Professional Documents
Culture Documents
Tetanus: Andrew Michael Taylor FRCA
Tetanus: Andrew Michael Taylor FRCA
Uploaded by
Ryan Haryana DarajatunOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tetanus: Andrew Michael Taylor FRCA
Tetanus: Andrew Michael Taylor FRCA
Uploaded by
Ryan Haryana DarajatunCopyright:
Available Formats
Tetanus
Andrew Michael Taylor FRCA
Tetanus is caused by a neurotoxin released by Clostridium tetani, a spore-forming anaerobic bacterium. It occurs throughout the world and remains an important cause of death with an estimated annual mortality of 800 000 1 000 000. Over half of these deaths are in neonates. Tetanus is relatively rare in the developed world. For example, there are 510 cases per year in the UK; 75% of these occur in individuals over the age of 45 yr. There have been no cases in the UK of tetanus in the newborn for over 30 yr. Tetanus is a clinical diagnosis. Individuals with symptoms and signs of tetanus should be closely monitoredideally within an intensive care unit with immediate access to ventilatory support. Modern management encompasses wound debridement, antimicrobial therapy, active and passive immunization, sedation and vigilant monitoring.
Pathophysiology
C. tetani spores are widespread in the environment residing in soil, faeces and dust.3 Tetanus spores are extremely hardy and can survive extreme conditions for prolonged periods. They usually enter the body after contamination of an abrasion or minor puncture wound, although, in 20% of cases, no entry site can be found. Spores also gain entry through skin ulcers, abscesses, gangrene, burns or after abdominal/pelvic surgery, childbirth and abortion.4 The incubation period of the disease is between 3 and 21 days (average 7 days). The manifestations of tetanus are caused by tetanospasmin, which is released by the tetanus bacillus on entry into the body. Symptoms arise 12 weeks after infection. Tetanospasmin is an extremely potent neurotoxin; it is estimated that as little as 240 g is enough to kill the entire world population. The toxin spreads into the nervous system by binding to the neuromuscular junction. Once bound, it is transported retrogradely to the cell body. Further spread occurs trans-synaptically to adjacent motor and autonomic nerves.4 Tetanospasmin exerts its effect by cleaving synaptobrevin, a vesicle-associated membrane protein which is essential for the release of neurotransmitter. The toxin primarily affects inhibitory pathways, preventing the release of glycine and g-amino butyric acid (GABA). When interneurones inhibiting alpha motor neurones are affected, there is failure to inhibit motor reflexes. This causes increased muscle tone and rigidity, interposed by sudden and potentially devastating muscle spasms. Muscles of the face are affected early because of their short axonal pathways. Sympathetic neurones become affected later in the disease. Disinhibited autonomic discharge leads to loss of autonomic control, resulting in sympathetic overactivity and increased catecholamine levels. Neuronal binding of the toxin is irreversible. Recovery requires the growth of new nerve terminals, which explains the prolonged duration of the disease.
Key points Tetanus is a preventable disease; it is a significant cause of mortality worldwide causing one million deaths annually. At least 20 cases of tetanus occur in the UK each year.
Downloaded from http://ceaccp.oxfordjournals.org/ by guest on July 27, 2013
Management of tetanus is essentially supportive using antibiotics, surgery, immunization, sedation and, when necessary, ventilation. The mortality from tetanus remains high despite modern intensive care.
Epidemiology
Tetanus is an entirely preventable disease; the first vaccine was produced in 1924. Routine vaccination began in the UK in 1961. It is given as a combined vaccine along with diphtheria and pertussis (DPT). Unfortunately, immunity to tetanus may not be life-long and booster injections may be required after individuals sustain tetanus-prone wounds. Tetanus immunization guidelines are available in the British National Formulary.1 Poor access to a programme of immunization accounts for the high prevalence of the disease in the developing world. Implementation of global tetanus immunization has been a target of the World Health Organization since 1974. Recently there has been a cluster of tetanus cases amongst injecting drug-users in the UK. Twenty-four cases were reported between 2003 and 2004. The majority of these had no record of (or, at best, incomplete) immunization. This outbreak is thought to be a result of a batch of contaminated heroin.2 I.M or s.c. drug-use is a particularly high risk activity for developing tetanus.
Andrew Michael Taylor FRCA Consultant Anaesthetist Department of Anaesthesia Nottingham University Hospitals NHS Trust Nottingham NG7 2UH UK Tel: 0115 9249924 Fax: 0115 970 0739 E-mail: andytanaes@hotmail.com
doi:10.1093/bjaceaccp/mkl014 Continuing Education in Anaesthesia, Critical Care & Pain | Volume 6 Number 3 2006 The Board of Management and Trustees of the British Journal of Anaesthesia [2006]. All rights reserved. For Permissions, please email: journals.permissions@oxfordjournals.org
101
Tetanus
Mortality
In developing countries, the mortality from tetanus exceeds 50%. Death occurs mainly from acute respiratory failure. In the developed world, with intensive care support, mortality is around 10%, rising to 20% in severe cases. Mortality increases with increasing age (exceeding 50% if more than 60 yr old) and previously unvaccinated individuals (22%). A short incubation period (<5 days) signifies more severe disease. The severity of illness may be decreased by partial immunity.
Table 1 Ablett classification of tetanus severity Grade 1 (mild) Mild trismus, general spasticity, no respiratory compromise, no spasms, no dysphagia Grade 2 (moderate) Moderate trismus, rigidity, short spasms, mild dysphagia, moderate respiratory involvement, ventilatory frequency >30 Grade 3 (severe) Severe trismus, generalized rigidity, prolonged spasms, severe dysphagia, apnoeic spells, pulse >120, ventilatory frequency >40 Grade 4 (very severe) Grade 3 with severe autonomic instability
Clinical features
Table 2 Differential diagnosis of tetanus
Tetanus is a clinical diagnosis characterized by a triad of muscle rigidity, muscle spasms and autonomic instability. Early symptoms of tetanus include neck stiffness, sore throat, dysphagia and trismus. Muscle spasms are extremely painful. They occur spontaneously but are also provoked by touch, visual, auditory or emotional stimuli. Muscle spasms can be so intense that they cause tendon rupture, joint dislocation and bone fractures. Spasm extending to the facial muscles causes the typical facial expression, risus sardonicus. Truncal spasm causes opisthotonus. During prolonged spasms, severe hypoventilation and life-threatening apnoea may occur. Laryngeal spasms also occur resulting in sudden airway obstruction and respiratory arrest. Severe tetanus is associated with profound autonomic instability. This usually starts a few days after the spasms and lasts 12 weeks. Increased sympathetic tone causes vasoconstriction, tachycardia and hypertension. Autonomic storms are associated with raised catecholamine levels. These alternate with episodes of sudden hypotension, bradycardia and asystole. Other features of autonomic disturbance include salivation, sweating, increased bronchial secretions, hyperpyrexia, gastric stasis and ileus.
Hypocalcaemic tetany Epilepsy Chorea Meningitis Encephalitis Subarachnoid haemorrhage Strychnine poisoning Rabies Sepsis Drug withdrawal
Downloaded from http://ceaccp.oxfordjournals.org/ by guest on July 27, 2013
Grading severity
There are several grading systems; the scale proposed by Ablett5 is the most widely used (Table 1). This categorizes patients into four grades depending upon the intensity of spasms, and respiratory and autonomic involvement.
Differential diagnosis
Tetanus is a purely clinical diagnosis. The differential diagnosis is listed in Table 2.
Management
Classification of tetanus
Four different forms of tetanus are described; local, cephalic, generalized and neonatal. In local tetanus, spasm and rigidity are confined to the site of injury. It is an uncommon and relatively mild form of tetanus with a low mortality (1%). Cephalic tetanus occurs after a wound to the head and neck or otitis media. It is characterized by cranial nerve palsies (especially the seventh) and leads to paralysis; it is associated with a high mortality. The most common type is generalized tetanus which is responsible for 80% of cases. It results from the haematogenous spread of the toxin. The muscles of the head and neck are affected first with progressive distal spread of spasm and rigidity throughout the body. Neonatal tetanus is responsible for over 50% of deaths associated with tetanus. It is caused by poor umbilical hygiene and is entirely preventable by maternal vaccination. It carries a poor prognosis. Neonatal tetanus has been completely eliminated from the UK. All patients suspected of tetanus should be managed on an intensive care unit. To minimize the risk of precipitating spasms, the patient should be nursed in a dark, quiet room. A low threshold to secure the airway must be maintained at all times and constant vigilance is required. Patients with respiratory distress should be intubated immediately. Death caused by sudden laryngospasm, diaphragmatic paralysis, and inadequate respiratory muscle contraction is a frequent occurrence in parts of the developing world where there is no immediate access to ventilatory support.
Neutralization of unbound toxin
Free circulating toxin should be neutralized with human tetanus immunoglobulin (HTIG); HTIG does not affect toxin which is already fixed to nerve terminals. It has a long half-life (23 days) and does not need to be repeated. There is no consensus on the correct dose of HTIG; 500010 000 units by infusion is
102
Continuing Education in Anaesthesia, Critical Care & Pain | Volume 6 Number 3 2006
Tetanus
recommended in the British National Formulary.1 HTIG is given on a named-patient basis. Recovery from tetanus does not result in immunity and vaccination with tetanus toxoid is indicated during the convalescent stage of the disease.
its cardiostability. The use of aminosteroid neuromuscular blocking agents is not recommended because of their association with critical care neuropathy.
Control of autonomic instability Surgical debridement
If present, the infected site should be cleaned thoroughly and necrotic tissue extensively debrided to reduce the bacterial and toxin load. A number of antibiotics are effective in eradicating the tetanus bacterium. Metronidazole is the antibiotic of choice. The recommended regimen is 500 mg 8-hourly for 710 days. Erythromycin, tetracycline, chloramphenicol and clindamycin are each acceptable alternatives. The use of penicillin in proven cases of tetanus remains controversial; one randomized, controlled trial showed that patients treated with penicillin had a higher mortality when compared with metronidazole (24% vs 7%; P < 0.01).6 A major cause of mortality in tetanus is circulatory collapse caused by autonomic instability. Sudden cardiac arrest is common and is thought to be precipitated by a combination of high catecholamine levels and the direct action of the tetanus toxin on the myocardium. Prolonged sympathetic activity may end with profound hypotension and bradycardia. Parasympathetic over activity may lead to sinus arrest. Direct damage to the vagal nucleus by the tetanus toxin has been implicated. High dose atropine (up to 100 mg h1) has been advocated where bradycardia is a prominent feature. Sedation is also the first line manoeuvre to control autonomic instability. Morphine is particularly useful and is effective in decreasing catecholamine output. b-Blockade, although theoretically useful to control episodes of hypertension and tachycardia, is associated with sudden cardiovascular collapse, pulmonary oedema and death. Other agents that have been used include clonidine and magnesium. Clonidine is an a2-adrenergic agonist which reduces sympathetic outflow, arterial pressure, heart rate and catecholamine release. It can be administered orally or parenterally and is, in addition, a sedative. Magnesium is increasingly being utilized as part of multimodal therapy for tetanus.7 It has a number of actions which are effective in countering the state of autonomic hyperactivity; in particular, blocking catecholamine release from nerves and the adrenal medulla, and reducing receptor responsiveness to released catecholamines. It is also a pre-synaptic neuromuscular blocker, becoming a useful adjunct in the control of rigidity and spasms. The recommended dose is 20 mmol h1, adjusted to achieve a plasma concentration of 2.54.0 mmol litre1. It is important to monitor plasma calcium concentrations during the administration of magnesium as it inhibits the release of parathyroid hormone.
Downloaded from http://ceaccp.oxfordjournals.org/ by guest on July 27, 2013
Control of muscle rigidity and spasms
Muscle spasms and rigidity are treated effectively by sedation. Many different drugs alone and in combination have been used to achieve this. Benzodiazepines are considered first line treatment; both diazepam and midazolam have been extensively used. Large doses (up to 100 mg h1) may be required. Morphine can be equally efficacious and is usually used as an adjunct to benzodiazepine sedation. Morphine has a central action which can minimize the effects of tetanospasmin. More recently, experience has been gained using remifentanil in tetanus. Although it is a pharmacologically attractive choice as a short-acting sedative and analgesic, its use is prohibitively expensive and associated with a number of undesirable side-effects. Propofol has also been used successfully; however, in order to achieve adequate plasma concentrations to relieve muscle rigidity, mechanical ventilation is necessary. Additional, useful sedation may be provided using anticonvulsants, in particular phenobarbital (which enhances GABA activity) and phenothiazines such as chlorpromazine. Other agents that have been used with success include dantrolene and intrathecal baclofen. Baclofen is a structural analogue of GABA. When given intrathecally, it diffuses into the spinal cord inhibiting neuronal transmission. Complete abolition of rigidity and spasms has been achieved in a limited number of cases using the intrathecal route. There is a significant risk of respiratory depression associated with its use. There have been only a few case reports which support the use of dantrolene. Disadvantages include potential hepatotoxity and cost. Muscle spasms refractory to benzodiazepines should be managed with neuromuscular blocking agents. There have been no comparative trials of neuromuscular blocking agents with tetanus and recommendations are again based on case reports. Atracurium is probably the neuromuscular blocking agent of choice. Vecuronium has also been used because of
Supportive treatment
Successful management of tetanus requires the entire armamentarium of the modern intensive care unit. A multidisciplinary approach is essential. Most cases require 46 weeks of supportive treatment. Poor nutrition and weight loss occur rapidly because of dysphagia, altered gastrointestinal function and increased metabolic rate. Enteral nutrition should be established as early as possible. Nosocomial infections are common because of the prolonged course of tetanus and remain an important cause of mortality. Prevention of respiratory complications involves meticulous mouth care, chest physiotherapy and tracheal suction. Adequate sedation during invasive procedures is mandatory to prevent provoking spasm or autonomic instability. Pulmonary embolism is a particular problem and thromboprophylaxis is
Continuing Education in Anaesthesia, Critical Care & Pain | Volume 6 Number 3 2006
103
Tetanus
essential. Rhabdomyolysis is a common finding after a prolonged tetanic spasm. This may lead to acute renal failure. Recovery from tetanus is slow but often complete. The psychological support needed following prolonged illness should not be forgotten.
3. Thwaites CL. Tetanus. Curr Anaesth Crit Care 2005; 16: 5057 4. Cook TM, Protheroe RT, Handel JM. Tetanus: a review of the literature. Br J Anaesth 2001; 87: 47787 5. Ablett JJL. Analysis and main experiences in 82 patients treated in the Leeds Tetanus Unit. In: Ellis M. ed. Symposium on tetanus in Great Britain. Boston Spa, UK: Leeds General Infirmary, 1967; 110 6. Ahmadsyah I, Salim A. Treatment of tetanus: an open study to compare the efficacy of procaine penicillin and metronidazole. Br Med J (Clin Res Ed) 1985; 291: 64850 7. Attygalle D, Rodrigo N. Magnesium as first line therapy in the management of tetanus: a prospective study of 40 patients. Anaesthesia 2002; 57: 81117
References
1. British National Formulary Number 49. British Medical Association and Royal Pharmaceutical Society of Great Britain: Pharmaceutical Press, 2005 2. Health Protection Agency. Ongoing national outbreak of tetanus in injecting drug users. Commun Dis Rep CDR Wkly [serial online] 2004; 14(a): news. Available at http://www.hpa.org.uk/cdr/ PDFfiles/2004/ cdr0904.pdf
Please see multiple choice questions 610.
Downloaded from http://ceaccp.oxfordjournals.org/ by guest on July 27, 2013
104
Continuing Education in Anaesthesia, Critical Care & Pain | Volume 6 Number 3 2006
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Case Report: Pulmonary Sequestration: A Case Report and Literature ReviewDocument4 pagesCase Report: Pulmonary Sequestration: A Case Report and Literature Reviewjo_jo_maniaNo ratings yet
- Canadian Contraception ConsensusDocument14 pagesCanadian Contraception Consensusjo_jo_maniaNo ratings yet
- Donordarah PDFDocument1 pageDonordarah PDFjo_jo_maniaNo ratings yet
- AnyelirDocument2 pagesAnyelirjo_jo_maniaNo ratings yet
- Structure Content: 1. EXERCISE 1 (Skill 1-2) 2. Toefl Review Exercise (Skill 1-2) 3. Answer KeysDocument3 pagesStructure Content: 1. EXERCISE 1 (Skill 1-2) 2. Toefl Review Exercise (Skill 1-2) 3. Answer Keysjo_jo_mania0% (1)
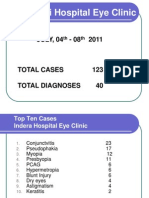
- NEW Weekly Indra 04-08 July 2011Document13 pagesNEW Weekly Indra 04-08 July 2011jo_jo_maniaNo ratings yet
- Donor DarahDocument1 pageDonor Darahjo_jo_maniaNo ratings yet
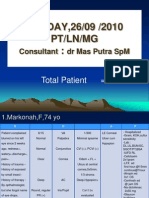
- Sunday, 26/09 /2010 PT/LN/MG:: Consultant DR Mas Putra SPMDocument6 pagesSunday, 26/09 /2010 PT/LN/MG:: Consultant DR Mas Putra SPMjo_jo_maniaNo ratings yet
- International Centre For Eye Health Teaching Set 2 The Eye in Primary Health CareDocument25 pagesInternational Centre For Eye Health Teaching Set 2 The Eye in Primary Health Carejo_jo_maniaNo ratings yet
- Migraine Prophylaxis: Pharmacotherapy PerspectivesDocument11 pagesMigraine Prophylaxis: Pharmacotherapy Perspectivesjo_jo_maniaNo ratings yet
- Laser Iridotomy and GlaucomaDocument2 pagesLaser Iridotomy and Glaucomajo_jo_maniaNo ratings yet
- Arterial Blood Gas: DR - Made Widia, Sp.A (K)Document19 pagesArterial Blood Gas: DR - Made Widia, Sp.A (K)jo_jo_mania100% (1)
- UveaDocument43 pagesUveajo_jo_mania100% (1)
- OrtoDocument61 pagesOrtojo_jo_maniaNo ratings yet
- Histamin Dan inDocument30 pagesHistamin Dan inNurul FadilaturrahmiNo ratings yet
- Dyslexia: Developmental Dyslexia Is ADocument5 pagesDyslexia: Developmental Dyslexia Is Ajo_jo_mania100% (1)
- An Endometrial Is A Procedure To Remove A Small Sample of The Lining of The UterusDocument2 pagesAn Endometrial Is A Procedure To Remove A Small Sample of The Lining of The Uterusjo_jo_maniaNo ratings yet
- X RaysDocument1 pageX Raysjo_jo_maniaNo ratings yet
- My CatatanDocument2 pagesMy CatatanDevyNo ratings yet
- Family Welfare Program 1.2Document4 pagesFamily Welfare Program 1.2amadieuNo ratings yet
- Neck LumpsDocument27 pagesNeck Lumpsfrabzi100% (1)
- CBT For CandA With OCD PDFDocument16 pagesCBT For CandA With OCD PDFRoxana AlexandruNo ratings yet
- Counseling For Gargle, Magic Mouth Wash & Mucositis in Cancer PTDocument3 pagesCounseling For Gargle, Magic Mouth Wash & Mucositis in Cancer PTAthirah BidinNo ratings yet
- Indications For Thyroid Surgeryexperience of The Ent Departmentof Moulay Ismail Military Hospital in Meknes (About 103 Cases)Document8 pagesIndications For Thyroid Surgeryexperience of The Ent Departmentof Moulay Ismail Military Hospital in Meknes (About 103 Cases)IJAR JOURNALNo ratings yet
- ABX Pentra Urinary Proteins CPDocument4 pagesABX Pentra Urinary Proteins CPSivaNo ratings yet
- Caesalpinia CristaDocument5 pagesCaesalpinia CristaDarmawan Said100% (1)
- Puberphonia 11Document19 pagesPuberphonia 11jaguar1979100% (2)
- APHNI Proceeding 2021Document9 pagesAPHNI Proceeding 2021Muhammad Faza ZhafranNo ratings yet
- Syngenta Proactive Fungicide Programme Guide BookDocument6 pagesSyngenta Proactive Fungicide Programme Guide BookTUXPAN LOCALIDADNo ratings yet
- Freeze Dried Superfoods 2004Document10 pagesFreeze Dried Superfoods 2004noragarcia76No ratings yet
- Occupational Health and HygieneDocument40 pagesOccupational Health and HygieneAISYAH NABILAH ROSLANNo ratings yet
- Dieta Baja en CarbohidratosDocument19 pagesDieta Baja en CarbohidratosESTUARDO ENRIQUE JO ORELLANANo ratings yet
- Lecture1 Introduction To Gene TherapyDocument42 pagesLecture1 Introduction To Gene TherapySandeep SinghNo ratings yet
- Introduction To Study of Pathophysiology: Prof. J. Hanacek, M.D., PH.D.Document30 pagesIntroduction To Study of Pathophysiology: Prof. J. Hanacek, M.D., PH.D.Margaret Marie CepilloNo ratings yet
- Retained PlacentaDocument3 pagesRetained PlacentaDeddy AngNo ratings yet
- Anxiety, Stress & Coping: An International JournalDocument10 pagesAnxiety, Stress & Coping: An International JournalPhany Ezail UdudecNo ratings yet
- Arnold Magazine 2020Document116 pagesArnold Magazine 2020Danieel GomesNo ratings yet
- Delivery Bot: End of Project DocumentationDocument45 pagesDelivery Bot: End of Project DocumentationAhmed Abd elmoneimNo ratings yet
- First AidDocument37 pagesFirst AidPearl Delay100% (1)
- 100 Puppy Mills ListDocument3 pages100 Puppy Mills Listapi-285462255No ratings yet
- Formatif Modul 6Document39 pagesFormatif Modul 6dwi anlesNo ratings yet
- PEC11 Chap 19 Seizures and SyncopeDocument55 pagesPEC11 Chap 19 Seizures and SyncopeRyanNo ratings yet
- Liver Function Trans CompressDocument17 pagesLiver Function Trans CompressJack KayatNo ratings yet
- AstringentsDocument23 pagesAstringentsBishal ChauhanNo ratings yet
- TizanidineDocument2 pagesTizanidinebhawanisrNo ratings yet
- Referat EticaDocument5 pagesReferat EticaCarp Petru-CosminNo ratings yet
- Biter Gourd GraftingDocument5 pagesBiter Gourd GraftingDr.Eswara Reddy Siddareddy100% (1)
- The Serpentine Mineral GroupDocument3 pagesThe Serpentine Mineral GroupWilly ApryantoNo ratings yet