Professional Documents
Culture Documents
Assessment of A Clinical Trial
Uploaded by
api-240690004Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Assessment of A Clinical Trial
Uploaded by
api-240690004Copyright:
Available Formats
Ashley Francis Please read the article by Bolliger et al. and answer the following questions.
Assessment of a Clinical Trial
1 Adequate literature review? I do not think this article serves as an adequate literature review. Few previous findings were discussed and even fewer directly applicable to the goals of this study. The authors did mention that little research has been done on the subject matter. The goal of this study was to determine whether the use of oral nicotine inhalers can result in long term reduction in smoking; and the safety nicotine replacement and smoking. Pharmacia and Upjohn Consumer Healthcare of Sweden. (A pharmaceutical development company). -Receive information about general implications of smoking. -Asked to reduce the number of cigarettes daily as much as possible (50% reduction suggested). -Nicorette Inhaler used for nicotine replacement (maufactured by Pharmica and Upjohn); disposable cartridges containing 10 mg nicotine and 1 mg methanol that dispense approximately 4-5 mg of nicotine at room temperature. -Participants instructed to use between 6 to 12 cartridges over 24 hours (24 - 60 mg of nicotine in 24 hours). -Participants were encouraged to decrease use of inhaler after 4 months, but could continue up to 18 out of 24 months. -Counseling also provided at each visit to the clinic for assessment (at 1, 2, 3, and 6 weeks; and 3, 4, 6, 12, 18, 24 months) -Receive information about general implications of smoking. -Asked to reduce the number of cigarettes daily as much as possible (50% reduction suggested). -Methanol used in inhaler cartridge in replacement of nicotine. -Participants instructed to use between 6 to 12 cartridges over 24 hours. -Participants were encouraged to decrease use of inhaler after 4 months, but could continue up to 18 out of 24 months. -Counseling also provided at each visit to the clinic for assessment (at 1, 2, 3, and 6 weeks; and 3, 4, 6, 12, 18, 24 months) 200 200 Randomized by computer generation Double blinded test -At least 18 years old -Smoke 15 or more cigarettes a day -Have a carbon monoxide concentration in exhaled are greater than or equal to 10 ppm -Have smoked regularly for three or more years -Have failed at least one serious attempt to quite within the past 12 months -Want to reduce smoking as much as possible with the help of the nicotine inhaler -Be prepared to adhere to protocol -Be willing to provide informed consent
Goal of the study
Source of funding
Test drug regimen
Control drug regimen
6 7 8 9
Number of subjects: test drug Number of subjects: control drug Randomized? If so, what method of randomization was used? Blindingnone, single-blinded, doubleblinded
Inclusion criteria 10
Exclusion criteria 11
-Current use of nicotine replacement therapy or any other behavioral or pharmacological smoking cessation or reduction program -Use of other nicotine containing products -Any other condition that might interfere with the study Yes, but there were 18 more women in the active treatment group. @ 4 months: (84/200) x 100 = 42% @ 12 months: (27/200) x 100 = 13.5% @ 18 months: (22/200) x 100 = 11% n=166 for those that were compliant and completed 24 month test. @ 4 months: (62/200) x 100 = 31% @ 12 months: (12/200) x 100 = 6% @ 18 months: (8/200) x 100 = 4% n=144 for those that were compliant and completed 24 month test. -Throat irritation and coughing more common in active group. -227 adverse events reported in treatment group by 113 participants. -Throat irritation and coughing more common in active group. -Nausea, vomiting, and palpitation also reported. (9 with nausea symptoms, 1 with palpitation). -193 adverse events reported in placebo group by 114 participants. -Nausea, nausea and vomiting, palpitation also reported. (8 with nausea symptoms, 2 with palpitation) -Nicotine inhalers effectively and safely achieved sustained reduction in smoking over 24 months.
12
Were groups generally comparable at baseline? (note any exceptions)
13
Test drug compliance
14
Control drug compliance
15
Major toxicity of test drug
16
Major toxicity of control drug
17
Major finding of the study
18
There is a 1.2% chance that these findings are due to chance at 24 What is the probability that the findings in months. (0.1% and 0.2% at months 4 and 12 respectively). this study are due to chance? Aside from the experimental treatment, were the groups treated equally? If not, The groups were treated equally. how did they differ? Patients were analyzed by intention-to-treat analysis. Were patients analyzed by intention-totreat or per-protocol? Using an intention-to-treat analysis, what is the success in sustained smoking Treatment Group = (26/200) x 100 = 13% reduction at 12 months for the treatment Placebo Group = (8/200) x 100 = 4% group & for the placebo group? Using a per protocol analysis, what is the success in sustained smoking reduction at Treatment Group = (26/27) x 100 = 96.3% 12 months for the treatment group & for Placebo Group = (8/12) x 100 = 66.7% the placebo group? Yes, the study indicated who was lost to follow up and why. However, Were all patients who entered the trial they did not make a comparison to those not lost to follow up. accounted for at its conclusion? The authors did NOT directly indicate any sources of bias. They did discuss limitations. However, there is bias present. There is selection bias based on the potential difference in all smokers and those responding to the add in the newspaper. There was bias due to drop Did authors state potential sources of outs and non-compliance, however, intention-to-treat minimizes. There bias? What are the sources of bias in the may also be bias present as a result of a conflict of interest. Those study? conducting the study are paid by those funding the study and producing the products used by the study. There may be recall bias present as subjects are self reporting the reduction of cigarettes smoked.
19 20
21
22
23
24
25
26
-While the data supports the authors conclusions, there are discrepancies and inconsistencies in reported data. Compliance numbers do not add up within different tables and the article itself. Also, Do the data presented in the study support the authors fail to address small sample size (Fishers Exact testing) and the authors conclusions? power level when making claims. Therefore, even though the data supports the conclusions, the data seems incomplete and misleading. -Data regarding safety conclusion is vague and does not support claims. This study may be likely to affect clinical practice as it indicates statistical findings. It is more likely to be published and pharmaceutical Is this study likely to affect clinical representatives from Pharmacia and Upjohn will be more apt to present practice? Why/why not? these findings when marketing their product.
1. Briefly discuss the strengths of the article 2. Briefly discuss the limitations of the study. 3. Briefly discuss the public health implication of the study if any (Note: Your response to these three questions should not be more than two double space pages) (See attached)
Bolliger et al. assessed smoking reduction with oral nicotine inhalers in a double-blinded, randomized clinical trial of efficacy and safety. The goal of the study was to determine if use of an oral nicotine inhaler resulted in long term reduction in smoking. The study also aimed to assess the safety of nicotine replacement and smoking. A randomized, double-blinded, controlled trial was used in a university hospital setting. 400 subjects volunteered to participate in the intervention methods. 200 placebos and 200 controls were urged to limit their smoking as much as possible. Subjects reported number of cigarettes smoked each day from week 6 until month 24. Exhaled carbon monoxide levels were also recorded and compared with baseline measurements. The study found that nicotine inhalers were safe and effective in achieving sustained smoking reduction over 2 years (24 months). However, there was no statistical difference found regarding point prevalence reduction beyond month 4 between the two groups. The following is a critique of the study conducted by Bolliger et al. Introduction: The introduction of this article describes the subject matter of interest adequately. The difficulty that smokers face when attempting to quit, use of nicotine replacement as a quitting aid, and use of smoking reduction as a leeway to quitting are highlighted by referencing current literature findings and limitations. The introduction may have been strengthened by elaborating on alternative methods to nicotine inhalers and clearly indicating the magnitude of tobacco usage and consequential burden. The purpose for creating the study is clearly stated, though utilization of results is not indicated. Methods: The study design is a double-blinded, randomized, placebo-controlled, clinical trial. Subjects are recruited through newspaper advertisement and offered no compensation. Subjects may not be representative of the population as not everyone reads the newspaper or is willing to volunteer in studies without compensation. Rationale for selecting subjects meeting inclusion/exclusion criteria listed above is unclear. Initially, the sample size was fairly large, 400 subjects (n=200 treatment; n=200 placebo), however there was loss to follow up causing inadequate sample size. Data collection plans and procedures are clearly indicated with a timeline, however there is little elaboration on measurement tools and scales. One measurement selected (! 50% reduction rate) is even deemed an arbitrary value by the authors. Subjects are only power analyzed for the first four months, but are told they may keep using inhalers for 18 months. Data is analyzed out to 24 months, causing inconsistency. Case definitions and variables are not clearly described, in particular, the biologic mechanism and justification for plasma cotitionnaire levels and carbon monoxide measurements are never
addressed. Statistical procedures are vague, especially regarding power level. Odds ratios are generally not used in experimental designs, therefore do not seem appropriate to prove or disprove the hypothesis. Intention-to-treat analysis is used. This can be misleading as the study aims to search for efficacy and not effectiveness. A per-protocol analysis should have been provided in addition to measure under ideal conditions, truly estimating efficacy. Results: As mentioned, odds ratios do not seem like an appropriate method of analysis. There is no clear differentiation between the interpretation of point prevalence and sustained reduction data. The reader can see that one is shown to be significant, but there is no explanation to the meaning of these results. No methodology was used for confounders, therefore confounders were not addressed. Women are mentioned to be over sampled in the treatment group, however, sex is never adjusted for. While table and figures are easy to understand, they seem to be missing the information necessary to make them meaningful. Discussion/Conclusion: There is little comparison to other studies as the authors address this is a relatively new endeavor for the scientific community. One weakness addressed by the authors is the arbitrary threshold (! 50%) assigned for analysis. Authors also indicate that this study may not be generalizable as there are varying levels of addiction and these must be treated differently. A strength however, is the accepted carbon monoxide level of < 10 ppm. Implications of data are not mentioned in the discussion, rather in the conclusion. Data can be used to propel nicotine treatment as a useful method in tobacco reduction with hopes that reduction may lead to cessation. The conclusions regarding the possibility of smoking reduction to undermine the benefits of quitting are sound and provide the ability for the conversation regarding nicotine treatment as a stepping stone to begin. Overall, there are many flaws to this study, but there are also strengths to be highlighted. Researchers avoided bias introduced during observation recording and data analysis through double blinding. Also, sample size started out fairly large and researchers strived to compensate for non-compliance using intention-to-treat analysis. Randomization increases representativeness of the sample. Using the data as a platform for research design and discussion regarding reduction as a stepping stone to cessation is a clearly stated and explicit implication. However, while there are strengths, data may be misleading and a clear conflict of interest is present as funders are also employers/manufacturers of researchers and treatment tools. The limitations and flaws of this study outweigh the strengths, therefore I rate this article as a 5 (poor). However, poor or not, Bolliger et al. are successful in starting a new conversation for the medical community.
You might also like
- HW 7 Francis 3Document2 pagesHW 7 Francis 3api-240690004No ratings yet
- Great Starts Breakfast Survey ReportDocument42 pagesGreat Starts Breakfast Survey Reportapi-240690004No ratings yet
- Timelineupdated 1 15Document1 pageTimelineupdated 1 15api-240690004No ratings yet
- Yst - GSWB InforgraphicDocument2 pagesYst - GSWB Inforgraphicapi-240690004No ratings yet
- Di Resume 2 8Document2 pagesDi Resume 2 8api-240690004No ratings yet
- HW 7 Francis 2Document1 pageHW 7 Francis 2api-240690004No ratings yet
- 1 Fashionshowinvitation2013Document1 page1 Fashionshowinvitation2013api-240690004No ratings yet
- Infusionconfusion 6Document1 pageInfusionconfusion 6api-240690004No ratings yet
- 4 Proposal FinalDocument28 pages4 Proposal Finalapi-240690004No ratings yet
- 4 Progressive Growth EssayDocument2 pages4 Progressive Growth Essayapi-240690004No ratings yet
- 3 MethodsresearchproposalDocument11 pages3 Methodsresearchproposalapi-240690004No ratings yet
- 2 SBH Final PaperDocument12 pages2 SBH Final Paperapi-240690004No ratings yet
- 4 Bios Homework 2Document4 pages4 Bios Homework 2api-240690004No ratings yet
- Health-Education Plan For Richard BowmanDocument8 pagesHealth-Education Plan For Richard Bowmanapi-240690004No ratings yet
- 3 Casestudyfinal9 23afDocument12 pages3 Casestudyfinal9 23afapi-240690004No ratings yet
- 2 SBH BrochureoriginalDocument2 pages2 SBH Brochureoriginalapi-240690004No ratings yet
- 1 Briefing MemoDocument2 pages1 Briefing Memoapi-240690004No ratings yet
- 1 Fashionshowinvitation2013Document1 page1 Fashionshowinvitation2013api-240690004No ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- KSKV Etn1013 - Electronic Schematic DrawingDocument12 pagesKSKV Etn1013 - Electronic Schematic DrawingNur Hafizah RazaliNo ratings yet
- Toward An Ecological Theory of Autism: January 2001Document31 pagesToward An Ecological Theory of Autism: January 2001carola1344No ratings yet
- Barrier Analysis PaperDocument8 pagesBarrier Analysis PaperGustavo DucaNo ratings yet
- Suicidepreventiondraft 2Document3 pagesSuicidepreventiondraft 2api-305982723No ratings yet
- Peet CurriculumvitaeDocument7 pagesPeet Curriculumvitaeapi-405364092No ratings yet
- FFM113: Fundamentals of Theatre and Film Production Management Lecturer: Raja Nor Aminah Binti Raja AyobDocument3 pagesFFM113: Fundamentals of Theatre and Film Production Management Lecturer: Raja Nor Aminah Binti Raja AyobAKMAL DANISH ALIPENo ratings yet
- The Militant Song Movement in Latin America Chile,... - (6 The Rhythm of Values Poetry and Music in Uruguay, 1960 1985)Document22 pagesThe Militant Song Movement in Latin America Chile,... - (6 The Rhythm of Values Poetry and Music in Uruguay, 1960 1985)Flavia ManciniNo ratings yet
- CI Project Proposal TemplateDocument6 pagesCI Project Proposal TemplateDarien Tayag Aloro100% (3)
- The ICF A Framework For Setting Goals For Children With Speech Impairment PDFDocument21 pagesThe ICF A Framework For Setting Goals For Children With Speech Impairment PDFRita GonçalvesNo ratings yet
- Nepf Teacher Professional Responsibilities Rubric With EvidDocument16 pagesNepf Teacher Professional Responsibilities Rubric With Evidapi-278277795No ratings yet
- Shouldice Hospital LTD: Group Case presentation-NMP25Document9 pagesShouldice Hospital LTD: Group Case presentation-NMP25Krishna TiwariNo ratings yet
- Power, Politics N EmpowermentDocument25 pagesPower, Politics N EmpowermentMade Candra SwadayaNo ratings yet
- Chanakya National Law UniversityDocument20 pagesChanakya National Law UniversityManini JaiswalNo ratings yet
- Vineyard Model - Prayer For HealingDocument6 pagesVineyard Model - Prayer For HealingNickNo ratings yet
- Assignment #1 Clinical PsychologyDocument17 pagesAssignment #1 Clinical PsychologyKaren NguyenNo ratings yet
- 4567 Main StreetDocument3 pages4567 Main StreetNajus NaaNo ratings yet
- Chapter 3-Managing Yourself To Get Things Done: True/FalseDocument12 pagesChapter 3-Managing Yourself To Get Things Done: True/FalsedavidNo ratings yet
- The Social BrainDocument41 pagesThe Social Brainchelseabaldo020890No ratings yet
- What Is ComprehensionDocument10 pagesWhat Is ComprehensionCm AgustinNo ratings yet
- Sentence Fragments: Use This Flowchart To Test For Sentence CompletenessDocument2 pagesSentence Fragments: Use This Flowchart To Test For Sentence CompletenessCathlyn LiNo ratings yet
- 2019 - An Mhealth Intervention For The Treatment of Patients With An Eating Disorder - A Multicenter Randomized Controlled TrialDocument13 pages2019 - An Mhealth Intervention For The Treatment of Patients With An Eating Disorder - A Multicenter Randomized Controlled TrialpabobadillaNo ratings yet
- Alphabet-Vocabulary-Flashcards - ListoDocument52 pagesAlphabet-Vocabulary-Flashcards - ListonanolakesNo ratings yet
- Be Set Free Fast (BSFF)Document8 pagesBe Set Free Fast (BSFF)Panther MelchizedekNo ratings yet
- Community PsychologyDocument5 pagesCommunity PsychologyKilliam WettlerNo ratings yet
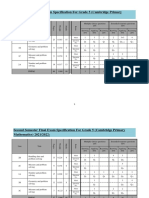
- Grade 5 Specifications CambridgeDocument2 pagesGrade 5 Specifications CambridgekatyaNo ratings yet
- Mory 2016Document35 pagesMory 2016daniela fonnegraNo ratings yet
- ESL Lesson PlanDocument4 pagesESL Lesson PlanRalph Julius DomingoNo ratings yet
- Digital Lesson PlanDocument5 pagesDigital Lesson Planapi-325767293No ratings yet
- Final ExamDocument5 pagesFinal Examkristenereeves100% (10)
- Visual Arts - Evic: This Are Lines Poised For ActionDocument6 pagesVisual Arts - Evic: This Are Lines Poised For Actionjohn evic aranteNo ratings yet