Professional Documents
Culture Documents
2 Acute Pain Chronic Renal Failure Nursing Care Plans
2 Acute Pain Chronic Renal Failure Nursing Care Plans
Uploaded by
Pisay Shehannah Grail MedinaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2 Acute Pain Chronic Renal Failure Nursing Care Plans
2 Acute Pain Chronic Renal Failure Nursing Care Plans
Uploaded by
Pisay Shehannah Grail MedinaCopyright:
Available Formats
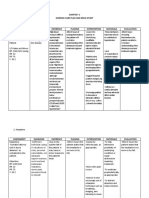
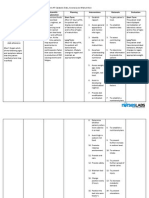
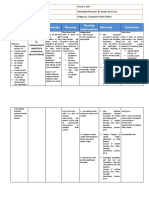
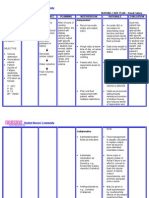
Medical Diagnosis: Chronic Renal Failure Problem: Acute Pain Assessment Subjective: (none) Objective: Facial Grimaces Guarding
ng behaviors Costovertebral pain/ Flank pain Limited ROM Body weakness Facial Mask Narrowed Focus Sleep Disturbance Diaphoresis RR & BP changes (Dont forget which of the following signs and symptoms above that the patient manifested and may manifest) Nursing Diagnosis Acute Pain Scientific Explanation Pain is a discomfort that is caused by the stimulation of the nerve endings. Any trauma that the kidney experience (by any caused or factors) perceive by the body as a threat, the body releases cytokine and prostaglandin causing pain which is felt by the patient at his/her costovertebral area/flank. Planning Short Term: After 6-8 hours of nursing interventions, the patient will demonstrate use of relaxation skills to relieve pain. Interventions 1. Establish rapport. Rationale 1. To get the cooperation of the patient and SO. Evaluation Short Term: The patient shall have demonstrated use of relaxation skills to relieve pain. (Use pain scale here)
2. Monitor and record vital signs. 3. Assess pts general condition
2. To obtain baseline data. Long Term: The patient shall have reported pain relief or control.
Long Term: After 2-3 days of nursing interventions, the patient will report relief/control of pain.
4. Accept patients description of pain.
3. To obtain baseline data
4. Pain is a subjective experience and cannot be felt by other. 5. Perform a comprehensive assessment of pain ( location , onset, characteristics, frequency) 5. To be able to compare changes from previous reports to rule out worsening of underlying condition/develo ping complications
6. Determine
6. To know
possible pathophysiology and causes of pain
underlying condition that leads to pain and possible management that would not further aggravate pain.
7. Assess patients perception along with behavioral and physiological responses.
7. To know clients attitude towards pain and use of specific pain and medication.
8. Perform pain assessment each time pan occurs, note and investigate changes from previous report. 9. Assess patients description of pain.
8. To rule out worsening of underlying condition / development of complication.
9. To acknowledge the pain experience convey acceptance of clients response to pain.
10. Observe nonverbal cues including how client walks, holds
10. Observation may/ may not be congruent with
body, sits, facial expressions, cool fingertips/ toes, which can mean constricted vessels
verbal reports indicating need for further evaluation.
11. Assess for referral pain as appropriate
11. To help determine possibility of underlying condition or organ dysfunction requiring treatment. 12. To rule out worsening of pain due to methods used.
12. Review patients previous experiences with pain and methods found either helpful or unhelpful for pain control in the past.
13. Explore method for alleviation/ control of pain.
14. Encourage verbalization of feelings about the pain.
13. Timely intervention is more likely to be successful in alleviating pain. 14. To allow out let for emotions and enhance coping mechanism.
15. Provide quite environment, calm activities and adequate rest reinforce 16. Provide comfort measures such as back rub, change position, use of heat/ cold. 17. Instruct/encourage use of relaxation exercise such as focused breathing. 18. Encourage diversional activities such as TV and socialization with others.
15. To prevent fatigue and lessen stimuli.
16. To provide nonpharmacologic pain management.
17. This is a form of relaxation technique that helps decrease level of pain.
19. Assist with selfcare activities.
18. Provides divertionary activities that help block the perception of pain by the brain.
20. Assist in treatment of underlying disease process causing pain. 21. Provide for individualized
19. To able to perform ADLs and maintain good hygiene.
physical therapy/ exercise program that can be continued by the client discharge refer to physical therapist.
22. Administer analgesics as ordered.
20. Evaluate effectiveness of therapies. 21. To continue therapeutic effect and wellness for the patient 22. Pharmacologic mgmt for pain
You might also like
- Injection Site Cheat Sheet PDFDocument2 pagesInjection Site Cheat Sheet PDFjustin_sane100% (2)
- Nursing Care PlansDocument7 pagesNursing Care PlansNicholaiCabadduNo ratings yet
- NCP - DM - FatigueDocument12 pagesNCP - DM - FatigueJisel-Apple BulanNo ratings yet
- Nursing Care Plan CYSTITISDocument2 pagesNursing Care Plan CYSTITIS@ngelo0% (1)
- NCP Chronic PainDocument4 pagesNCP Chronic Painkentkrizia100% (3)
- NCP For Dizziness and HeadacheDocument4 pagesNCP For Dizziness and Headachekarthi karthi100% (1)
- NCP - Acute PainDocument3 pagesNCP - Acute PainRene John Francisco0% (1)
- NCP SviDocument4 pagesNCP SviEjie Boy IsagaNo ratings yet
- HemodialysisDocument2 pagesHemodialysisjustin_saneNo ratings yet
- 2 Acute Pain Chronic Renal Failure Nursing Care PlansDocument5 pages2 Acute Pain Chronic Renal Failure Nursing Care Plansjustin_saneNo ratings yet
- NCP (Icu)Document2 pagesNCP (Icu)jessie_nuñez_263% (8)
- NCP 1Document5 pagesNCP 1Denisse Shazz Mae MaretNo ratings yet
- Nursing Care Plan: Lopez, Maria Sofia B. 9/29/2020 3-BSN-B Prof. ZoletaDocument5 pagesNursing Care Plan: Lopez, Maria Sofia B. 9/29/2020 3-BSN-B Prof. ZoletaSofiaLopezNo ratings yet
- Coronary Artery Disease Care PlanDocument2 pagesCoronary Artery Disease Care PlanDanelle Harrison, RN100% (2)
- Patient 3 NSDDocument20 pagesPatient 3 NSDBea Bianca CruzNo ratings yet
- Common Drug Stems Cheat SheetDocument2 pagesCommon Drug Stems Cheat SheetCharis Mae DimaculanganNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument5 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationArian May MarcosNo ratings yet
- IV GaugesDocument1 pageIV Gaugesjustin_saneNo ratings yet
- Acute Pain AGEDocument2 pagesAcute Pain AGEHarris AustriaNo ratings yet
- 5 Altered Nutrition Less Than Body Requirements Chronic Renal Failure Nursing Care PlansDocument3 pages5 Altered Nutrition Less Than Body Requirements Chronic Renal Failure Nursing Care Plansjustin_sane40% (5)
- NCPDocument2 pagesNCPDidith AbanNo ratings yet
- Hyperthermia Pneumonia Nursing Care PlanDocument1 pageHyperthermia Pneumonia Nursing Care Planjustin_saneNo ratings yet
- Physical AssessmentDocument29 pagesPhysical Assessmentjustin_saneNo ratings yet
- NCPDocument4 pagesNCPEsther RefuncionNo ratings yet
- PneumoniaDocument17 pagesPneumoniajustin_saneNo ratings yet
- Risk For Infection Pneumonia Nursing Care PlanDocument1 pageRisk For Infection Pneumonia Nursing Care Planjustin_sane100% (1)
- Risk For Infection Pneumonia Nursing Care PlanDocument1 pageRisk For Infection Pneumonia Nursing Care Planjustin_sane100% (1)
- NCP FormatDocument2 pagesNCP FormatNaotaka KohinataNo ratings yet
- Nursing Care Plan #1Document6 pagesNursing Care Plan #1Yamete KudasaiNo ratings yet
- Assessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveDocument2 pagesAssessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveDanica Kate GalleonNo ratings yet
- Acute Pain Related To InjuryDocument2 pagesAcute Pain Related To InjuryErickson Caisido GarciaNo ratings yet
- Pleural EffusionDocument5 pagesPleural EffusionTerizla MobileNo ratings yet
- NCPDocument3 pagesNCPDharline Abbygale Garvida Agullana100% (2)
- EdemaDocument2 pagesEdemaVirus50% (2)
- Ineffective Airway Clearance Pneumonia Nursing Care PlanDocument1 pageIneffective Airway Clearance Pneumonia Nursing Care Planjustin_sane100% (4)
- Activity IntoleranceDocument2 pagesActivity IntoleranceJenny Pearl PasalNo ratings yet
- Nursing Care Plan - NumbnessDocument2 pagesNursing Care Plan - NumbnessJasmin Jacob100% (3)
- 2 NCP Impaired Swallowing EditedDocument4 pages2 NCP Impaired Swallowing EditedZharm MayNo ratings yet
- NCP AfDocument3 pagesNCP AfAngelica Mercado SirotNo ratings yet
- Ineffective Airway Clearance Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: IndependentDocument4 pagesIneffective Airway Clearance Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: IndependentIrish Eunice FelixNo ratings yet
- Nursing Diagnosis For Pediatrics Gastroenteritis 1Document2 pagesNursing Diagnosis For Pediatrics Gastroenteritis 1densu4u100% (4)
- NCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus NephropathyDocument4 pagesNCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus NephropathySapna thakurNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanJoshua Pascasio100% (1)
- Nursing Care Plan Renal FailureDocument2 pagesNursing Care Plan Renal FailureMark Jason Rabadan100% (1)
- NCP For CTTDocument2 pagesNCP For CTTKay D. BeredoNo ratings yet
- NCP - Acute Pain Related To EdemaDocument2 pagesNCP - Acute Pain Related To EdemaChenime Añana0% (1)
- Cad NCPDocument1 pageCad NCPKrizzia Mae F. MayoresNo ratings yet
- NCPDocument4 pagesNCPAnn AquinoNo ratings yet
- Nursing Care PlanDocument1 pageNursing Care PlanMichael John PaderesNo ratings yet
- NCPDocument1 pageNCPJ. ishtelleNo ratings yet
- BPN NCPDocument6 pagesBPN NCPJoart EspinozaNo ratings yet
- Nursing Care Plan: References: Nurse's Pocket Guide Pages 151-155Document1 pageNursing Care Plan: References: Nurse's Pocket Guide Pages 151-155Caroline ChaNo ratings yet
- NCP: Acute GastroenteritisDocument3 pagesNCP: Acute GastroenteritishauteanicoleNo ratings yet
- Disturbed Sleep PatternDocument2 pagesDisturbed Sleep PatternROxanne S. RendonNo ratings yet
- Uti NCPDocument1 pageUti NCPAngelique Vinoya100% (2)
- Nursing Health History of ReyDocument3 pagesNursing Health History of ReyElaine Joy Calma Canlas100% (1)
- NURSING CARE PLAN (Vomiting) Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Goal: IndependentDocument2 pagesNURSING CARE PLAN (Vomiting) Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Goal: IndependentRohanie100% (1)
- Acute Pain OsteosarcomaDocument8 pagesAcute Pain OsteosarcomaMaryjoy Gabriellee De La Cruz100% (1)
- Health Teaching Plan DyspneaDocument3 pagesHealth Teaching Plan DyspneaMae JavierNo ratings yet
- Nursing Care Plan ADocument6 pagesNursing Care Plan ACrystal WyattNo ratings yet
- Nursing Care Plan Peptic UlcerDocument3 pagesNursing Care Plan Peptic UlcerJefferson Baluyot PalmaNo ratings yet
- NCP - Excessive Fluid VolumeDocument4 pagesNCP - Excessive Fluid VolumeryanNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanRaphael Reyes Enriquez100% (1)
- NCP Fluid Vol Excess AgnDocument3 pagesNCP Fluid Vol Excess AgnArbie JacintoNo ratings yet
- Nursing Care Plan: Pulmonary EbolismDocument5 pagesNursing Care Plan: Pulmonary EbolismneuronurseNo ratings yet
- Nursing Care Plan Rheumatoid ArthritisDocument3 pagesNursing Care Plan Rheumatoid ArthritisJashAnia MarIe EvArdo FloresNo ratings yet
- NCP DMDocument6 pagesNCP DMstara123No ratings yet
- Post-Thyroidectomy FdarDocument1 pagePost-Thyroidectomy FdarKim Glaidyl BontuyanNo ratings yet
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationDocument1 pageNovilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationCharina AubreyNo ratings yet
- Grieve and LossDocument6 pagesGrieve and LossRuffy AbdulazisNo ratings yet
- Acute Pain Nursing Diagnosis & Care Plans - NurseTogetherDocument22 pagesAcute Pain Nursing Diagnosis & Care Plans - NurseTogetherrachealakusukNo ratings yet
- NCPDocument18 pagesNCPChristian Karl B. LlanesNo ratings yet
- DiagnosticDocument5 pagesDiagnosticjustin_saneNo ratings yet
- Improving Postoperative Pain Management What Are.40Document6 pagesImproving Postoperative Pain Management What Are.40Luz Adriana Flores PalafoxNo ratings yet
- Peptic UlcerrDocument3 pagesPeptic Ulcerrjustin_saneNo ratings yet
- Applications of Telecounselling in Spinal Cord Injury Rehabilitation: A Systematic Review With Effect SizesDocument13 pagesApplications of Telecounselling in Spinal Cord Injury Rehabilitation: A Systematic Review With Effect Sizesjustin_saneNo ratings yet
- DMDocument10 pagesDMjustin_saneNo ratings yet
- Assessment Nursing Diagnosis Scientific Explanation Planning Interventions Rationale EvaluationDocument2 pagesAssessment Nursing Diagnosis Scientific Explanation Planning Interventions Rationale Evaluationjustin_saneNo ratings yet
- Microsoft Word - Pneumonia Education EnglishDocument9 pagesMicrosoft Word - Pneumonia Education Englishjustin_saneNo ratings yet
- Other Possible Nursing Care PlansDocument1 pageOther Possible Nursing Care Plansjustin_saneNo ratings yet
- Ineffective Breathing Pattern Pneumonia Nursing Care PlanDocument1 pageIneffective Breathing Pattern Pneumonia Nursing Care Planjustin_saneNo ratings yet
- Impaired Gas Exchange Pneumonia Nursing Care PlanDocument1 pageImpaired Gas Exchange Pneumonia Nursing Care Planjustin_saneNo ratings yet
- Chilldeck KTV & Music Lounge: Free Five (5) Songs in Every Three (3) Buckets of DrinksDocument1 pageChilldeck KTV & Music Lounge: Free Five (5) Songs in Every Three (3) Buckets of Drinksjustin_saneNo ratings yet