Professional Documents
Culture Documents
Versatile Class Lectures on Urinary System and Kidney Disorders
Uploaded by
rohishaakOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Versatile Class Lectures on Urinary System and Kidney Disorders
Uploaded by
rohishaakCopyright:
Available Formats
A Versatile Look of Class Lectures Path-202
CLASS LECTURES EFFECTIVE FOR ALL THE FOUR SECTIONS (A+B & C+D)
Path-202 / FINAL
COMPILED BY M. SAJJAD HUSSAIN msh.03226272278@gmail.com
URINARY SYSTEM
A+B:27/04 LECTURE 11(Continued) C+D:27/04
11.1. URINARY SYSTEM
The urinary system consists of; i) ii) iii) iv) Two kidneys Two ureters Urinary bladder Urethera
11.1.1. STRUCTURES ASSOCIATED WITH A KIDNEY i) Renal capsule ii) Cortex iii) Medulla iv) Calyx v) Renal pyramids vi) Renal crest vii) Renal pelvis viii) Renal artery ix) Renal vein x) Arcuate artery xi) Renal fat. 11.1.2. STRUCTURES ASSOCIATED WITH A NEPHRON i) Efferent vessel ii) Afferent vessel iii) Bowmans capsule iv) Glomerulus v) Bowmans space vi) Proximal convulated tubule vii) Proximal straight tubule viii) Loop of Henley ix) Distal straight tubule x) Distal convulated tubule xi) Collecting duct.
11.2. CONGENITAL ANOMALIES OF KIDNEYS
1. RENAL APLASIA OR AGENESIS It is the failure of development of one or both kidneys but there may be absent or presence of ureter also along with. If a single kidney is absent then the respective ureter begins as a blind pouch. Unilateral renal aplasia may remain undetected for a longer time. 2. RENAL HYPOPLASIA It indicates the incomplete or partial development of kidney in which there would be a fewer number of nephrones and calyxes at birth. In bovines, there may be absence or decreased number of tubules. 3. RENAL DYSPLASIA It is an abnormality of altered structural organization resulting from abnormal differentiation.
Microscopically: There is persistence of primitive mesenchyma, Interstitial fibrosis, renal cysts and few enlarged hypercellular glumeruli. 4. ECTOPIC KIDNEYS (FUSED KIDNEYS) It is the fusion of cranial or caudal poles of the kidneys during nephrogenesis which result in appearance of one large/Giant kidney with two ureters. 5. POLYCYSTIC KIDNEY In this condition, kidney have many cysts that involved numerous nephrones. Such kidneys can have Swiss Cheese appearance when incised. CYST: Fluid-filled cavity is known as a cyst. As cyst enlarged, it compressed the adjacent parenchyma that ultimately leading to renal failure or impairment of kidneys. As there is an obstruction in the nephrone, then there is increased luminal pressure and a secondary dilatation that results into modifications in the matrix and weakened the tubular basement membrane. It (obstruction) allowing the secular dilatation of tubules. There is focal tubular hyperplasia. Increased intra-tubular pressure causes development of enlarged dilated tubules.
A+B:28/04
LECTURE 12
C+D:28/04
12.1. CIRCULATORY DISTURBANCES
The circulatory disturbances involve the following; 1) HEMORRHAGES: The hemorrhages over the kidneys may be classified into three types; a) Patachial hemorrhages: The most common type of such hemorrhages is renal cortical hemorrhage. It often appears due to septicemia, which may occur due to any bacterial infection (like Streptococcus and Salmonella infections). b) Echymotic hemorrhages Such type of hemorrhages indicates the multifocal tubular and vascular necrosis. These are commonly observed in Herpes-virus infection. c) Large spot/Intrarenal/Subcapsular hemorrhages: It may be due to i) Direct trauma ii) Renal biopsy iii) Bleeding disorders iv) DIC (disseminated intravascular coagulatibility)
2) CONGESTION: Kidneys are usually dark in color, red, swollen. When cut, there is oozing of blood. Sometime there is unilateral hypostatic congestion in animals and it died on lateral recumbency.
12.2. RENAL INFARCT
Definition: It is the area of coagulative necrosis that results from local ischemia and usually due to thrombo-embolism and aseptic emboli. Diagnostic Features: i) There is ischemic necrosis of local area of kidney. ii) It may be single or multiple. iii) Infarct area is wedge shaped iv) The base of wedge shaped area is towards the cortical region v) The apex of this area is towards the medulla. GROSSLY: 1. Renal infarct usually appears red or pale white depending on several factors including; i) interval after vascular occlusion, ii) Whether an artery or a vein is occluded. 2. Occlusion of arteries results in infarct that is initially hemorrhagic and slightly swollen. 3. It turned pale to yellow grey within 2-3 days, because of lysis of RBCs and loss of Hb. 4. Pale infarct has a central area of coagulative necrosis and usually surrounded by a zone of congestion and hemorrhages along with pale margin because of surrounded zone of leukocytes. 5. Infarcts are often wedge-shaped with base against the cortical surface and apex pointing towards the medulla. MICROSCOPICALLY: 1. Nephrones and interstitium in central zone of infarct becomes necrotic. 2. Glumeruli tend to be spread along the margin of the necrotic zone. 3. Area is infiltrated initially with the neutrophils, few macrophages and lymphocytes. 4. Capillaries adjacent to the necrotic area are markedly engorged with blood. 5. Healing of infracted area occur by lysis and phagocytosis of necrotic tissue and also replacement by fibrous connective tissue, leaving a discrete fibrotic scar. 6. Scars arranged from linear to broader fashion depending on the size of acute infarct. ETIOLOGY/CAUSES Renal infarct may occur as a result of (due to) theses diseases: i) Vegetative vulvitis ii) Embolic obstruction iii) Strongylus vulgaris iv) Thrombosis
v) Renal amyloidosis
12.3. NEPHRITIS
It is the inflammation of the kidney. FORMS OF NEPHRITIS It may be of various forms/types i) Glomerular nephritis ii) Tubular nephritis iii) Glomerulo-tubular nephritis iv) Interstitial nephritis
12.4. GLUMERULAR NEPHRITIS
It could be of many types depending upon the duration. i) Acute ii) Subacute iii) Chronic iv) Diffused or local 12.4.1. ACUTE GLOMERULAR NEPHRITIS It is an inflammatory condition effecting the glumeruli primarily but secondarily damages the other part of the nephrone as well as interstitial tissues later. GROSSLY: i) Kidney is swollen, capsule dense and somewhat stretched. ii) When kidney is incised, renal substances bulges and numerous thread like rods corresponding to petechial hemorrhages into the capsular space. MICROSCOPICALLY: 1. Acute inflammatory exudate is accumulated in the interstitial tissue and mesengium. 2. There is edema and swelling of endothelium of capillary loop. 3. Mesengium becomes widen and resulting compression of capillaries and great ischemia of glomerulus. 4. Greatly increased in cellularity of tuft as well as swelling and multiplication of epithelium of tuft. 5. Later, this epithelium desquamated and cast off into capsular space. 6. Polymorphs leukocytes collect in large number in the glomerular capillaries and in capsular space which then, passes into the urine.
A+B:29/04
LECTURE 13
C+D:29/04
13.1. SUBACUTE GLOMERULAR NEPHRITIS
GROSSLY: i) Kidney is considerably large (Large white kidney). The consistency is very soft.
ii) Capsule strips easily and exposed surface is smooth and pale while the cut surface show marked swelling and paler of the cortex. iii) Pyramids appear dark, pale due to great accumulation of lipids in cells of convulated tubules. iv) There may be bright yellow streaks & patches in the cortex region due to large deposits of lipids. MICROSCOPICALLY: 1. Glomeruli show an extreme cellularity which is highly characteristic. 2. There is more proliferation of epithelial and endothelial cells of tufts. 3. The epithelial cells proliferation is referred as Extra-capillary glomerular nephritis: 13.1.1. Extra capillary Glomerular Nephritis: i) In this condition (ECGN), epithelium of bowmans capsule proliferate so that large masses of cells occupy the capsular space. ii) The whole circumference of a glomerulus is involved, so cell form a semilunar mass in capsular space which is known as epithelial crescent. iii) RBCs, desquamated epithelium and fibrin mass is present in capsular space in varying amount. iv) During the coarse of time, crescent becomes fibrosed and fused with the tuft which also under hyalinization. 13.1.2. Intra capillary Glomerular Nephritis i) there are few or more cells in capsular space but there is a great proliferation of endothelial cells which give the tuft a highly cellular appearance. ii) Diffused, homogeneous thickening of capillary basement membrane ! also referred as <Membranous glomerular nephritis>. iii) There is remarkable increase in glomerular permeability especially for protein. iv) Tubules show marked degenerative changes such as fatty degeneration, cloudy swelling. v) As tubular degeneration progresses, many of epithelial cells cast off and tubules become atrophic. 13.1.4. CONSEQUENCES OF RENAL DISEASES (Generally) 1. There is a leakage of various low molecular weight protein into the glomerular filterate and subsequently into the urine. 2. Protein rich glomerular filtrate accumulated in the tubular lamina and subsequently appears in the urine. 3. There is a fusion of visceral epithelium and form a structure called podcyte. 4. As a result, there is a thickening of basement membrane and neutrophilic infiltration. 5. There is hypertrophy of endothelium as well as dense granular deposits of immune complex associated with basement membrane.
13.2. CHRONIC GLOMERULAR NEPHRITIS
GROSSLY: i) Kidney is small and shriveled with surface covered with fine granules entirely. ii) Renal capsule is so adherent that it is stripped off and portion of cortex may come away with it (Decortication). iii) Cut surface of the kidney shows extreme irregularity and atrophy of cortex. MICROSCOPICALLY: 1. There is a complete loss of renal architecture. 2. Renal parenchyma has been replaced with chief substitutes of fibrous tissues with few scattered glomeruli. 3. Glomeruli show extensive hyalinization. 4. Due to disappearance of tubules and shrinkage of cortex, there may be large number of hyaline glomeruli. 5. Glomuruli are atrophic, shrinken, but the capillaries still may give the passage to some blood. 6. Convulated tubules show an extreme degree of atrophy and only the outline may be detected under high resolution.
A+B:04/05
LECTURE 14
C+D:04/05
14.1. VIRAL GLOMERULAR NEPHRITIS
The glomerular lesions may occur in certain viral diseases such as: i) Acute infectious canine hepatitis ii) Septicemic cytomegalovirus infection iii) Equine arteritis virus infection iv) New castle disease (in birds). LESIONS: 1. The Lesions are mild and result from the viral replication in the capillary endothelium. 2. Viral induced intranuclear inclusions are present in glomerular capillaries & endothelium. 3. Inclusion bodies are usually large, basophilic (magenta color) and either fill the nucleus or separated from the nuclear membrane by clear hallow. 4. Viral antigen can be demonstrated in the endothelium, epithelium or Mesengial cell through immunovytochemistry.
14.2. RENAL AMYLOIDOSIS
What is Amyloid:
It is an insoluble, fibril protein with a beta pleated sheath conformation, produced after incomplete proteolysis of several soluble amyloidogenic proteins. Amyloid protein deposits are composed of fragments of serum acute phase reactant protein called as Serum Amyloid Associated (SAA) protein. Sometime, Amyloid fibril from either source are deposited in the tissues along with glycoprotein called Amyloid P-component. 14.2.1. Site of Deposition of Amyloid The Glomerulus is the most common renal site for deposition of Amyloid. 14.2.2. GLOMERULAR AMYLOIDOSIS It is a protein loss nephropathy resulting in marked protein urease and uremia. GROSSLY: i) Kidney is enlarged, pale tan to yellow and have smooth to finally granular capsular surface. ii) Amyloid laden glomeruli can be visible as fined dots on the cut surface. iii) Cortex can have finally granular appearance, but if treated with I2 solution, result in brown staining of glomeruli that become purple when exposed to H2SO4. MICROSCOPICALLY 1. There are Glomerular Amyloid deposits in the mesengium and subendothelial location. 2. The Amyloid is usually acellular and accumulate segmently within a glomerular tuft, thus replaced the normal architecture by eosinophilic, homogenous to slightly fibrilar matrix. 3. Glomeruli enlarged, capillary lumina become obliterated and tuft can appears as a large hypercellular eosinophilic hyaline sphere. 4. Tubulo-basement membrane may become hyalinized and thickened. 5. Renal tubules are markedly dilated and contain proteinous material. 6. Amyloid is conformed with Congo Red (green) stain.
14.3. INTERSTITIAL NEPHRITIS
It is also termed as tubulo-interstitial nephritis. It is a disease in which the aggregates of inflammatory cells can be present in the renal interstitium, in various systemic infectious diseases of domestic animals like: i) In Dog: Leptospira infection, Icterohemorrhagiae and Infectious Canine hepatitis. ii) In Cattle: E.coli septicemia, Malignanat catarrhal fever (MCF), Theleria parva inf. iii) In Horse: Equine viral arteritis, Equine Infectious anemia. iv) In Sheep: Sheep pox infection. 14.3.1. FORMS OF INTERSTITIAL NEPHRITIS: It may be i) Acute ii) Subacute iii) Chronic. Either it may be i) Diffused ii) Focal In Case of Diffused Interstitial Nephritis:
GROSSLY i) Kidney is swollen, and pale in color. ii) Cut surface bulges, there may be grey infiltrate of varying amount and intensities which obscure normally, readily striated cortical architecture. iii) Predominantly, grey foci are present in the cortical surface but sometime, it may occur in the outer medullary region. MICROSCOPICALLY 1. The aggregates of lymphocytes, plasma cells, monocytes and few neutrophils are randomly scattered or intensely localized throughout the interstitium. 2. Degenerated necrotic tubular epithelium (DNTE) is a distinguishable characteristic.
14.4. GRANULOMATOUS NEPHRITIS
It is characterized by the multiple granulomas in the kidneys. It is associated with a variety of infectious agents i.e. viruses, bacteria, fungi, parasites etc. i) Viral Infections: - Faline infectious peritonitis - Encephaliozoon tuniculi (In case of dog) ii) Bacterial Infections: - Mycobacterium tuberculosis iii) Fungal infections: - Aspergilosis iv) Parasitic Infections: - Toxocara canis
A+B:05/05
LECTURE 15
C+D:05/05
15.1. PYELITIS: inflammation of the pelvis of the kidney. 15.2. PYELONEPHRITIS: Inflammation of the both pelvis and renal parenchyma (kidney
itself). ETIOLOGY: It mostly occur due to: i) ascending infections of the urinary tract ii) Abnormal reflex of urine contaminated with the bacteria (vesico-uretral reflex) Other most common causative agents are: i) E. coli iv) Proteus ii) Corynebacterium renale iii) Klebsiella v) Pseudomonas aureginosa
Pyelitis may be unilateral or bilateral but often it is bilateral.
GROSSLY i) Mucus membrane is inflamed, thickened , reddened, roughened and granular. ii) It is coated with purulent exudate iii) Pelvis and ureter are markedly dilated and present purulent exudate in their lumina. iv) Medullary crests or papillae are ulcerated and necrotic. MICROSCOPICALLY 1. Most common and severe lesions of pyelonephritis are usually in the inner medulla. 2. Transitional epithelium usually necrotic and desquamated. 3. Necrotic debris, fibrin, neutrophils and bacterial colonies can be adherent to denuded area -< seems to have a look of filled exudate.
15.3. HYDRONEPHROSIS
It refers to dilatation of renal pelvis due to obstruction of urine outflow and it increased the pelvis pressure, dilatation of pelvis and progressive renal parenchymal atrophy. ETIOLOGY/CAUSATIVE AGENTS 1) The urine outflow may be stopped due to i) tumor ii) Stone formation, so urine can accumulate in the kidney and cysts formation occur that leads to atrophy of the parenchyma. 2) Congenital absence or malformation of ureter(s). 3) Chronic inflammation of urinary tract that leads to Neoplasia in ureter and urethra. 4) Congenital malposition of kidney(s). GROSSLY i) Dilatation of the pelvis and calyxs ii) Kidney(s) become(s) enlarged with rounded extremitites. iii) Cortex and medulla are progressively thin. iv) Hydronephrotic kidneys are thin walled and contain fluid filled sac. v) Occasionally, such kidney may become contaminated by bacteria and thin walled sac becomes filled with pus instead of urine. Such type of lesion is known as Pyonephritis. MICROSCOPICALLY 1. There is a loss of tubules by degeneration and atrophy followed by condensation of interstitial connective tissue and fibrosis of renal parenchyma. 2. The thin sac is lined by flattened transitional epithelium.
15.4. RENAL CALCULUS
SYN: Nephrolethiasis. Stone formation in the kidney is termed as nephrolethiasis. FORMS OF CALCULUS
The stone (calculus) may single or multiple. It may presents variable color depending upon the salt deposited. Such as: i) White to grey stone: indicated deposition of oxalalate. ii) Yellow stone: indicates deposition of urate, cystine, xanthene and benzocumorin. ii) Brown stone: indicates deposition of silica, urate and xanthene. 15.4.1. DEVELOPMENT OF CALCULUS Renal calculus consists of nucleus of organic material around which the urinary salt is deposited in several concentric layers which are bound together by colloidal matrix of organic matter. During its passage, calculus excites violent spasmatic contrations which are responsible for pain of the kidney (also named as renal colic). Bacterial colony (known as nidus) is responsible for the salt deposition. It may lodges in the pelvis of the kidney or ureter. ETIOLOGY 1) Less water intake 2) Excessive Salt intake. 3) Any damage to the endothelial lining of the kidney that leads to nidus formation.
15.5. NEOPLASMS OF KIDNEY (Tumors of Kidney)
It may be classified into three types: i) Adenomas tumors. ii) Carcinomas tumors. iii) Embryonal tumors. TUMORS OF URINARY TRACT (Its your assignment). END OF URINARY SYSTEM
COMPOSED BY M. SAJJAD HUSSAIN DVM 4th semester (2007-ag-1638)
PRESENTED BY M. SAJJAD HUSSAIN msh.03226272278@gmail.com
You might also like
- Pathology of Liver, Biliary, and PancreasDocument52 pagesPathology of Liver, Biliary, and PancreasHassan.shehri100% (11)
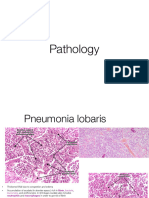
- PathologyDocument30 pagesPathologyTenorski baritonNo ratings yet
- Vascular Events in Acute InflammationDocument21 pagesVascular Events in Acute InflammationPOPCULTUREFAMNo ratings yet
- Endometrial Hyperplasia Microscopic FindingsDocument10 pagesEndometrial Hyperplasia Microscopic Findingsanditri weningtyasNo ratings yet
- Practical 4 PathologyDocument13 pagesPractical 4 PathologyVINCENTNo ratings yet
- Tubulointerstitial Disease Visual PathDocument5 pagesTubulointerstitial Disease Visual PathDavid KramerNo ratings yet
- Pathology Slides by Organ 2Document25 pagesPathology Slides by Organ 2Lin AdutNo ratings yet
- Bromadiolona en PerrosDocument9 pagesBromadiolona en Perrosantonio arteagaNo ratings yet
- Review Paper: I. Explain Briefly The Following TermDocument6 pagesReview Paper: I. Explain Briefly The Following Termapi-19916399No ratings yet
- Section 1 Functional Disturbances and Diseases of Kidneys: DR - Damodar SedaiDocument82 pagesSection 1 Functional Disturbances and Diseases of Kidneys: DR - Damodar SedaiShreeya SharmaNo ratings yet
- Pathology 1st Practical ExamDocument101 pagesPathology 1st Practical Examjeffrey_co_1No ratings yet
- Guide to the Hepatobiliary System and Liver DiseaseDocument29 pagesGuide to the Hepatobiliary System and Liver DiseaseRahulNo ratings yet
- Pathanatomy Full MCQ SDocument47 pagesPathanatomy Full MCQ SAbhishek RaoNo ratings yet
- A Complete Neurological Nursing Assessment GuideDocument57 pagesA Complete Neurological Nursing Assessment GuideSarithaRajeshNo ratings yet
- 1) The Pathophysiology of Generalised Edema in Congestive Heart FailureDocument7 pages1) The Pathophysiology of Generalised Edema in Congestive Heart FailureAishah NajihahNo ratings yet
- CH 3 Hemodynamic Disorders, Thromboembolic Disease,: A. CongestionDocument11 pagesCH 3 Hemodynamic Disorders, Thromboembolic Disease,: A. Congestion賴宥瑄No ratings yet
- Week 5 Etiology of DiseasesDocument68 pagesWeek 5 Etiology of DiseasesShaira InditaNo ratings yet
- Task Full AnsDocument16 pagesTask Full AnsManushi HenadeeraNo ratings yet
- Hematologic DysfuncyionDocument96 pagesHematologic DysfuncyionJason OgalescoNo ratings yet
- Hemodynamic DisorderDocument7 pagesHemodynamic DisorderYana MilyushinaNo ratings yet
- Microscopy exam guideDocument16 pagesMicroscopy exam guideSalsa Salaa HNo ratings yet
- Practical 4 Cardivascular and Hepatobiliary SystemDocument9 pagesPractical 4 Cardivascular and Hepatobiliary SystemchinNo ratings yet
- EclampsiaDocument7 pagesEclampsiaAbsalom MwazhaNo ratings yet
- Pathology Seminar Review (Semester 1)Document26 pagesPathology Seminar Review (Semester 1)Lin AdutNo ratings yet
- Hemodynamic Disorders, Thromboembolic Disease, And Shock NewDocument170 pagesHemodynamic Disorders, Thromboembolic Disease, And Shock Newtsegayg1999No ratings yet
- Pathology Practical HISTOPATHOLOGYDocument60 pagesPathology Practical HISTOPATHOLOGYAnkita PandaaNo ratings yet
- CHAPTER 5 InflammationDocument51 pagesCHAPTER 5 Inflammationyeshita yonasNo ratings yet
- Diseases of Urinary SystemDocument29 pagesDiseases of Urinary SystemHassan.shehri100% (9)
- 2013 Surgery ReviewDocument5 pages2013 Surgery ReviewHaslinNo ratings yet
- Development of Urinary SystemDocument20 pagesDevelopment of Urinary SystemAmanuel TagesseNo ratings yet
- Gross SpecimensDocument16 pagesGross SpecimensRavi RagavendarNo ratings yet
- Veterinary Clinics: Canine and Feline UveitisDocument24 pagesVeterinary Clinics: Canine and Feline UveitisAdrian RamirezNo ratings yet
- Liver FibrosisDocument12 pagesLiver FibrosisEslam NassarNo ratings yet
- Pathology For Dentistry Lect 10Document9 pagesPathology For Dentistry Lect 10Mohamad AladdinNo ratings yet
- PathologyDocument9 pagesPathologyGeorge MagedNo ratings yet
- Venous CongestionDocument20 pagesVenous CongestionLittle Miss CeeNo ratings yet
- Hydronephrosis OutlineDocument13 pagesHydronephrosis OutlineSarah Sy-SantosNo ratings yet
- Acute Tubular Injury PathogenesisDocument4 pagesAcute Tubular Injury PathogenesisChristopher CheweNo ratings yet
- Imaging in Ductal Plate MalformationsDocument7 pagesImaging in Ductal Plate MalformationsDiego Fernando Ortiz TenorioNo ratings yet
- Renal Pathology 2- 2021Document13 pagesRenal Pathology 2- 2021oziad4518No ratings yet
- Embryology of Urinary SystemDocument34 pagesEmbryology of Urinary SystemFatimaNo ratings yet
- Cell Injury Pathology Types Causes MechanismsDocument17 pagesCell Injury Pathology Types Causes MechanismsAli AzizNo ratings yet
- 2023 S2 Renal Practical CSB520Document6 pages2023 S2 Renal Practical CSB520Saem HashmiNo ratings yet
- HbS gene mutation causes sickle cell anemiaDocument29 pagesHbS gene mutation causes sickle cell anemiaJennyu YuNo ratings yet
- Hydatidcyst 180609173228 PDFDocument60 pagesHydatidcyst 180609173228 PDFKarem MaaliNo ratings yet
- Systemic Path Slides Final-By A Student PDFDocument60 pagesSystemic Path Slides Final-By A Student PDFpixey55No ratings yet
- Objective: Contagious Bovine PleuropneumoniaDocument2 pagesObjective: Contagious Bovine PleuropneumoniaSulove KoiralaNo ratings yet
- Peritonitis: Dr. Mahmoud Al-AwayshehDocument35 pagesPeritonitis: Dr. Mahmoud Al-Awayshehraed faisalNo ratings yet
- DB50 - Pa Tho Physiology and Pathology of ShockDocument4 pagesDB50 - Pa Tho Physiology and Pathology of ShockChelsea RoseNo ratings yet
- Master Radiology Notes Urology PDFDocument106 pagesMaster Radiology Notes Urology PDFNoor N. AlsalmanyNo ratings yet
- Post Mortem Examination Renal SystemDocument17 pagesPost Mortem Examination Renal SystemDanNo ratings yet
- Acute and Chronic CholecystitisDocument10 pagesAcute and Chronic Cholecystitisissam_1994No ratings yet
- Gambar Makros Mikros RadangDocument41 pagesGambar Makros Mikros RadangBevi Ayu Kumala WardaniNo ratings yet
- Midterm Review 2009-10 2007Document12 pagesMidterm Review 2009-10 2007TaylorNo ratings yet
- Pathology of Urinary System 2Document44 pagesPathology of Urinary System 2Liana Ika SuwandyNo ratings yet
- Print Chapter 25 The Urinary System Exam Flashcards - Easy NotecardsDocument4 pagesPrint Chapter 25 The Urinary System Exam Flashcards - Easy NotecardsChantel AceveroNo ratings yet
- Lec 1disorders of Vascular Flow and ShockDocument91 pagesLec 1disorders of Vascular Flow and ShockMohid AhmedNo ratings yet
- Plates illustrating the natural and morbid changes of the human eyeFrom EverandPlates illustrating the natural and morbid changes of the human eyeNo ratings yet
- Ultrastructure of the KidneyFrom EverandUltrastructure of the KidneyAlbert J. DaltonRating: 5 out of 5 stars5/5 (1)
- 2009 Caroli Et Al.Document19 pages2009 Caroli Et Al.rohishaakNo ratings yet
- Scope For Value Addition in MilkDocument20 pagesScope For Value Addition in Milkrohishaak60% (5)
- Milk CompositionDocument28 pagesMilk Compositionrohishaak100% (1)
- Case Discussion: Maha Research Labs: Sales Force ExpansionDocument11 pagesCase Discussion: Maha Research Labs: Sales Force ExpansionrohishaakNo ratings yet
- Tat To Policy 240615Document9 pagesTat To Policy 240615Hasan KhanNo ratings yet
- Cpscea ProtocolDocument9 pagesCpscea ProtocolrohishaakNo ratings yet
- General English 2Document16 pagesGeneral English 2rohishaakNo ratings yet
- Rajasthan Public Service CommissionDocument5 pagesRajasthan Public Service CommissionPooja MeenaNo ratings yet
- Genetic & Non-Genetic Afftg Dairy CowsDocument6 pagesGenetic & Non-Genetic Afftg Dairy CowsrohishaakNo ratings yet
- DONATEDocument1 pageDONATErohishaakNo ratings yet
- Semester 9 PDFDocument4 pagesSemester 9 PDFrohishaakNo ratings yet
- 5882new Banking Awareness Book 2013-14Document33 pages5882new Banking Awareness Book 2013-14prasant906No ratings yet
- Zoology AgainDocument32 pagesZoology AgainrohishaakNo ratings yet
- Sbi Po Descriptive Topics CapsuleDocument27 pagesSbi Po Descriptive Topics CapsuleJason GilesNo ratings yet
- Animals/110Document1 pageAnimals/110rohishaakNo ratings yet
- Unit 14 Metabolic Deficiency DiseasesDocument27 pagesUnit 14 Metabolic Deficiency DiseasesransinghNo ratings yet
- List of Circulating Currencies - Wikipedia, The Free EncyclopediaDocument11 pagesList of Circulating Currencies - Wikipedia, The Free EncyclopediagdeepthiNo ratings yet
- Ketone Bodies1Document22 pagesKetone Bodies1rohishaakNo ratings yet
- Fatty Acid Catabolism: 1. Digestion, Mobilization, and Transport of Fatty Acids Oxidation 3. Ketone BodiesDocument13 pagesFatty Acid Catabolism: 1. Digestion, Mobilization, and Transport of Fatty Acids Oxidation 3. Ketone BodiesrohishaakNo ratings yet
- 4091banking QuestionsDocument39 pages4091banking QuestionspavanaecigrowteamNo ratings yet
- BiochemistryDocument17 pagesBiochemistryrohishaakNo ratings yet
- Paper 1Document6 pagesPaper 1rohishaakNo ratings yet
- Ketosis-Causes AND Consequences: Biochemistry For Medics WWW - Namrata.coDocument39 pagesKetosis-Causes AND Consequences: Biochemistry For Medics WWW - Namrata.corohishaakNo ratings yet
- Prospectus of Egg Industry in IndiaDocument8 pagesProspectus of Egg Industry in IndiarohishaakNo ratings yet
- Paper 2Document10 pagesPaper 2rohishaakNo ratings yet
- Phy Sio AssDocument35 pagesPhy Sio AssrohishaakNo ratings yet
- Ketosis & KetoacidosisDocument23 pagesKetosis & KetoacidosisrohishaakNo ratings yet
- M.Prasad Naidu MSC Medical Biochemistry, Ph.D.Research ScholarDocument17 pagesM.Prasad Naidu MSC Medical Biochemistry, Ph.D.Research ScholarrohishaakNo ratings yet
- Les For GMAT Succes PDFDocument7 pagesLes For GMAT Succes PDFrohishaakNo ratings yet