Professional Documents
Culture Documents
MechanicalLumbarDisorders RAH AlliedHealth 1201023
MechanicalLumbarDisorders RAH AlliedHealth 1201023
Uploaded by
depan_dkb32Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MechanicalLumbarDisorders RAH AlliedHealth 1201023
MechanicalLumbarDisorders RAH AlliedHealth 1201023
Uploaded by
depan_dkb32Copyright:
Available Formats
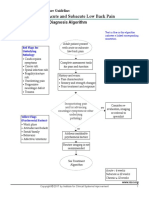
Orthopaedic Spinal Services
Lumbar disorders: mechanical lumbar disorders
>> Non-specific LBP > Radiculopathy > Spinal claudication > Acute cauda equina syndrome > Scoliosis
Clinical condition
Non-specific LBP (with or without leg symptoms) May include: >> spondylosis >> strain >> sprain >> discogenic pain >> facet joint arthropathy, >> osteoporotic compression fracture >> congenital disease (severe kypohosis/ scoliosis), spondylolysis, spondylolisthesis.
Signs and symptoms
Subjective assessment >> Predominantly LBP of varying intensity >> May complain of LL pain usually less severe than LBP and not extending beyond the knee >> Aggravated by mechanical loading or sustained positions. Eased by rest and analgesics/NSAIDs >> Acute onset may relate to a specific incident or be insidious. May be acute, episodic or chronic Objective examination >> Lumbar movements may provoke local pain and/or stiffness and show variable limitations in ROM. Proximal referral of pain may occur >> Neurological assessment is normal >> Neurodynamic tests (eg SLR) are negative
Investigations
Investigations should be considered if symptoms persist beyond 12 weeks (in the absence of red flags). Plain XR is indicated after 12 weeks if no prior XR. If ongoing medical concerns or patient anxieties consider self-funded MRI.
Management
>> Encourage early activation, provide education and advise that bed rest for longer than two days may be harmful >> Recommend conservative management involving activity pacing and regular exercise for general physical conditioning >> Narcotic analgesia should be avoided (see analgesia guideline) >> Surgical intervention is rarely indicated for non-specific LBP >> Consider community services to address smoking cessation and weight loss >> CBT is worthwhile for the management of chronic LBP
Referral
Consider referral to Spinal Outpatient Services/ Neurosurgery Department after 12 weeks if XR/ MRI reveals significant or unexpected pathology or patient is considering surgical treatment.
Radiculopathy
Subjective assessment >> Pain is predominantly in the LL in a dermatomal distribution (usually single leg only). May occur with or without LBP >> Altered sensation is localised to a single dermatome and weakness in the corresponding myotome may be reported
MRI should be considered if radicular symptoms have been present for >4-6 weeks and are severe enough to consider surgical intervention. Consider earlier investigations if neurological deficit is severe or progressive.
>> Encourage early activation and advise that bed rest for longer than two days may be harmful >> Recommend conservative management involving activity pacing and regular exercise for general physical conditioning
Spinal/Neurosurgery opinion is appropriate if symptoms persist beyond three months (in cases of persisting neurological deficits and predominantly LL pain). Earlier opinion is indicated if acute significant neurological deficit eg foot-drop.
page 1 of 3
For more information
Email: RAHspine@health.sa.gov.au Web: www.sahealth.sa.gov.au/lumbardisorders
Date of development: June 2011
11292
Orthopaedic Spinal Services
Lumbar disorders mechanical lumbar disorders
>> Non-specific LBP > Radiculopathy > Spinal claudication > Acute cauda equina syndrome > Scoliosis
Clinical condition
Signs and symptoms
>> Symptoms are aggravated by mechanical loading or sustained positions. Simple analgesics and NSAIDs may provide minimal relief >> Acute onset frequently relates to a specific incident. May be episodic or chronic
Investigations
Management
>> A trial of low-dose neuro-modulating medication may be worthwhile (see analgesia guideline) >> Evidence suggests that surgical decompression can reduce short-term symptom severity in selected cases >> Consider community services to address smoking cessation and weight loss
Referral
Spinal claudication
Subjective assessment >> Pain/sensory loss/weakness of LLs, usually bilateral and asymmetrical. Not distinctly dermatomal, often accompanied by LBP >> Symptoms are increased by walking or standing, eased by sitting, lying or flexion at the waist Objective examination >> Neurological assessment is often normal. AJ reflexes may be absent, may have mild weakness; usually L5/S1 distribution. May have signs and symptoms of single/multiple radiculopathies >> Exclude vascular cause (examine pulses) >> Cauda equina syndrome is uncommon and associated with marked neurological disability
MRI is the screening modality of choice for the diagnosis of spinal claudication. Immediate investigation required if severe or progressive neurological deficits. Consider investigation if symptoms are of sufficient duration (often several months) and severity to consider surgical intervention.
>> Conservative management involving activity pacing and regular exercise for general physical conditioning is recommended in most cases >> Epidural intervention may be considered >> Surgical decompression may be indicated in cases of severe and progressive gait limitation or by the presence/progression of neurological deficits
Consider referral to the Spinal Outpatient Services/ Neurosurgery Department if surgical opinion is required.
page 2 of 3
For more information
Email: RAHspine@health.sa.gov.au Web: www.sahealth.sa.gov.au/lumbardisorders
Date of development: June 2011
11292
Orthopaedic Spinal Services
Lumbar disorders: mechanical lumbar disorders
>> Non-specific LBP > Radiculopathy > Spinal claudication > Acute cauda equina syndrome > Scoliosis
Clinical condition
Acute cauda equina syndrome
Signs and symptoms
Subjective assessment >> Severe local back pain that may radiate into saddle area and down one or both LLs >> Bowel and bladder dysfunction urinary retention, bowel incontinence, etc >> Erectile dysfunction >> Saddle anaesthesia Objective examination >> Lower extremity muscle weakness +/- reduced or absent lower extremity reflexes. Widespread sensory deficits may be present
Investigations
Urgent MRI scanning is required.
Management
>> Immediate referral to Emergency Department >> Urgent surgical decompression may be indicated
Referral
Immediate referral to Emergency Department. Contact the spinal registrar/ fellow on call via the RAH switchboard: Tel. 8222 4000.
Scoliosis >> idiopathic >> neuromuscular >> congenital
Subjective assessment >> Frequently reports noticeable asymmetry >> Pain may indicate some underlying pathology in other structures >> Restrictive pulmonary disease may be seen in early onset (less than eight years old) idiopathic scoliosis, severe neuromuscular or severe congenital scoliosis Objective examination >> Spinal curvature, malalignment or asymmetrical posture observed >> The presence of neurological signs or symptoms increases the likelihood of a non-idiopathic cause
Standing full length postero-anterior X-ray of the spine to confirm clinical diagnosis. A Cobb angle of greater than (or equal to) 10 of curvature is diagnostic of scoliosis.
>> Management options include observation, bracing or surgery. Management depends on the magnitude of the curve and the risk of progression >> Conservative management (observation) is usually indicated if the Cobb angle is less than 20 >> Referral for specialist opinion is suggested if Cobb angle is greater than 20 or has increased by 5 degrees in one year.
For specialist opinion, please refer children under the age of 16 years to the Spinal Clinic, Womens and Childrens Hospital, North Adelaide. Tel: 8161 7000. For those over the age of 16 years, please refer to Professor Freeman, Spinal Deformity Clinic, Royal Adelaide Hospital. Tel: 8222 4466 Fax: 8222 2480.
page 3 of 3
For more information
Email: RAHspine@health.sa.gov.au Web: www.sahealth.sa.gov.au/lumbardisorders
Date of development: June 2011
11292
You might also like
- Neuromuscular DisordersDocument73 pagesNeuromuscular Disordersnurwahidah100% (1)
- Low Back Pain Red Flags 1stBRAINSDocument59 pagesLow Back Pain Red Flags 1stBRAINSSofina Lusia HarahapNo ratings yet
- Red Flag: MSK Services Pathway - Elbow PathologyDocument7 pagesRed Flag: MSK Services Pathway - Elbow PathologyMuhammed ElgasimNo ratings yet
- Spine High Yield PDFDocument81 pagesSpine High Yield PDFBimnilson SinghNo ratings yet
- Herniated Nucleus PulposusDocument41 pagesHerniated Nucleus PulposusMichael John F. Natividad100% (2)
- Yoga Therapy: Herniated Lumbar Disc - Back Pain A Structural Yoga Therapy Research PaperDocument25 pagesYoga Therapy: Herniated Lumbar Disc - Back Pain A Structural Yoga Therapy Research PaperdturkerNo ratings yet
- NP Outreach Curriculum in Rheumatology St. Joseph's Health Care, London, ON Dr. Sherry Rohekar November 12, 2009Document50 pagesNP Outreach Curriculum in Rheumatology St. Joseph's Health Care, London, ON Dr. Sherry Rohekar November 12, 2009lynkx864100% (1)
- Polymyalgia Rheumatica, A Simple Guide To The Condition, Treatment And Related DiseasesFrom EverandPolymyalgia Rheumatica, A Simple Guide To The Condition, Treatment And Related DiseasesRating: 5 out of 5 stars5/5 (2)
- SPINAL PAIN Diagnostic TriageDocument29 pagesSPINAL PAIN Diagnostic Triagenurul ulyaniNo ratings yet
- Pathology and Management of Low Back PainDocument33 pagesPathology and Management of Low Back PainSam100% (1)
- Mnemonics For Clinical Exam-OldDocument24 pagesMnemonics For Clinical Exam-OldDrAmeen1976100% (1)
- Cervical Stenosis 2006Document16 pagesCervical Stenosis 2006kppsadiNo ratings yet
- Mnemonics For Clinical ExamDocument20 pagesMnemonics For Clinical ExamDrAmeen1976100% (3)
- Spine and Spinal Cord InjuryDocument39 pagesSpine and Spinal Cord InjuryblackcatNo ratings yet
- Ortho Conus Medullaris and Cauda Equina SyndromeDocument16 pagesOrtho Conus Medullaris and Cauda Equina Syndromemohamed100% (1)
- Complex Regional Pain SyndromeDocument10 pagesComplex Regional Pain SyndromegeejeiNo ratings yet
- Physical Therapy Protocols For Conditions of Shoulder RegionDocument111 pagesPhysical Therapy Protocols For Conditions of Shoulder RegionPieng Napa100% (1)
- Classical Disc Herniation by DR Anupreet BassiDocument17 pagesClassical Disc Herniation by DR Anupreet Bassidr_bassiNo ratings yet
- A Simple Guide to Slipping Rib Syndrome, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Slipping Rib Syndrome, Diagnosis, Treatment and Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Achilles TendinopathyDocument9 pagesAchilles TendinopathysynysterbraveNo ratings yet
- Management of Back Pain in AdultsDocument41 pagesManagement of Back Pain in AdultsMadhusree GhoshNo ratings yet
- Benign Fasciculation Syndrome, (Muscle Twitching) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandBenign Fasciculation Syndrome, (Muscle Twitching) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Low Back PainDocument17 pagesLow Back PainRamon Salinas AguileraNo ratings yet
- Radiology 101 The Basics & Fundamentals of Imaging - 4E (PDF) (UnitedVRG)Document17 pagesRadiology 101 The Basics & Fundamentals of Imaging - 4E (PDF) (UnitedVRG)claudedNo ratings yet
- Physical Therapy For Herniated DiscsDocument28 pagesPhysical Therapy For Herniated DiscswidiaNo ratings yet
- Low Back Pain HPNDocument39 pagesLow Back Pain HPNRussel Janolo100% (1)
- Lumbar Disc HerniationDocument8 pagesLumbar Disc Herniationandra_scooterNo ratings yet
- ENTPDocument5 pagesENTPIsmail Lubis0% (1)
- MimicSpinalDisorders RAH AlliedHealth 120123Document4 pagesMimicSpinalDisorders RAH AlliedHealth 120123KurbulNo ratings yet
- Family Medicine DepartmentDocument45 pagesFamily Medicine Departmentسليمان فايزNo ratings yet
- ICD-9-CM Code: 724.3 ICF CodesDocument8 pagesICD-9-CM Code: 724.3 ICF CodesGeorgiana MilcoveanuNo ratings yet
- Presentation Lower Back PainDocument86 pagesPresentation Lower Back PainSten SchaperNo ratings yet
- Low Back Pain Presentation IMPDocument114 pagesLow Back Pain Presentation IMPrapannika100% (3)
- North American Spine Society Public Education SeriesDocument12 pagesNorth American Spine Society Public Education Serieseryoktadiputra565No ratings yet
- Trauma Saraf SpinalDocument41 pagesTrauma Saraf SpinalFatahillah NazarNo ratings yet
- Name: Biadsi Odey Group:M1560 SUBJECT: Rheumatology (Patenit Presentation) - Data: 31/03/2019Document10 pagesName: Biadsi Odey Group:M1560 SUBJECT: Rheumatology (Patenit Presentation) - Data: 31/03/2019Galina LozovanuNo ratings yet
- Low Back Pain: Management Update: DR Dewanta Sembiring, SpsDocument46 pagesLow Back Pain: Management Update: DR Dewanta Sembiring, SpsYoke RetnaningpuriNo ratings yet
- Back PainDocument3 pagesBack PainShaz ChindhyNo ratings yet
- Exercise 1Document4 pagesExercise 1api-479716004No ratings yet
- Acute Low Back PainDocument27 pagesAcute Low Back PainGalih Cakhya ImawanNo ratings yet
- Tutorial Low Back Pain: Rahma Herviastuti 12/329221/KU/14991 Pembimbing: Dr. Wahyu Wihartono, SP.S, M.KesDocument40 pagesTutorial Low Back Pain: Rahma Herviastuti 12/329221/KU/14991 Pembimbing: Dr. Wahyu Wihartono, SP.S, M.KesRahma HerviastutiNo ratings yet
- Trigonum Low Back Pain FixDocument37 pagesTrigonum Low Back Pain FixsilvaNo ratings yet
- Motion SicknessDocument3 pagesMotion SicknessJessica FredelinaNo ratings yet
- Multiple Sclerosis: Case Study by Trcoski ElenaDocument43 pagesMultiple Sclerosis: Case Study by Trcoski ElenaElena TrcoskiNo ratings yet
- Cervical Myelopathy - ERHDocument42 pagesCervical Myelopathy - ERHAries RHNo ratings yet
- TremorDocument14 pagesTremorEcaterina LungociuNo ratings yet
- Back PainDocument31 pagesBack PainSaif SinghNo ratings yet
- Weebly Questions Week TwoDocument3 pagesWeebly Questions Week Twoapi-459697337No ratings yet
- Spasticity Management GuidelinesDocument13 pagesSpasticity Management GuidelinesRaluca AndreeaNo ratings yet
- Care of Patients With Problems of The CNS-Spinal CordDocument34 pagesCare of Patients With Problems of The CNS-Spinal CordjacobNo ratings yet
- File 1694763811 0005620 SpasticityDocument17 pagesFile 1694763811 0005620 Spasticity2022824838.pasangNo ratings yet
- Week 7 Case Study 7 Chir13009 Tutors Notes 1Document10 pagesWeek 7 Case Study 7 Chir13009 Tutors Notes 1api-502171898No ratings yet
- CHIR12007 Clinical Assessment and Diagnosis Portfolio Exercises Week 5Document4 pagesCHIR12007 Clinical Assessment and Diagnosis Portfolio Exercises Week 5api-479849199No ratings yet
- Functional Disorders As An Impact of Diabetic NeuropathyDocument30 pagesFunctional Disorders As An Impact of Diabetic NeuropathyshintiasspNo ratings yet
- Week 7 Case Study 7 Chir13009Document12 pagesWeek 7 Case Study 7 Chir13009api-468597987No ratings yet
- ARHM 2013StrokeSymposium RicciDocument20 pagesARHM 2013StrokeSymposium RicciEdsel JavellanaNo ratings yet
- Low Back Pain: Aldy S. RambeDocument40 pagesLow Back Pain: Aldy S. RambeHatta Diana TariganNo ratings yet
- Spine Trauma: Dr. Elvira CesarenaDocument65 pagesSpine Trauma: Dr. Elvira CesarenadrelvNo ratings yet
- Exercise 1: CHIR12007 Clinical Assessment and Diagnosis Portfolio Exercises Week 5Document3 pagesExercise 1: CHIR12007 Clinical Assessment and Diagnosis Portfolio Exercises Week 5api-468597987No ratings yet
- Low Back Pain (LBP)Document16 pagesLow Back Pain (LBP)HusseinNo ratings yet
- Osteoarthritis: Uyenvy Pham, M.D. Swedish Geriatric Fellow March 22, 2011Document45 pagesOsteoarthritis: Uyenvy Pham, M.D. Swedish Geriatric Fellow March 22, 2011Saya MenangNo ratings yet
- 64.ataxia (Presented by Zeeshan Ahmad Roll No 65)Document40 pages64.ataxia (Presented by Zeeshan Ahmad Roll No 65)Zeeshan AhmadNo ratings yet
- Abnormal Spine CurvaturesDocument7 pagesAbnormal Spine CurvaturesMartin SageNo ratings yet
- Guillain Barre SyndromeDocument6 pagesGuillain Barre SyndromeBeaulahNo ratings yet
- Cerebral Palsy: Nisrin Alqatarneh MSC Ot Thanks To Dr. Sumaya MalkawiDocument111 pagesCerebral Palsy: Nisrin Alqatarneh MSC Ot Thanks To Dr. Sumaya Malkawilama mansourNo ratings yet
- Spine Disease and Fractures For StudentsDocument79 pagesSpine Disease and Fractures For StudentsAbdullah MohdNo ratings yet
- Parkinson's DiseaseDocument25 pagesParkinson's DiseaseArko duttaNo ratings yet
- Stroke Rehabilitation: Dr. Retno Setianing, SPRMDocument32 pagesStroke Rehabilitation: Dr. Retno Setianing, SPRMamalia hafidhahNo ratings yet
- Physiotherapy Management of Complications in Patients With Motor Neuron Disease (MND)Document10 pagesPhysiotherapy Management of Complications in Patients With Motor Neuron Disease (MND)YangNo ratings yet
- Peer Review Process: Author: Section Editor: Deputy EditorDocument10 pagesPeer Review Process: Author: Section Editor: Deputy EditorLuis Enrique Caceres AlavrezNo ratings yet
- Stemi Inferior BanisDocument27 pagesStemi Inferior BanisIsmail LubisNo ratings yet
- Cleft Lip and Cleft PalateDocument16 pagesCleft Lip and Cleft PalateIsmail LubisNo ratings yet
- B. Disorders of Hyperpigmentation: 1. EphelidesDocument4 pagesB. Disorders of Hyperpigmentation: 1. EphelidesIsmail LubisNo ratings yet
- Family ApgarDocument6 pagesFamily ApgarunjyilNo ratings yet
- Pressure:: Minimal Pressure High PressureDocument1 pagePressure:: Minimal Pressure High PressureIsmail LubisNo ratings yet
- Income Satisfaction:: Very Dissatisfied Highly SatisfiedDocument1 pageIncome Satisfaction:: Very Dissatisfied Highly SatisfiedIsmail LubisNo ratings yet
- INTPDocument5 pagesINTPIsmail LubisNo ratings yet
- Would I Go On A Date With You?: Sure!Document1 pageWould I Go On A Date With You?: Sure!Ismail LubisNo ratings yet
- Autonomy:: Great Deal of Autonomy Very Limited AutonomyDocument1 pageAutonomy:: Great Deal of Autonomy Very Limited AutonomyIsmail LubisNo ratings yet
- Dyspnea (Chronic) HPWDocument1 pageDyspnea (Chronic) HPWIsmail LubisNo ratings yet
- Responsibility:: Limited Responsibility Sole ResponsibilityDocument1 pageResponsibility:: Limited Responsibility Sole ResponsibilityIsmail LubisNo ratings yet
- 14 Surgical Procedures Discectomy and HerniectomyDocument10 pages14 Surgical Procedures Discectomy and Herniectomydrkis200No ratings yet
- Herniated Lumbar Intervertebral Disk: Epidemiology and Natural HistoryDocument6 pagesHerniated Lumbar Intervertebral Disk: Epidemiology and Natural HistoryGeysel SuarezNo ratings yet
- Neuro No 1Document3 pagesNeuro No 1Marcela YolinaNo ratings yet
- Spinal Cord Injury: C M, S - P J - LDocument99 pagesSpinal Cord Injury: C M, S - P J - Lsheel1No ratings yet
- A Case Study of Cauda Equina SyndromeDocument5 pagesA Case Study of Cauda Equina SyndromeProfessor Stephen D. Waner100% (5)
- EM Cases Course Pre Course Handbook 2016Document27 pagesEM Cases Course Pre Course Handbook 2016Malik UsmanNo ratings yet
- Abstracts - Final Off Print BJNDocument57 pagesAbstracts - Final Off Print BJNZieshNo ratings yet
- Management of Cauda Equina Syndrome by Full Endoscopic Interlaminar Decompression A Case ReportDocument4 pagesManagement of Cauda Equina Syndrome by Full Endoscopic Interlaminar Decompression A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Cauda Equina SyndromeDocument15 pagesCauda Equina SyndromeAdhi Surya NegaraNo ratings yet
- Spinal Cord InjuriesDocument49 pagesSpinal Cord Injuriesjustin_saneNo ratings yet
- Clinical Features and Diagnosis of Neoplastic Epidural Spinal Cord Compression - UpToDateDocument19 pagesClinical Features and Diagnosis of Neoplastic Epidural Spinal Cord Compression - UpToDatePrincess Jeanne Roque GairanodNo ratings yet
- Low Back Pain Anatomy of Thoracolumbar SpineDocument10 pagesLow Back Pain Anatomy of Thoracolumbar SpineMNo ratings yet
- Red Flag LBPDocument4 pagesRed Flag LBPnabella cholidatunNo ratings yet
- Subacute Low Back PainDocument49 pagesSubacute Low Back Painsayid najibullahNo ratings yet
- Cauda Equina Syndrom in Hernia Nukleus Pulposus: Dr. Riski AmandaDocument46 pagesCauda Equina Syndrom in Hernia Nukleus Pulposus: Dr. Riski AmandaMagista NugrahaNo ratings yet
- Dor LombarDocument27 pagesDor LombarLeonardoCampanelliNo ratings yet
- Goodman & Snyder: Differential Diagnosis For Physical Therapists, 5th EditionDocument4 pagesGoodman & Snyder: Differential Diagnosis For Physical Therapists, 5th EditionCyndi MenesesNo ratings yet
- Overview of Tool and Key Points: Section A: HistoryDocument4 pagesOverview of Tool and Key Points: Section A: HistoryM Naeem ArhamNo ratings yet
- Red Flags Presented in Current Low Back Pain Guidelines: A ReviewDocument15 pagesRed Flags Presented in Current Low Back Pain Guidelines: A ReviewVictor Andrés Olivares IbarraNo ratings yet
- Bilateral Lower Extremity Weakness English Script TextDocument3 pagesBilateral Lower Extremity Weakness English Script TextIsaac AffamNo ratings yet
- Low Back PainDocument7 pagesLow Back PainPutriDundaNo ratings yet