Professional Documents
Culture Documents
Nejmvcm0706756 2
Nejmvcm0706756 2
Uploaded by
Daru KristiyonoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nejmvcm0706756 2
Nejmvcm0706756 2
Uploaded by
Daru KristiyonoCopyright:
Available Formats
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
videos in clinical medicine
Tympanocentesis in Children with Acute Otitis Media
Nader Shaikh, M.D., M.P.H., Alejandro Hoberman, M.D., Diana H. Kearney, R.N., C.C.R.C., and Robert Yellon, M.D.
Overview
Tympanocentesis involves needle aspiration of fluid from the middle ear. Familiarity with this procedure enables primary care practitioners to effectively treat patients who have refractory acute otitis media.
Indications
In children with refractory acute otitis media, drainage of pus from the middle ear often results in a rapid and marked abatement of symptoms. In addition, identification of pathogens from the fluid specimen obtained enables tailored antimicrobial therapy. The American Academy of Pediatrics recommends that tympanocentesis be considered in children who have signs and symptoms of acute otitis media that persist after two courses of antibiotic treatment.1 In immunocompromised children and ill-appearing neonates with acute otitis media, unusual or resistant organisms can be identified through tympanocentesis. In children with suppurative complications of acute otitis media, such as mastoiditis or facial paralysis, tympanocentesis allows for drainage and can provide immediate relief from pressure and pain.
Contraindications
From the Department of Pediatrics (N.S., A.H., D.H.K.) and the Department of Pediatric Otolaryngology (R.Y.), Childrens Hospital of Pittsburgh of UPMC, University of Pittsburgh School of Medicine. Address reprint requests to Dr. Shaikh at Childrens Hospital of Pittsburgh of UPMC, One Childrens Hospital Drive, 4401 Penn Ave., Pittsburgh, PA 15224, or at nader.shaikh@chp.edu. This article (10.1056/NEJMvcm0706756) was published on January 12, 2011, at NEJM.org. N Engl J Med 2011.
Copyright 2011 Massachusetts Medical Society.
Tympanocentesis is contraindicated in children with tympanostomy tubes and in children with congenital stenosis of the external auditory canal.
Preparation
To prepare for the procedure, explain the risks and benefits to the parent or guardian and document informed consent in the medical record. Proper analgesia should be administered 30 minutes before the procedure. Acetaminophen plus codeine (1 mg of codeine per kilogram of body weight) can be used as oral analgesia. Alternatively, a cotton ball soaked with 8% tetracaine may be inserted into the external auditory canal 30 minutes before the procedure.
Equipment
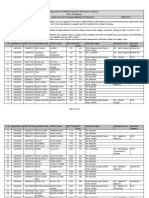
The following equipment is necessary: a papoose board; a surgical otoscope with speculum; a mechanical suction device; a tympanocentesis aspirator with a 3-in., 18-gauge spinal-tap needle (Fig. 1); a second aspirator with flexible tubing; and cotton balls. The suction device can usually be set to medium, although the strength of the suction at any one setting will vary with the equipment used. If the suction is set at the maximal setting, the specimen may be drawn into the tubing and lost. If a tympanocentesis aspirator is not available, a 3-ml syringe can be connected to a 3-in., 18-gauge spinal-tap needle that is bent at its midpoint to a 30-degree angle. Given the manipulation required to bend the needle and the relatively weaker suction achieved when using a syringe, this is not the preferred method.
10.1056/nejmvcm0706756 nejm.org
Figure 1. Tympanocentesis Aspirator with Needle.
The New England Journal of Medicine Downloaded from nejm.org on April 4, 2014. For personal use only. No other uses without permission. Copyright 2011 Massachusetts Medical Society. All rights reserved.
Tympanocentesis in Children with Acute Otitis Media
Procedure
Figure 2. Site of Needle Insertion. The needle should be inserted in the inferior portion (gray shading) of the tympanic membrane.
Fully immobilize the child on a papoose board and have an assistant secure the childs head. Cerumen should be removed before the procedure is begun. With your dominant hand, insert the otoscope into the external auditory canal and visualize the umbo and the annulus. Once the otoscope is in the proper position, switch hands, so that you are holding the instrument in place with your nondominant hand. Insert the needle that is attached to the tympanocentesis aspirator, which is attached to the suction device. Under direct visualization, advance the needle toward the tympanic membrane, keeping your thumb poised over the orifice of the tympanocentesis aspirator without occluding it. Insert the bevel of the needle through the inferior portion of the tympanic membrane, 2 to 3 mm above its inferior rim (Fig. 2). Immediately after penetrating the tympanic membrane, place your thumb on the orifice of the tympanocentesis aspirator and start suctioning fluid from the middle ear. Once pus is visualized in the aspirator, promptly remove your thumb from the aspirator to avoid losing the specimen to the suction tubing. Use a second tympanocentesis aspirator with a flexible catheter to suction any remaining pus from the middle ear. Insert the catheter through the speculum and place it over the opening in the tympanic membrane made by the needle. The catheter should not go through the tympanic membrane. This step also clears the debris in the external auditory canal and will enhance visualization of the tympanic membrane at future visits. Place a small cotton pledget in the external auditory canal to absorb any remaining blood or pus, and release the child from the restraint. Remove the plastic receptacle from the tympanocentesis aspirator and send the specimen for microbiologic evaluation.
Complications
The incidence of complications of tympanocentesis has not been studied systematically but appears to be extremely low. Complications include disruption of the ossicles, piercing of the oval or round windows, laceration of the facial nerve or the chorda tympani, bleeding from a high-riding bulb of the internal jugular vein, and chronic perforation of the tympanic membrane. The likelihood of incurring complications can be minimized by ensuring adequate immobilization, bracing the hands against the childs head, and paying careful attention to the point of needle insertion. Damage to the oval window, the ossicles, or the facial nerve can be prevented by ensuring that the needle is inserted in the inferior portion of the tympanic membrane (Fig. 2). Bleeding can be minimized by avoiding the umbo and annulus. In case of profuse bleeding from either the external auditory canal or a prominent jugular-vein bulb, the external auditory canal can be packed with a cotton ball soaked in oxymetazoline. Having the child sit up and having the parent soothe the child may also help to reduce bleeding.
Follow-up
Oral and topical antimicrobial therapy is generally initiated after the procedure, while the results of the culture are being awaited. Pathogenic bacteria are detected in the specimens from approximately 70 to 80% of patients with acute otitis media. The results of Grams staining of the specimen and the susceptibility pattern of the isolated bacteria (generally available within 2 days) should be used to guide antimicrobial therapy. The small perforation in the tympanic membrane made during tympanocentesis usually heals in 2 to 3 days; some serosanguineous drainage during this period is normal. For the first 3 days after the procedure, a cotton ball
2
10.1056/nejmvcm0706756
nejm.org
The New England Journal of Medicine Downloaded from nejm.org on April 4, 2014. For personal use only. No other uses without permission. Copyright 2011 Massachusetts Medical Society. All rights reserved.
Tympanocentesis in Children with Acute Otitis Media
coated with petroleum jelly should be used during bathing to keep water out of the childs external auditory canal. A follow-up examination should be scheduled for 3 or 4 days after the procedure.
Summary
References 1. Diagnosis and management of acute otitis media. Pediatrics 2004;113:1451-65.
Copyright 2011 Massachusetts Medical Society.
Tympanocentesis is an underused procedure. Clinicians should become familiar with tympanocentesis so that they can safely perform the procedure in children with acute otitis media.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
10.1056/nejmvcm0706756
nejm.org
The New England Journal of Medicine Downloaded from nejm.org on April 4, 2014. For personal use only. No other uses without permission. Copyright 2011 Massachusetts Medical Society. All rights reserved.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Certified Coding Specialist CCS Exam Preparation OCRDocument319 pagesCertified Coding Specialist CCS Exam Preparation OCRKian Gonzaga100% (32)
- 82 Where The Sidewalk Ends - Silverstein, Shel PDFDocument88 pages82 Where The Sidewalk Ends - Silverstein, Shel PDFMadhu Kohli100% (17)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- E TicketDocument2 pagesE TicketmusytazabNo ratings yet
- E TicketDocument2 pagesE TicketmusytazabNo ratings yet
- Application Letter (Default)Document1 pageApplication Letter (Default)musytazabNo ratings yet
- Curriculum VitaeDocument1 pageCurriculum VitaemusytazabNo ratings yet
- Lexical Cohesion and The Organization of Discourse: First Year ReportDocument35 pagesLexical Cohesion and The Organization of Discourse: First Year ReportmusytazabNo ratings yet
- Kualitas Hidup Salah Satu Indikator Yogya (DR Maria)Document45 pagesKualitas Hidup Salah Satu Indikator Yogya (DR Maria)Yuliarni HasanNo ratings yet
- Page 1 of 44Document44 pagesPage 1 of 44tarini.goyalNo ratings yet
- Jurnal ImunologiDocument7 pagesJurnal ImunologiSisQha LuCiiajjaNo ratings yet
- Central University of Applied Sciences, Department of PharmacyDocument10 pagesCentral University of Applied Sciences, Department of PharmacyBoas WayneNo ratings yet
- Presentation For After SITE VISITDocument11 pagesPresentation For After SITE VISITGauri LalNo ratings yet
- Sedation Policy LPCH 6 11Document24 pagesSedation Policy LPCH 6 11Tribowo WicaksonoNo ratings yet
- Proximate Composition Mineral and Lipid Profile of Malaysian Artemisia Argyi 2Document5 pagesProximate Composition Mineral and Lipid Profile of Malaysian Artemisia Argyi 2International Journal of Innovative Science and Research TechnologyNo ratings yet
- Total Gastrectomy ConsentDocument18 pagesTotal Gastrectomy ConsentTanyaNganNo ratings yet
- EvaluationDocument2 pagesEvaluationfatimaadessaNo ratings yet
- Breast AugmentationDocument7 pagesBreast AugmentationnikitagustiNo ratings yet
- Vitamin & Mineral (Nutrisi Ternak Non-Ruminaisia)Document14 pagesVitamin & Mineral (Nutrisi Ternak Non-Ruminaisia)Mawardi A AsjaNo ratings yet
- Ndodontic: Rnaldo Astellucci MD DDSDocument399 pagesNdodontic: Rnaldo Astellucci MD DDSFernanda CombaNo ratings yet
- API Product ListDocument4 pagesAPI Product ListpstindiaNo ratings yet
- Activity IntoleranceDocument2 pagesActivity Intolerancejunex123No ratings yet
- Renew Bariatrics Offers All-Inclusive Medical Tourism PackagesDocument2 pagesRenew Bariatrics Offers All-Inclusive Medical Tourism PackagesPR.comNo ratings yet
- MPKAY v1003Document39 pagesMPKAY v1003Pranil MestryNo ratings yet
- ABC's of Abg Part 2Document38 pagesABC's of Abg Part 2Sheena Mae GonzagaNo ratings yet
- Kalasag 2nd Issue May2009Document10 pagesKalasag 2nd Issue May2009AlvinMatabangNo ratings yet
- Jurnal Kontap InternasionalDocument5 pagesJurnal Kontap InternasionalNGADIRAHNo ratings yet
- UmbilikusDocument4 pagesUmbilikusAnel RedzepiNo ratings yet
- Pulsed Radiofrequency ofDocument8 pagesPulsed Radiofrequency ofDiego Pinto PatroniNo ratings yet
- Two Dimensional and M-Mode Echocardiography - BoonDocument112 pagesTwo Dimensional and M-Mode Echocardiography - BoonRobles RobertoNo ratings yet
- Aromatherapy Associates DejnuyoDocument5 pagesAromatherapy Associates Dejnuyobaroqueclothing4269No ratings yet
- Circumcision Using The Mogen ClampDocument4 pagesCircumcision Using The Mogen ClampJorge AndrésNo ratings yet
- Worksheet On Exercise No. 7 Case Study On Diabetes MellitusDocument10 pagesWorksheet On Exercise No. 7 Case Study On Diabetes MellitusShannen CostoNo ratings yet
- Freud Teaches Psychotherapy 2nd EdDocument889 pagesFreud Teaches Psychotherapy 2nd Edkiki011100% (2)
- Low Back Pain and CyclingDocument3 pagesLow Back Pain and Cyclinglukabog100% (1)
- Bag TechniqueDocument64 pagesBag TechniqueKailash Nagar100% (1)
- 3.skin PathologyDocument38 pages3.skin PathologyFaisal MehboobNo ratings yet