Professional Documents
Culture Documents
June Case Study Final
June Case Study Final
Uploaded by
api-174496267Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
June Case Study Final
June Case Study Final
Uploaded by
api-174496267Copyright:
Available Formats
1 Amanuel Negussie DOS 731 - June Case Study July 2013 Volumetric Modulated Arc therapy (VMAT) treatment
of Tonsillar Cancer History of Present Illness: KC is a 61-year-old gentleman with a history of stage IVA follicular lymphoma diagnosed in July 2012. A positron emission tomography/computed tomography (PET/CT) performed in July 18, 2012 demonstrated involvement in the superficial lobe of right parotid gland, lymph node in the tail of right parotid, intraparotid lymph nodes within the tail of the left parotid, and left laryngeal tonsil. In addition, abdomen and pelvis showed extensive hypermetabolically active adenopathy within retroperitoneum, peripancreatic area, along the mesentery and within the pelvis. Musculoskeletal also showed low uptake with findings concerning for skeletal involvement. A bone biopsy performed showed hypercellular bone marrow with trace involvement by non-hodgkins in the right side only. As a result, the patient received chemotherapy with Rituminab, Cyclophosphamide, Bendamustine, Rituxan, Vincristine, and Prednisone. A restaging PET/CT scan performed on February 2013 showed favorable treatment response. However, persistent abnormal activity in the left palatine tonsil was noted. In addition, a new cervical lymphadenopathy was located in the left neck, level IIA and 3, measuring up to 1.5 centimeter (cm). In March 2013, KC underwent a left tonsil biopsy which showed human papillomavirus (HPV) positive moderately differentiated keratinizing squamous cell carcinoma. The tumor was staged IVA (T1N2b). As a primary treatment, the patient underwent tonsillectomy and neck dissection in April 2013. Past Medical History: KC has a past medical history of non-Hodgkins lymphoma, arthritis, high blood pressure, chickenpox, and a hernia repair. In addition, he has some hearing loss and tinnitus. He also has chronic problem with painful stiff joints. KC is allergic to penicillin. Social History: KC is an employee at mental health institution. He does not smoke tobacco, and does not drink alcoholic beverages. KCs mother had multiple myeloma at age 93. He has no other family history of cancer. Medication: KC is currently taking Aleve, Citalopram, and Xanax. Diagnostic Imaging Studies: The patient had a diagnostic PET/CT scan in July 2012. The study showed a tonsillar mass with the right parotid gland and intra parotid lymph nodes involvement.
2 A post-chemotherapy PET/CT scan was also performed in February 2013 that demonstrated a positive treatment response. It also showed a cervical lymphadenopathy in the left neck that measured 1.5 cm. Radiation Oncologist Recommendations: KC was recommended to undergo surgery followed by radiation therapy to treat his tonsillar tumor along with involved regional lymph nodes. The patient agreed to undergo both procedures. The post-operative radiation therapy was planned to be tailored according to the surgical findings. Potential benefits and risks associated with post-op radiation therapy for tonsillar cancer were reviewed in detail with the patient. He had numerous questions all of which were answered to his satisfaction. The Plan (Prescription): After reviewing the surgical findings and examining the patient, the radiation oncologist decided to proceed with VMAT treatment. The treatment was prescribed to the left tonsillar and bilateral necks to 5000 centigray (cGy) at 200 cGy per fraction followed by a boost to the tumor bed and involved nodes to 1400 cGy at 200 cGy per fraction, and a second boost to the tumor bed to 600 cGy at 200 cGy per fraction. Patient Setup/Immobilization: KC was simulated in a supine position with his head towards the scanner. A wire was placed on his surgical scar. His head was set in a slightly extended position on an accufoam. A bite block was used to keep his mouth open during treatment (Figure 1). A shoulder strap was used to pull the shoulders away from the treatment area (Figure 1). An aquaplast mask was made by warming a thermoplastic mesh in a warm bath and stretching it over the patients face, neck, and shoulders (Figure 1). The customized mask will be used to reproduce the same head position and restrict movement during treatment. A sponge was placed under his knees for comfort. A General Electric (GE) Lightspeed 4 slice CT unit was used for the simulation. The head and neck images were taken at 2.5 mm slices. Due to weight loss, KC was re-simulated for his boost treatment. Similar setup position was used. A new aquaplast mask was made since the original one was not fitting appropriately. Anatomic Contouring: After the simulation was completed, the CT scan slices were imported into Varian Eclipse version 10 treatment planning system (TPS). The medical dosimetrist contoured all the normal structures including the brain, brain stem, left and right eye, left and right lens, total lung, left and right inner ear, left and right optic nerve, left and right parotid, mandible, and oral cavity. The radiation oncologist contoured the optic chiasm, pituitary gland,
3 submandibular gland, thyroid, gross tumor volume (GTV), clinical target volume (CTV), and planning target volume (PTV). Beam Isocenter/ Arrangement: A Varian 21 IX linear accelerator (Linac) was used to treat the patient. During simulation, the radiation oncologist set an isocenter within the treatment site. For the initial PTV 50, three rotational arcs were arranged, two in clockwise (CC) direction and one in counter clockwise (CCW) direction. The first CC beam rotated from 205o to 155o with 5o collimator angle and 15 x 21 cm field size (Figure 2). The second CC beam rotated from 155o to 205o with 355o collimator angle and 15 x 21 cm field size (Figure 3). The CCW beam rotated from 205o to 155o with 270o collimator angle and 15 x 120 cm field size (Figure 4). The couch rotation was set at 0o for all arcs. For PTV 64, two rotational arcs were arranged, one in CC direction and one in CCW direction. The CC beam rotated from 210o to 179o with 10o collimator angle and 11.6 x 12.3 cm field size. (Figure 5). The CCW beam rotated from 179o to 210o with 350o collimator angle and 11.6 x 12.3 cm field size (Figure 6). For PTV 70, two rotational arcs were arranged, one in CC direction and one in CCW direction. The CC beam rotated from 210o to 150o with 20o collimator angle and 5.7 x 5.4 cm field size (Figure 7). The CCW beam rotated form 150o to 210o with 340o collimator angle and 5.7 x 5.4 cm field size (Figure 8). Treatment Planning: The medical dosimetrist started the plan by choosing the appropriate gantry rotation, collimator angle, and field size that allowed best target coverage. The spinal cord was expanded by 3 mm in all angles. Avoidance structures were created for structures that overlap with the target with 2 mm margin around the PTV. This included left parotid, right parotid, mandible, and oral cavity. A 1 cm thick ring was created 2 cm away from the PTV (Figure 9). The purpose of the ring was reduce beam streaking and increase dose conformity. The dental artifact was contoured and assigned a density of water. Metal artifacts can distort dose distribution by creating cold and hot spots.1 Therefore, this correction method reduces such complication. The initial plan had two arc fields, one rotating from 155o to 205o and the other from 205o to 155o (Figure 2 and 3). The inverse planning process included clinical goals to the PTV 50 and planning constraints to the ring, the avoidance structures, and OR. The progressive resolution optimizer (PRO) algorithm within the eclipse software generated an ideal intensity map with
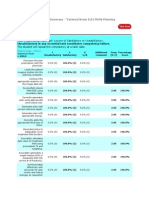
4 optimal weighting of each control point. The MLC segments, the gantry speeds, and the dose rates of each control point were generated from the ideal intensity map. The plan was reviewed after each optimization and weightings of the objectives were adjusted based on the information retrieved from the dose volume histogram (DVH) and the isodose lines. During this process, the medical dosimetrist noted that the spinal cord was not meeting the required constraints. Multiple attempts were made to minimize the dose, but it was affecting the PTV coverage. As a result, the medical dosimetrist decided to add a third arc field, which covered mostly the superior portion of the PTV and cut off of the spinal cord that was in the treatment field. This helped reduce the dose to spinal cord with an adequate PTV coverage. The final three dimension (3D) dose distribution was evaluated using DVH analysis as well as viewing the 3D dose distribution in multi-plane view and on individual CT slices. The final dose calculation was performed using the analytical anisotropic algorithm (AAA). The plan was finalized with the 95% isodose line covering PTV 50 with a mean dose of 5120 cGy and a maximum dose of 5510 cGy located within PTV 50 (Figure 10 and 11). All of the clinical goals and planning objectives were met (Figure 12). After careful revision, the physician accepted the initial plan. The boosts were optimized with the same objectives used to plan the initial treatment. The inverse planning process included clinical goals to the PTV 64 and PTV 70, and planning constraints to the ring, the avoidance structures, and OR. The plan was reviewed after each optimization and weightings of the objectives were adjusted based on the information retrieved from the dose volume histogram (DVH) and the isodose lines. The PTV 64 plan was finalized with the 95% isodose line covering PTV 60 with a mean dose of 6569 cGy and a maximum dose of 6995 cGy located within PTV 60 (Figure 13 and 14). The PTV 70 plan was finalized with the 95% isodose line covering PTV 70 with a mean dose of 7126 cGy and a maximum dose of 7483 cGy located within PTV 70 (Figure 13 and 14). All of the clinical goals and planning objectives were met (Figure 14). After careful revision, the physician accepted the boost plans. Quality Assurance / Physics Check: A monitor unit check was performed with RadCalc. At the clinical site, a 5% deviation in MU is the tolerance for all plans. Anything outside of this range needs to be recalculated and fixed by the medical dosimetrists or physicists prior to the first treatment. The initial and boost plans were approved with an individual MU difference less than 2% (Figure 15, 16, and 17).
5 The rapid arc QAs were generated using the AAA of each arc. The intensity maps were calculated in a solid water flat phantom. The intensity maps were exported to be compared to measurements obtained with the SunNuclear MapCheck device. The PTV 50 plan passed the QA with 3%, the PTV 64 plan with 2.8%, and the PTV 70 plan with 3% differentiation. Conclusion: This plan presented the medical dosimetrist with few challenges. A great deal of time was spent creating avoidance and optimizing structures. This eased the planning process, as it allowed the medical dosimetrist to simply manipulate the PTV coverage and the dose to ORs. One of the challenges that the medical dosimetrist faced was minimizing the dose to the spinal cord. This is expected in most head and neck treatments since a large portion of the cervical spine can lie in the path of the entrance and exit treatment beam. To avoid such difficulties, the spinal cord in this plan was initially expanded by 3 mm for optimization purpose. In addition, the beam was set to not directly rotate along the patients posterior neck and minimize the dose to the spinal cord. Although these cautions were taken, the spinal cord still presented a challenge to the plan. As stated above, adding a third arc beam was found necessary to meet the goal.
6 Figures
Figure 1. The patients setup position with accufoam, aquaplast mask, bite block, and shoulder strap
Figure 2. Transverse, coronal, and sagittal view of the PTV. Blue represents PTV50, pink represents PTV 64, red represents PTV70
Figure 2. Collimator angle and field size of the first arc covering PTV50
Figure 3. Collimator angle and field size of the second arc covering PTV 50
Figure 4. Collimator angle and field size of the third covering PTV 50
Figure 5. Collimator angle and field size of the third covering PTV 64
Figure 6. Collimator angle and field size of the third covering PTV 64
10
Figure 7. Collimator angle and field size of the third covering PTV 70
Figure 8. Collimator angle and field size of the third covering PTV 70
11
Figure 9. Transverse, coronal, and sagittal view of the 2 cm ring constructed around the PTV
12
Figure 10. Transverse, coronal, and sagittal view of dose distribution. The 95% isodose line (blue) conformity around the PTV (pink)
13
Figure 11. A Dose-wash representation of the 95% dose distribution across PTV 50
PTV 50 Oral Cavity Mandible
Rt Parotid Rt Inner Ear Lt Parotid
Spinal cord
Figure 12. DVH of the initial VMAT plan
14
Figure 13. A Dose-wash representation of the 95% dose distribution to PTV 64 and PTV 70
PTV 64
PTV 70
Rt. Parotid
Spinal cord
Figure 14. DVH of the boost VMAT plans
15
Figure 15. MU check of the PTV 50 plan
16
Figure 16. MU check of the PTV 64 plan
Figure 17. MU check of the PTV 70 plan
17 References 1. Kim Y, Tome WA, Todd MB, et al. The impact of metal artifacts on head and neck IMRT dose distribution. Radiotherapy and Oncology. 2006;79(2):198-202.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- DatabaseDocument161 pagesDatabaseFahidNo ratings yet
- Petty Cash Exercises ANSWERSDocument2 pagesPetty Cash Exercises ANSWERSXDragunov Alcroix100% (10)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Professional Responsibility OutlineDocument48 pagesProfessional Responsibility OutlineEli Colmenero100% (5)
- Moving RIG Mobilization & Risk Assessment: Harmand - Cv. Marga Sari UtamaDocument28 pagesMoving RIG Mobilization & Risk Assessment: Harmand - Cv. Marga Sari UtamaHSE PT. GROGOL SARANA TRANSJAYANo ratings yet
- Excel103 AdvancedExercisesDocument33 pagesExcel103 AdvancedExercisesArun ThevarNo ratings yet
- The Components of Clinic Management System AreDocument5 pagesThe Components of Clinic Management System AreCedric PurgatorioNo ratings yet
- Chapter 4 OjtDocument9 pagesChapter 4 OjtKatz EscañoNo ratings yet
- Tank SterilizationDocument6 pagesTank SterilizationalshamlehNo ratings yet
- 02-Samss-013 2020Document16 pages02-Samss-013 2020slan79bisNo ratings yet
- Oryx ASHRAE - Salah Nezar 24-09-2010 TransmitedDocument46 pagesOryx ASHRAE - Salah Nezar 24-09-2010 Transmitednavas1972No ratings yet
- Internship ReportCAA PakistanDocument9 pagesInternship ReportCAA PakistanUmairChJalandhariNo ratings yet
- Comparative Study of Education in Kenya and Japan: What Can Kenya Learn?Document25 pagesComparative Study of Education in Kenya and Japan: What Can Kenya Learn?dulluamos78% (27)
- Amanuel Negussie: Certificate of AttendanceDocument1 pageAmanuel Negussie: Certificate of Attendanceapi-174496267No ratings yet
- ElectronDocument2 pagesElectronapi-174496267No ratings yet
- V 13 RtsummaryonsitetrainingworkshopfamanuelnegussieDocument1 pageV 13 Rtsummaryonsitetrainingworkshopfamanuelnegussieapi-174496267No ratings yet
- ImrtDocument3 pagesImrtapi-174496267No ratings yet
- Conference LogsDocument1 pageConference Logsapi-174496267No ratings yet
- WK VII WikiDocument6 pagesWK VII Wikiapi-174496267No ratings yet
- For E-PortfolioDocument14 pagesFor E-Portfolioapi-174496267No ratings yet
- WK VI WikiDocument4 pagesWK VI Wikiapi-174496267No ratings yet
- WK II WikiDocument4 pagesWK II Wikiapi-174496267No ratings yet
- Esophagus and ProstateDocument3 pagesEsophagus and Prostateapi-174496267No ratings yet
- PDF Chapter 5 The Expenditure Cycle Part I Summary - CompressDocument5 pagesPDF Chapter 5 The Expenditure Cycle Part I Summary - CompressCassiopeia Cashmere GodheidNo ratings yet
- Oma MMS Enc V1 - 2 20050301 ADocument116 pagesOma MMS Enc V1 - 2 20050301 AcolonmeNo ratings yet
- CMHC Annual Report 2022 enDocument177 pagesCMHC Annual Report 2022 enHelena MarlynNo ratings yet
- Piezon Master EAS PM700 Service ManualDocument28 pagesPiezon Master EAS PM700 Service ManualcckmNo ratings yet
- 7.4 - Equations and Graphs of Trigonometric FunctionsDocument16 pages7.4 - Equations and Graphs of Trigonometric FunctionsJoven IsNo ratings yet
- Tips For Writing Better Answers in Upsc Main ExamiDocument30 pagesTips For Writing Better Answers in Upsc Main ExamivikramadhityaNo ratings yet
- Chapter 1 Lesson 1Document10 pagesChapter 1 Lesson 1NathanNo ratings yet
- UNIT Portfolios 1-5 - Spanish 1 3Document2 pagesUNIT Portfolios 1-5 - Spanish 1 3s9321722No ratings yet
- Penalty and ProsecutionsDocument50 pagesPenalty and ProsecutionsSatish BhadaniNo ratings yet
- The Chhattisgarh Land Revenue Code 1959 Complete Act - Citation 134590 - Bare AcDocument175 pagesThe Chhattisgarh Land Revenue Code 1959 Complete Act - Citation 134590 - Bare AcKshitij NawarangNo ratings yet
- GSK218M Programming Operation ManualDocument327 pagesGSK218M Programming Operation ManualMiguel DiazNo ratings yet
- ECE EEE F418 Term Project Presentation ScheduleDocument7 pagesECE EEE F418 Term Project Presentation SchedulesaimanobhiramNo ratings yet
- 4.2.4. Manual-BIS Hotel5.7 Manual Instruction PDFDocument92 pages4.2.4. Manual-BIS Hotel5.7 Manual Instruction PDFIgoFernandesNo ratings yet
- Checklist FormDocument2 pagesChecklist FormMarinelle Abulencia RoblesNo ratings yet
- Preliminary Footing Design Template: Jsdesign EngineeringDocument2 pagesPreliminary Footing Design Template: Jsdesign EngineeringJohnnyNo ratings yet
- ENTP. Per TOPICDocument13 pagesENTP. Per TOPICeffendyNo ratings yet
- EXP13 PNP Transistor As An AmplifierDocument3 pagesEXP13 PNP Transistor As An AmplifierMohammed Dyhia AliNo ratings yet
- Saudi Aramco Test Report: External Tank Bottom Testing 24-Jul-18 CP-SATR-X-3204Document7 pagesSaudi Aramco Test Report: External Tank Bottom Testing 24-Jul-18 CP-SATR-X-3204nadeem shaikhNo ratings yet