Professional Documents
Culture Documents
1.prevention and Treatment of Surgical Infection (DR TJ)
1.prevention and Treatment of Surgical Infection (DR TJ)
Uploaded by
iisscribdOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1.prevention and Treatment of Surgical Infection (DR TJ)
1.prevention and Treatment of Surgical Infection (DR TJ)
Uploaded by
iisscribdCopyright:
Available Formats
PREVENTION AND TREATMENT
of SURGICAL INFECTION
INTRODUCTION
The risk factors for developing a
wound infection
The preoperative (prehospital) component
The operative environment
The microbial factors
CLASSIFICATION OF SURGICAL WOUNDS
CLASSIFICATION OF SURGICAL WOUNDS
Classification of Operative Wounds
and Surgical infection rates
Health care-associated infection (HAI) /
Nosocomial Infections in Surgical Patients
Potential sites:
UTIs
Pneumonia
surgical site (wound) infections (SSIs)
bloodstream infection bacteremia
Principles Of Prevention To Infection
Preoperative Shower
Remote-Site Infection and Shaving
Hand Washing
Shoe Covers, Caps, Masks, Gowns, and Gloves
Core Body Temperature
Postoperative Care
Surgical Wound Management and Surgical
Wound Infection Care
Remote-Site Infection and Shaving
The presence of a remote-site infection,
whether it is a pustule, an upper respiratory
infection, or urinary tract infection, needs to be
identified and treated prior to any surgical
intervention
A patient whose surgical site has been shaved
has an infection rate two to three times higher
than patients who are not shaved
The need for shaving a surgical site should be
considered not for sanitary reasons but only for
the convenience of the patients wound care.
Hand Washing
Shoe Covers, Caps, Masks, Gowns,
and Gloves
Core Body Temperature
The presence of the cold environment in the
operating room reduces the patients core body
temperature
This reduction in the patients core temperature
significantly increases the risk of postoperative
infection
This requires meticulous attention to keeping the
patient warm
Postoperative Care
Supportive therapy
Monitoring Postoperative Fever
Blood and radiographic tests
Surgical Wound Management
Surgical Wound Management and
Surgical Wound Infection Care
Topical Wound Treatment
CLOSED WOUNDS
OPEN WOUNDS
Closed wound
Healing by primary intention
Closed wounds should be kept sterile for 24-48 h until
epithelialization is complete
Tensile strength is only 200/0 of normal skin at 3 weeks
when collagen cross-linking is becoming significant. At 6
weeks, wounds are at 70% of the tensile strength of normal
skin, which is nearly the maximal tensile strength achieved
by scar (75%-80% of normal).
Open Wound
Necrotic material should be removed
Open wounds heal optimally in a moist, sterile environment
The wound is open, and the edges are not approximated
The suture closed as delayed primary closure after 25 days
These wounds heal by contraction and epithelialization.
Secondary closure of wound
The wound is open, and the edges are not approximated. A
potentially contaminated wound is best left open lightly packed
with damp saline soaked gauze and the suture closed as delayed
primary closure after 25 days
MICROBIAL FACTORS OF IMPORTANCE IN
THE DEVELOPMENT OF INFECTION
Two major reservoirs:
(1) host endogenous microflora
(2) microbes within the external milieu, which
often represents the nosocomial
environment for hospitalized individuals
ANTIBIOTICS IN SURGERY
Prophylactic antibiotics
Antibiotic Therapy
Prophylactic antibiotics
Empirical cover against expected pathogens with local
hospital guidelines
Single-shot intravenous administration at induction of
anaesthesia
Repeat only in prosthetic surgery, long operations or if
there is excessive blood loss
Continue as therapy if there is unexpected
contamination
Patients with heart valve disease or a prosthesis should
be protected from bacteraemia caused by dental work,
urethral instrumentation or visceral surgery
Prophylactic antibiotics
Medical considerations that compromise the
healing capacity or increase the infection risk:
Diabetes
Peripheral vascular disease
Possibility of gangrene or tetanus
Immunocompromise
Prophylactic antibiotics
High-risk wounds or situations:
Penetrating wounds
Abdominal trauma
Compound fractures
Wounds with devitalized tissue
Lacerations greater than 5 cm or stellate lacerations
Contaminated wounds
High risk anatomical sites such as hand or foot
Biliary and bowel surgery.
Antibiotic Therapy
A narrow-spectrum antibiotic may be used to
treat a known sensitive infection
Combinations of broad-spectrum antibiotics
can be used when the organism is not known
Principles for the use of antibiotic
therapy
Antibiotics do not replace surgical drainage of
infection
Only spreading infection or signs of systemic
infection justifies the use of antibiotics
Whenever possible, the organism and sensitivity
should be Determined
Treatment of commensals that have become
opportunist pathogens
They are likely to have multiple antibiotic resistance
It may be necessary to rotate antibiotics
HIV, AIDS AND THE SURGEON
Involvement of surgeons with HIV patients
(universal precautions):
use of a full face mask ideally, or protective spectacles;
use of fully waterproof, disposable gowns and drapes,
particularly during seroconversion;
boots to be worn, not clogs, to avoid injury from dropped
sharps;
double gloving needed
allow only essential personnel in theatre;
avoid unnecessary movement in theatre;
respect is required for sharps, with passage in a kidney dish;
a slow meticulous operative technique is needed with
minimised bleeding.
Thank You
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Closure of Minor Skin Wounds With Sutures - UpToDate2019 PDFDocument32 pagesClosure of Minor Skin Wounds With Sutures - UpToDate2019 PDFGerii Pucllas VillarNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document7 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)hendra2darmawanNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document26 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)hendra2darmawan0% (1)
- Surgical Infection, SIRS and SepsisDocument27 pagesSurgical Infection, SIRS and Sepsishendra2darmawan100% (3)
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document10 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)hendra2darmawanNo ratings yet
- Antipsychotic Drugs: Setyawati S KaryonoDocument28 pagesAntipsychotic Drugs: Setyawati S Karyonohendra2darmawanNo ratings yet
- Modul Hormon Reproduksi Dan Kontrasepsi WanitaDocument46 pagesModul Hormon Reproduksi Dan Kontrasepsi Wanitahendra2darmawanNo ratings yet
- Introduction To Laboratory Medicine (Clinical Laboratory) : Dr. Dr. Tinny Rasjad SPPK (K)Document43 pagesIntroduction To Laboratory Medicine (Clinical Laboratory) : Dr. Dr. Tinny Rasjad SPPK (K)hendra2darmawanNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document24 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)hendra2darmawanNo ratings yet
- Transplantation ImmunologyDocument18 pagesTransplantation Immunologyhendra2darmawanNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document25 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)hendra2darmawanNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document28 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)hendra2darmawanNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document21 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)hendra2darmawanNo ratings yet
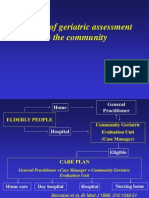
- The Use of Geriatric Assessment in The CommunityDocument16 pagesThe Use of Geriatric Assessment in The Communityhendra2darmawanNo ratings yet
- Disorder of PubertyDocument18 pagesDisorder of Pubertyhendra2darmawanNo ratings yet
- The Roles of Demography - Epidemiology - Statistics in COMDXDocument15 pagesThe Roles of Demography - Epidemiology - Statistics in COMDXhendra2darmawanNo ratings yet
- EpidemiologyDocument36 pagesEpidemiologyhendra2darmawan50% (2)
- Of Growth and Development IiDocument14 pagesOf Growth and Development Iihendra2darmawanNo ratings yet
- Pilot Laser BrochureDocument4 pagesPilot Laser BrochureCAO Group, Inc.No ratings yet
- Types of WoundsDocument40 pagesTypes of WoundsMwanja MosesNo ratings yet
- Skin DisordersDocument202 pagesSkin DisordersMj Briones100% (1)
- Research Articles ListDocument135 pagesResearch Articles Listnaga chaitanyaNo ratings yet
- People v. Buling YAPDocument2 pagesPeople v. Buling YAPDianne SantiagoNo ratings yet
- Chapter 28 Wound CareDocument26 pagesChapter 28 Wound CarePaijoNo ratings yet
- 7 BurnDocument29 pages7 BurnAlem AyahuNo ratings yet
- Emergency Report: July 26 - July 27 2016Document40 pagesEmergency Report: July 26 - July 27 2016Theresia Alfionita SinulinggaNo ratings yet
- GR 134362 People V Emelito Tayag Addict Not AggravatingDocument10 pagesGR 134362 People V Emelito Tayag Addict Not AggravatingdskymaximusNo ratings yet
- PRP in DermatologyDocument36 pagesPRP in DermatologySuryakant HayatnagarkarNo ratings yet
- Case Report Management Ankyloglossia With Scalpel ElectrosurgeryDocument3 pagesCase Report Management Ankyloglossia With Scalpel ElectrosurgeryDeasireeNo ratings yet
- HAAD ExamDocument5 pagesHAAD ExamFaith Levi Alecha AlferezNo ratings yet
- Nurs1000 Case Study Dhyani SakhiyaDocument8 pagesNurs1000 Case Study Dhyani SakhiyaKENNEDYNo ratings yet
- Management of Patients With Burn Injury WEBDocument28 pagesManagement of Patients With Burn Injury WEBJen Chua100% (2)
- IWGDF Guideline On The Classification of Diabetic Foot UlcersDocument15 pagesIWGDF Guideline On The Classification of Diabetic Foot Ulcersdr. Ellen FernandaNo ratings yet
- CapstoneDocument13 pagesCapstoneapi-401251868No ratings yet
- Diaper Industry in Next 25 YearsDocument58 pagesDiaper Industry in Next 25 Yearsjothi vel muruganNo ratings yet
- Wound Healing Activity of Withania LeafDocument8 pagesWound Healing Activity of Withania Leafyasir aliNo ratings yet
- Burn Patient Management Guidelines PDFDocument41 pagesBurn Patient Management Guidelines PDFIndah Kurnia100% (4)
- 2 4 1-BurnsDocument11 pages2 4 1-BurnsMicaNo ratings yet
- (123doc) Ophthalmic Microsurgical Suturing Techniques Part 2Document15 pages(123doc) Ophthalmic Microsurgical Suturing Techniques Part 2TEODORA MIHAELA PELEASANo ratings yet
- Wounds & Wound HealingDocument47 pagesWounds & Wound HealingDrSarmad100% (3)
- Manual Nudos Ethicon PDFDocument52 pagesManual Nudos Ethicon PDFMaria Paula CamposNo ratings yet
- BitesDocument18 pagesBitesPriya SharmaNo ratings yet
- Injectable Bone Graft and Allograft Bone Chips in The Treatment of Benign Bone LesionDocument8 pagesInjectable Bone Graft and Allograft Bone Chips in The Treatment of Benign Bone LesionIJAR JOURNALNo ratings yet
- Week 011-Module School Emergency ResourcesDocument5 pagesWeek 011-Module School Emergency ResourcesRica Mae LopezNo ratings yet
- Patients' Knowledge of Diabetes Complications and S Elf-Management Practices in GhanaDocument18 pagesPatients' Knowledge of Diabetes Complications and S Elf-Management Practices in GhanaNurul pattyNo ratings yet
- In Re Briggs A WLS Employee 12-22560Document107 pagesIn Re Briggs A WLS Employee 12-22560NevadaGadflyNo ratings yet
- LMMJ - Midterms 1.1 - Medico-Legal Aspects of Physical Injuries I TransDocument6 pagesLMMJ - Midterms 1.1 - Medico-Legal Aspects of Physical Injuries I Transchocoholic potchiNo ratings yet