF, PEA, PC...krgduraiNo ratings yet
- How To Read An ECGDocument21 pagesHow To Read An ECGSlychenkoNo ratings yet
- CPR ACLS Study GuideDocument18 pagesCPR ACLS Study GuideJohn Phamacy100% (1)
- Nervous System AlterationsDocument45 pagesNervous System AlterationsMajesty ParkerNo ratings yet
- ACLS ScenarioDocument21 pagesACLS Scenariomarves15No ratings yet
- ICU Rounding Template - v. WebsiteDocument2 pagesICU Rounding Template - v. Websitepattumkp0% (1)
- Post-ACLS Megacode Flashcards - QuizletDocument9 pagesPost-ACLS Megacode Flashcards - QuizletMaya LaPrade100% (1)
- Critical Care Admission OrdersDocument6 pagesCritical Care Admission OrdersTariq Niaz Ahmad, MDNo ratings yet
- AHA ACLS Written Test: Ready To Study? Start With FlashcardsDocument8 pagesAHA ACLS Written Test: Ready To Study? Start With Flashcardssally100% (1)
- Acls Drug OverviewDocument2 pagesAcls Drug OverviewBruce Abramowitz100% (1)
- Poster 10 PALS 01 01 ENG V20100927 PDFDocument1 pagePoster 10 PALS 01 01 ENG V20100927 PDFAndy XiaoNo ratings yet
- 15 Item Acls DrillDocument4 pages15 Item Acls DrillVal SolidumNo ratings yet
- 409 Pope, B. and Maillie, S. CCRN-PCCN Review Multisystem and Q and ADocument21 pages409 Pope, B. and Maillie, S. CCRN-PCCN Review Multisystem and Q and Agliftan100% (2)
- ACLS Algorithm Pulse No Yes: Stable Patient Unstable Patient Stable PatientDocument1 pageACLS Algorithm Pulse No Yes: Stable Patient Unstable Patient Stable PatientAhmed AlkhaqaniNo ratings yet
- ACLS ChartDocument1 pageACLS ChartJev DespiNo ratings yet
- Emergency Lecture PDFDocument57 pagesEmergency Lecture PDFDuane Liloc100% (1)
- LSCPR Pals Study Guide 2020Document57 pagesLSCPR Pals Study Guide 2020Juan Ma100% (1)
- EKG - Basic Interpretation and ACLS PreparationDocument39 pagesEKG - Basic Interpretation and ACLS PreparationSergio Cano100% (2)
- Intubation ChecklistDocument2 pagesIntubation ChecklistDaniel CrookNo ratings yet
- PCM Guidebook For History Taking and Physical Exam, Revised Final, 9-20-17Document82 pagesPCM Guidebook For History Taking and Physical Exam, Revised Final, 9-20-17anon_925247980No ratings yet