Professional Documents
Culture Documents
How To Read A Chest X Ray
How To Read A Chest X Ray
Uploaded by
jcrajaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
How To Read A Chest X Ray
How To Read A Chest X Ray
Uploaded by
jcrajaCopyright:
Available Formats
SSMJ Vol 1 Issue 2. Downloaded from http://www.southernsudanmedicaljournal.
com
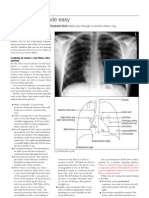
How to Read a Chest X-Ray A Step by Step Approach
Dr. Stephan Voigt
Consultant Radiologist
Isle of Wight NHS Primary Care Trust
St Marys Hospital Newport
Department of Diagnostic Imaging
Isle of Wight, UK
PO30 5TG
This article is an attempt to give the reader guidance how to read a chest X-ray and below are two
methods. There is no perfect way to read an x-ray. However, the important message I would like to
give is, to adopt one or the other approach, and to use the chosen approach consistently.
On all X-rays check the following:
Check patient details
o First name, surname, date of birth.
Check orientation, position and side description
o Left, right, erect, ap, pa, supine, prone
Check additional information
o inspiration, expiration
Check for rotation
o measure the distance from the medial end of each clavicle to the spinous process of
the vertebra at the same level, which should be equal
Check adequacy of inspiration
o Nine pairs of ribs should be seen posteriorly in order to consider a chest x-ray
adequate in terms of inspiration
Check penetration
o one should barely see the thoracic vertebrae behind the heart
Check exposure
o One needs to be able to identify both costophrenic angles and lung apices
Specific Radiological Checklist:
A - Airway
Ensure trachea is visible and in midline
o Trachea gets pushed away from abnormality, eg pleural effusion or tension
pneumothorax
o Trachea gets pulled towards abnormality, eg atelectasis
SSMJ Vol 1 Issue 2. Downloaded from http://www.southernsudanmedicaljournal.com
o Trachea normally narrows at the vocal cords
o View the carina, angle should be between 60 100 degrees
o Beware of things that may increase this angle, eg left atrial enlargement, lymph node
enlargement and left upper lobe atelectasis
o Follow out both main stem bronchi
o Check for tubes, pacemaker, wires, lines foreign bodies etc
o If an endotracheal tube is in place, check the positioning, the distal tip of the tube
should be 3-4cm above the carina
Check for a widened mediastinum
o Mass lesions (eg tumour, lymph nodes)
o Inflammation (eg mediastinitis, granulomatous inflammation)
o Trauma and dissection (eg haematoma, aneurysm of the major mediastinal vessels)
B Bones
Check for fractures, dislocation, subluxation, osteoblastic or osteolytic lesions in clavicles,
ribs, thoracic
Spine and humerus including osteoarthritic changes
At this time also check the soft tissues for subcutaneous air, foreign bodies and surgical clips
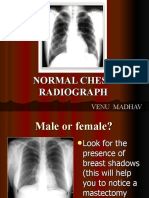
Caution with nipple shadows, which may mimic intrapulmonary nodules
o compare side to side, if on both sides the nodules in question are in the same
position, then they are likely to be due to nipple shadows
C - Cardiac
Check heart size and heart borders
o Appropriate or blunted
o Thin rim of air around the heart, think of pneumomediastinum
Check aorta
o Widening, tortuosity, calcification
Check heart valves
o Calcification, valve replacements
Check SVC, IVC, azygos vein
o Widening, tortuosity
SSMJ Vol 1 Issue 2. Downloaded from http://www.southernsudanmedicaljournal.com
D Diaphragm
Right hemidiaphragm
o Should be higher than the left
o If much higher, think of effusion, lobar collapse, diaphragmatic paralysis
o If you cannot see parts of the diaphragm, consider infiltrate or effusion
If film is taken in erect or upright position you may see free air under the diaphragm if intra-
abdominal perforation is present
E Effusion
Effusions
o Look for blunting of the costophrenic angle
o Identify the major fissures, if you can see them more obvious than usual, then this
could mean that fluid is tracking along the fissure
Check out the pleura
o Thickening, loculations, calcifications and pneumothorax
F Fields (Lungfields)
Check for infiltrates
o Identify the location of infiltrates by use of known radiological phenomena, eg loss of
heart borders or of the contour of the diaphragm
o Remember that right middle lobe abuts the heart, but the right lower lobe does not
o The lingula abuts the left side of the heart
Identify the pattern of infiltration
o Interstitial pattern (reticular) versus alveolar (patchy or nodular) pattern
o Lobar collapse
o Look for air bronchograms, tram tracking, nodules, Kerley B lines
o Pay attention to the apices
Check for granulomas, tumour and pneumothorax
G Gastric Air Bubble
Check correct position
Beware of hiatus hernia
Look for fee air
SSMJ Vol 1 Issue 2. Downloaded from http://www.southernsudanmedicaljournal.com
Look for bowel loops between diaphragm and liver
H Hilum
Check the position and size bilaterally
Enlarged lymph nodes
Calcified nodules
Mass lesions
Pulmonary arteries, if greater than 1.5cm think about possible causes of enlargement
Extended Radiological Check List Lateral Film
B Bones
Check the vertebral bodies and the sternum for fractures or other osteolytic changes
C Cardiac
Check for enlargement of the right ventricle and right atrium (retrosternal and retrocardiac
spaces)
Trace the aorta
D Diaphragm
Check for fluid tracking up, costophrenic blunting and the associated hemidiaphragm
E Effusions
Check to see the fissures here as well both major fissures and the horizontal may be found
in the lateral view
F Fields
SSMJ Vol 1 Issue 2. Downloaded from http://www.southernsudanmedicaljournal.com
Check the translucency of the thoracic vertebrae in the lateral view, when there is a sudden
change in transparency, then this is likely to be caused by infiltrate
Also try to find the infiltrate that you think you saw on the pa-film to verify existence and
anatomical location
Pay special attention to the lower lung lobes
I would like to close with a clarification of two important radiological findings, whose understanding is
very useful for a correct interpretation of chest x-ray findings.
The first is the silhouette sign, which can localise abnormalities on a pa-film without need for a
lateral view. The loss of clarity of a structure, such as the hemidiaphragm or heart border, suggests
that there is adjacent soft tissue shadowing, such as consolidated lung, even when the abnormality
itself is not clearly visualised. The reason is, that borders, outlines and edges seen on plain
radiographs depend on the presence of two adjacent areas of different density, Roughly speaking,
only four different densities are detectable on plain films; air, fat, soft tissue and calcium (five if you
include contrast such as barium). If two soft tissue densities lie adjacent, then they will not be visible
separately (eg the left and right ventricles). If, however, they are separated by air, the boundaries of
both will be seen.
The second important x-ray finding is the lung collapse. A collapse usually occurs due to proximal
occlusion of a bronchus, causing subsequently a loss of aeration. The remaining air is gradually
absorbed, and the lung loses volume. Proximal stenosing bronchogenic carcinoma, mucous plugging,
fluid retention in major airways, inhaled foreign body or malposition of an endotracheal tube are the
most common reasons for a lung collapse. Tracheal displacement or mediastinal shift towards the
side of the collapse is often seen. Further findings are elevation of the hemidiaphragm, reduced
vessel count on the side of the collapse or herniation of the opposite lung across the midline.
SSMJ Vol 1 Issue 2. Downloaded from http://www.southernsudanmedicaljournal.com
Figure 1: Left mid mediastinal / paraaortic tumour and left upper lobe satellite
lesion
SSMJ Vol 1 Issue 2. Downloaded from http://www.southernsudanmedicaljournal.com
Figure 2: Left basal pleural effusion and consolidation
SSMJ Vol 1 Issue 2. Downloaded from http://www.southernsudanmedicaljournal.com
Figure 3: Left upper lobe tumour
SSMJ Vol 1 Issue 2. Downloaded from http://www.southernsudanmedicaljournal.com
Figure 4: Right pleural metastases and pleural effusion due to carcinoma of
the ovary
SSMJ Vol 1 Issue 2. Downloaded from http://www.southernsudanmedicaljournal.com
Figure 5: Pleural calcifications and adhesions due to asbestos exposure
SSMJ Vol 1 Issue 2. Downloaded from http://www.southernsudanmedicaljournal.com
Figure 6: Pulmonary fibrosis and superimposed infection
SSMJ Vol 1 Issue 2. Downloaded from http://www.southernsudanmedicaljournal.com
Figure 7: Right middle lobe pneumonia
You might also like
- Pathophysiology For Breast CancerDocument2 pagesPathophysiology For Breast CancerKatrina Angeli Murillo100% (6)
- Body Reflex ZonesDocument161 pagesBody Reflex Zonesleonardo1monteiro-980% (5)
- Medical Genetics For The MRCOG and Beyond PDFDocument146 pagesMedical Genetics For The MRCOG and Beyond PDFs100% (3)
- Chest X-RayDocument101 pagesChest X-RayYuke04No ratings yet
- Lessonplan FinDocument14 pagesLessonplan Finx483xDNo ratings yet
- Hypnosis Personal Healing ScriptDocument10 pagesHypnosis Personal Healing Scriptmoumona100% (1)
- Rivanol EnglishDocument7 pagesRivanol EnglishAnnisa Nur JNo ratings yet
- How To Read X-RayDocument8 pagesHow To Read X-RayPeterson Wachira HscNo ratings yet
- ABC ChestDocument4 pagesABC ChestSintounNo ratings yet
- Chest X-Ray: Confirm DetailsDocument14 pagesChest X-Ray: Confirm DetailsNosheen HafeezNo ratings yet
- Interpreting The Chest Radio Graph Friendly)Document9 pagesInterpreting The Chest Radio Graph Friendly)Vagner BorgesNo ratings yet
- Chest X-Ray Interpretation A Structured Approach Radiology OSCEDocument1 pageChest X-Ray Interpretation A Structured Approach Radiology OSCEValentina SepúlvedaNo ratings yet
- Radiology NotesDocument34 pagesRadiology Notesliweiss100% (2)
- How To Read A Chest X-RayDocument3 pagesHow To Read A Chest X-RayKristina KostadinovskaNo ratings yet
- Thoracic Imaging Radiographic BasicsDocument130 pagesThoracic Imaging Radiographic BasicsIsak ShatikaNo ratings yet
- Chest X-Ray CXR InterpretationDocument13 pagesChest X-Ray CXR InterpretationduncanNo ratings yet
- Chest Xray PDFDocument8 pagesChest Xray PDFOvi SharmaNo ratings yet
- How To Read A Chest X RayDocument20 pagesHow To Read A Chest X RayJasvin Sidhu100% (1)
- How To Read A Chest X RayDocument11 pagesHow To Read A Chest X RayHilmia Fahma100% (2)
- Radiological Investigation of Chest. The Radiological Semiotics of The Chest PathologyDocument169 pagesRadiological Investigation of Chest. The Radiological Semiotics of The Chest PathologyВладимир КурпаянидиNo ratings yet
- Reading A Chest X-RayDocument2 pagesReading A Chest X-RaySabrinaAyuPutriNo ratings yet
- XrayDocument28 pagesXrayPravinNo ratings yet
- DX Imaging 1 MT and FinalDocument24 pagesDX Imaging 1 MT and FinalRaymondNo ratings yet
- How To Read Chest X-RayDocument4 pagesHow To Read Chest X-RaydrrajkumarsoniNo ratings yet
- 150 Interpretation of The Chest Radiograph - Part 2Document12 pages150 Interpretation of The Chest Radiograph - Part 2bandarascbNo ratings yet
- CXR Interpretation WriteupDocument32 pagesCXR Interpretation WriteupArhanNo ratings yet
- PICTURES All in This PDFDocument597 pagesPICTURES All in This PDFHai Sheikh100% (1)
- CHEST X-RAY Presentation CVSDocument45 pagesCHEST X-RAY Presentation CVSNorsafrini Rita Ahmad100% (1)
- X RayDocument18 pagesX RayAbdul Ghaffar AbdullahNo ratings yet
- Topic 20. X-RayDocument4 pagesTopic 20. X-RayMadeline WanhartNo ratings yet
- Chest X Ray - BasicsDocument4 pagesChest X Ray - BasicsEd ChangNo ratings yet
- CXR Pnemonic ABCDEFGHIDocument2 pagesCXR Pnemonic ABCDEFGHIAngela PuspitaNo ratings yet
- Chest X-Ray Interpretation: Bucky Boaz, ARNP-CDocument101 pagesChest X-Ray Interpretation: Bucky Boaz, ARNP-CAnna DiaconuNo ratings yet
- Pemeriksaan Radiologi Pada Sistem Respirasi01Document115 pagesPemeriksaan Radiologi Pada Sistem Respirasi01Rendy NunuhituNo ratings yet
- 2 1 Diseases of The Respiratory System Radiological Pathology DRDocument43 pages2 1 Diseases of The Respiratory System Radiological Pathology DRNatnael GetahunNo ratings yet
- DifdgDocument54 pagesDifdgMarina Ivosevic MilosavljevicNo ratings yet
- Cara Baca Foto ThoraxDocument23 pagesCara Baca Foto ThoraxNofilia Citra CandraNo ratings yet
- Diagnostic Imaging - 8 - Radiological Pathology - Lung Pathologies and Radiology in Specific Cases - Prof - Dr.i̇smet TAMERDocument35 pagesDiagnostic Imaging - 8 - Radiological Pathology - Lung Pathologies and Radiology in Specific Cases - Prof - Dr.i̇smet TAMERAly MssreNo ratings yet
- Chest X Rays Made EasyDocument3 pagesChest X Rays Made EasyHaluk AlibazogluNo ratings yet
- CXR InterpretationDocument3 pagesCXR InterpretationNairobipaeds Madakitari WatotoNo ratings yet
- Echo Heart4advancedDocument21 pagesEcho Heart4advanceddgina8800No ratings yet
- RADIOLOGICAL SIGNS ChestDocument73 pagesRADIOLOGICAL SIGNS Chestdoctor evanNo ratings yet
- Cara Membaca Foto Thoraks Yang BaikDocument2 pagesCara Membaca Foto Thoraks Yang BaikIdi Nagan RayaNo ratings yet
- (RADIO 250) LEC 06 Chest RadiologyDocument10 pages(RADIO 250) LEC 06 Chest Radiologyjmhinos4833No ratings yet
- Interpretation Chest X RayDocument127 pagesInterpretation Chest X RayVimal NishadNo ratings yet
- Radiology AssignmentDocument27 pagesRadiology AssignmentRoyce GonzagaNo ratings yet
- Chest InjuryDocument6 pagesChest InjuryRolando Reyna100% (1)
- How To Interpret CXRs For OSCEsDocument2 pagesHow To Interpret CXRs For OSCEsPrarthana Thiagarajan100% (9)
- Chest Xrays Made EasyDocument5 pagesChest Xrays Made Easyrouan.tan9275No ratings yet
- MDS 1005 Dissections 1-3 - 2015Document6 pagesMDS 1005 Dissections 1-3 - 2015Brooke Lynn FalzonNo ratings yet
- Fallot Tetralogy Imaging Findings With MDCT, Pre and Postoperative FindingsDocument25 pagesFallot Tetralogy Imaging Findings With MDCT, Pre and Postoperative FindingsMusaddad MudjahidNo ratings yet
- Normal Chest RadiographDocument108 pagesNormal Chest RadiographVenu Madhav100% (1)
- CXR Made Easy PDFDocument14 pagesCXR Made Easy PDFyourdirtysocksNo ratings yet
- Interpretasi Foto DadaDocument137 pagesInterpretasi Foto DadaRofi Irman100% (1)
- II.8. Infective EndocarditisDocument24 pagesII.8. Infective Endocarditisbcarmen.alexandraNo ratings yet
- Chest X-Ray Analysis 2023Document63 pagesChest X-Ray Analysis 2023CHARLOTTE DU PREEZNo ratings yet
- Ultrasound of The Thorax (Noncardiac)Document13 pagesUltrasound of The Thorax (Noncardiac)ludiegues752No ratings yet
- Radiologi PPDSDocument49 pagesRadiologi PPDSFadli Amali100% (1)
- Chest Xray BasicsDocument47 pagesChest Xray BasicsPartha GanesanNo ratings yet
- How To Read A Chest X-Ray film-SWUSMDocument24 pagesHow To Read A Chest X-Ray film-SWUSMEarl Mel Dustin LaoNo ratings yet
- Anatomical Atlas of Chinese Acupuncture Points: The Cooperative Group of Shandong Medical College and Shandong College of Traditional Chinese MedicineFrom EverandAnatomical Atlas of Chinese Acupuncture Points: The Cooperative Group of Shandong Medical College and Shandong College of Traditional Chinese MedicineRating: 4.5 out of 5 stars4.5/5 (8)
- Difficult Acute Cholecystitis: Treatment and Technical IssuesFrom EverandDifficult Acute Cholecystitis: Treatment and Technical IssuesNo ratings yet
- Bavetsias Et Al-2015-Frontiers in OncologyDocument10 pagesBavetsias Et Al-2015-Frontiers in OncologyJubairNo ratings yet
- Anp Presentation On GeriatricsDocument114 pagesAnp Presentation On Geriatricsgeetanjali behl100% (3)
- Askep Klien DG CholelithiasisDocument13 pagesAskep Klien DG CholelithiasisAmanda Mahendra SastranegaraNo ratings yet
- Usana Product InfoDocument1 pageUsana Product InfoMike AlertaNo ratings yet
- Cancer de PancreasDocument12 pagesCancer de PancreasRuben RoaNo ratings yet
- SORL BookDocument21 pagesSORL Booksyed imdadNo ratings yet
- Research Article: Management of Amavata (Rheumatoid Arthritis) by Application of Ayurvedic PrincipleDocument6 pagesResearch Article: Management of Amavata (Rheumatoid Arthritis) by Application of Ayurvedic PrinciplerajrajNo ratings yet
- Whole Body Checkup (Men Women) - Medanta-The Medicity - Medanta HealthcheckupDocument1 pageWhole Body Checkup (Men Women) - Medanta-The Medicity - Medanta HealthcheckupShubu ParajuliNo ratings yet
- Medbak Insert KitDocument2 pagesMedbak Insert Kitjohnnyboy30003223No ratings yet
- PLANETS INTERCEPTED - Lynn Koiner - Astrological ResearchDocument3 pagesPLANETS INTERCEPTED - Lynn Koiner - Astrological ResearchaiavenueNo ratings yet
- Colon: Colorectal Cancer, Also Called Colon Cancer or Large Bowel Cancer, IncludesDocument6 pagesColon: Colorectal Cancer, Also Called Colon Cancer or Large Bowel Cancer, IncludesMhackie Perez100% (1)
- Tuberculosis Associated Chronic Obstructive Pulmonary DiseaseDocument12 pagesTuberculosis Associated Chronic Obstructive Pulmonary DiseaseinetNo ratings yet
- Silica Sand MSDSDocument8 pagesSilica Sand MSDSizzybjNo ratings yet
- Evaluation of Efficacy and Tolerability of Acetaminophen Paracetamol and Mefenamic Acid As Antipyretic in Pediatric Pati PDFDocument7 pagesEvaluation of Efficacy and Tolerability of Acetaminophen Paracetamol and Mefenamic Acid As Antipyretic in Pediatric Pati PDFrasdiantiNo ratings yet
- Theraex For IKFRDocument130 pagesTheraex For IKFRsingle_ladyNo ratings yet
- BMI ClassificationDocument10 pagesBMI ClassificationFeyNo ratings yet
- 2019-01-01 Men S HealthDocument118 pages2019-01-01 Men S HealthMauroNo ratings yet
- Efectele Pe Termen Lung Ale Alaptatului OMSDocument74 pagesEfectele Pe Termen Lung Ale Alaptatului OMSbobocraiNo ratings yet
- ICMM Health and Safety Performance Indicator DefinitionsDocument34 pagesICMM Health and Safety Performance Indicator DefinitionsStakeholders360No ratings yet
- Praktikum 1 Patologi ThoraxDocument61 pagesPraktikum 1 Patologi ThoraxFarizky DwitiaNo ratings yet
- Pyrogel XT - MsdsDocument7 pagesPyrogel XT - MsdsBob KmnNo ratings yet
- Common Bile Duct Cyst: About An Observation and Review of The LiteratureDocument3 pagesCommon Bile Duct Cyst: About An Observation and Review of The LiteratureasclepiuspdfsNo ratings yet
- Wyneken The Anatomy of Sea Turtle PDFDocument14 pagesWyneken The Anatomy of Sea Turtle PDFElis PerroneNo ratings yet
- Post Test 02Document3 pagesPost Test 02Evangeline Olarte QuilantangNo ratings yet
- Reni-Infectious Disease 100 SoalDocument61 pagesReni-Infectious Disease 100 SoalNur akilaNo ratings yet