Professional Documents
Culture Documents
Jurnal Striktur Ncbi
Jurnal Striktur Ncbi
Uploaded by
Rangga Ro'ufa Amri0 ratings0% found this document useful (0 votes)
8 views5 pagesjurnal
Original Title
jurnal striktur ncbi
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentjurnal
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
8 views5 pagesJurnal Striktur Ncbi
Jurnal Striktur Ncbi
Uploaded by
Rangga Ro'ufa Amrijurnal
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
REVIEW
Management of urethral strictures
A R Mundy
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Postgrad Med J 2006;82:489493. doi: 10.1136/pgmj.2005.042945
Controlled clinical trials are unusual in surgery, rare in
urology, and almost non-existent as far as the management
of urethral stricture is concerned. What data there are
come largely from so called expert opinion and the
quality of this is variable. None the less, the number of so
called experts, past and present, is comparatively small
and in broad principle their views more or less coincide.
Although this review is therefore inevitably biased, it is
unlikely that expert opinion will take issue with most of the
general points raised here.
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . .
Correspondence to:
Professor A R Mundy, The
Institute of Urology,
London, 2A Maple House,
Ground Floor, Rosenheim
Wing, 25 Grafton Way,
London WC1E 6AU, UK;
kelly.higgs@uclh.nhs.uk
Submitted
1 November 2005
Accepted 9 February 2006
. . . . . . . . . . . . . . . . . . . . . . .
U
rethral strictures have always been com-
mon. We know something about how the
ancient Egyptians treated stricture disease
4000 years ago and other civilisations since and
indeed not much has changed until about 50
years ago.
Urethral strictures are still common now.
Hospital Episode Statistics in the UK and similar
data from the USA suggest that men are affected
with an increasing incidence from about 1 in
every 10 000 men aged 25 to about 1 in every
1000 men ages 65 or more. Traditionally,
strictures in the past were caused by gonococcal
urethritis. These days this is rare in the developed
world although still common in some societies.
In the UK, aetiology is almost equally divided
between inflammation, trauma, and idio-
pathic. The inflammation category includes
non-specific urethritis and, increasingly com-
monly, lichen sclerosus, formerly known as
balanitis xerotica obliterans (BXO). Trauma is
more usually iatrogenic and attributable to
instrumentation these days but also includes
the more dramatic fall astride injuries to the
bulbar urethra and pelvic fracture related injuries
to the membranous urethra and bulbo-membra-
nous junction. Many idiopathic strictures are
idiopathic because their cause is lost in the
mists of time but many of these occur at the
junction of the proximal and middle sections of
the bulbar urethra in adolescents and young
adults with no previous history and many believe
this represents a congenital anomaly. Among the
established congenital anomalies of the lower
urogenital tract, hypospadias is one of the more
common and although this is not itself asso-
ciated with stricture, a stricture is an occasional
consequence of hypospadias surgery in early
childhood and an increasingly common cause
of strictures in the trauma category.
The pathology of urethral stricture disease is
poorly understood. External trauma generally
causes partial or complete disruption of an
otherwise normal urethrathat is clear. How a
stricture develops in other circumstances
remains unclear but it would seem that for
whatever reason a scar develops as a conse-
quence of changes in the structure and function
of the urethral epithelium and the sub-epithelial
spongy tissue causing a fibrotic narrowing of the
urethra.
1
Secondary changes in the epithelium
more proximally develop there afterwards caus-
ing a progressive stricturing of an increasing
length of the urethra from before backwards.
Longstanding urethral obstruction may cause
secondary complications in the rest of the
urinary tract.
2
CLI NI CAL ASSESSMENT AND
I NVESTI GATI ON
Trauma aside, most patients present with slow
and progressive deterioration of the urinary
stream leading to a feeling of incomplete empty-
ing as obstruction progressively develops. More
severe cases may be complicated by haematuria
or recurrent urinary infection and its sequalae.
It is usual practice for patients with lower
urinary tract symptoms to have their urinary
flow rate measured as part of initial investiga-
tion. In those who have a urethral stricture the
peak flow rate is typically low but the flow
pattern is characteristically flat (fig 1). This flow
pattern is almost pathognomonic of a urethral
stricture; certainly it should lead to a urethro-
gram as the next step in investigation. If properly
performed, this will show the exact site and
length of the stricture and most of its potential
complications (fig 2). Ultrasound evaluation may
show a thickening of the bladder wall associated
with longstanding outflow obstruction, and a
presence of residual urine. If these two signs are
present, an ultrasound scan of the kidneys
should be the next step to look for signs of
obstructive uropathy and in the presence of
hydroureteronephrosis, there should be an esti-
mate of renal function.
TREATMENT
The normal urinary flow rate in young and
middle aged men is generally greater than 15 ml/
second and the flow pattern a bell shaped curve.
Patients with an established diagnosis of ure-
thral stricture but who have a flow rate greater
than 10 ml/second and normal bladder thick-
ness, complete bladder emptying and who are
untroubled by recurrent urinary infection do not
necessarily require any treatment but they
should be kept under review. A flow rate less
than 10 ml/second is more commonly associated
with symptoms and with the secondary effects
such as recurrent haematuria or recurrent
urinary tract infection and with features of overt
489
www.postgradmedj.com
bladder obstruction on ultrasonography, but this is not
necessarily so. If the stricture is troublesome it should be
treated; if not the patient should be kept under review. With
a flow rate of less than 5 ml/second, abnormalities such as
those listed above are much more likely and the patient is
potentially at risk of acute retention, although this is a lot less
common than one would expect from the severity of the
narrowing of the urethra that is seen in such a situation. In
these patients treatment is advisable even if symptoms of
voiding difficulty are not troublesome.
The time honoured method of treatment is urethral
dilatationthe passage of calibrated instrumentsusually
made of metal and called sounds, Bougies or, more simply,
urethral dilators. They are generally straight through most of
their length with a hockey stick curve at the end and are
calibrated according to the French system, which relates the
size of the urethral dilator to the urethral circumference in
millimetres. The normal urethral calibre is 2426F (French)
at the external urinary meatus, a little wider in the penile
urethra, wider still in the bulbar urethra (about 36F), and
then narrower again in the posterior urethra, above the level
of the perineal membrane.
Some patients with urethral stricture have the diagnosis
made on endoscopic evaluation of the lower urinary tract.
The principle of urethral dilatation is to stretch the urethral
stricture up or otherwise, and more commonly, to disrupt it.
A graduated series of dilators from smaller to larger size is
passed to restore the urethral calibre to normal, or there-
abouts. The alternative form of instrumentation, also with a
history measured in thousands of years, is urethrotomy.
Initially, this was performed blindly by increasingly sophis-
ticated means until visual internal urethrotomy was devel-
oped about 35 years ago. Visual control of the process might
be expected to give better results but in fact, there is no
evidence that this is so. As a general rule however urethral
dilatation might best be reserved for more straightforward
strictures that can be dilated in an office setting using topical
anaesthesia whereas visual internal urethrotomy is probably
better for more complicated strictures, performed in a day
case operating theatre under regional or general anaesthesia.
Both procedures are generally regarded as simple and
straightforward but in fact carry a significant risk of
complications.
3
It is now generally accepted that urethrotomy and
dilatation are equally effective and can be expected to cure
about 50% of short bulbar urethral strictures when first used.
If the procedure has to be repeated, it is rarely curative and it
is rarely curative even the first time in strictures other than in
the bulbar urethra.
46
When the stricture recurs, it usually does so within weeks
or months and almost always within two years. Those that
recur comparatively infrequently might be palliated (rather
than cured) by repeat instrumentation and, as long as this is
agreeable to the patient and is uncomplicated by bleeding or
sepsis,
3
such palliation might be perfectly acceptable. If
instrumentation is required more frequently or is complicated
or unacceptable to the patient in the long term, then
urethroplasty is the only curative option.
Alternatives have been recommended, such as the use of a
laser rather than a cold knife for internal urethrotomy; an
indwelling urethral stent to hold the urethra open; or much
more commonly, the use of clean intermittent self catheter-
isation.
7
None of these, however, are curative; the laser is
expensive as well as ineffective; stents, although popular a
decade ago, commonly do more harm than good
810
; and only
self catheterisation is occasionally helpful: for the patient
who is not fit for, or is otherwise unwilling to undergo, a
urethroplasty.
GENERAL PRI NCI PLES OF URETHROPLASTY
1113
Ideally, one would like to excise a urethral stricture and join
the two healthy ends of urethra on either side together again
to restore continuity and calibre. Unfortunately, this can only
be done with short urethral strictures because of limitations
of elasticity and length before erectile function is compro-
mised. Excision and end to end anastomosis, or an
anastomotic urethroplasty as it is more commonly called, is
however best, even if it can only be used for short strictures of
the bulbar urethra and more proximally, in the membranous
urethra, because it gives the best and most sustained results
in terms of both a low re-stricture rate and a low
complication rate. Whether this high success rate is
50
40
30
20
10
0
0 05 10 15 20 25 30 35 40 45 50 55
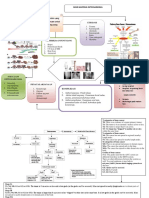
Figure 1 Flow pattern of a patient with
a urethral stricture.
A B
Figure 2 An uncomplicated (A) and a
somewhat more complicated stricture
(B).
490 Mundy
www.postgradmedj.com
attributable to the technique itself or because those strictures
that are amenable to an anastomotic urethroplasty generally
occur in younger patients with a more localised urethral
problem (such as trauma) is not clear.
When a stricture is too long for anastomotic urethroplasty
the alternative is some form of substitution urethroplasty.
Here, there are two alternative approaches. The first is to
excise the urethral stricture and perform a circumferential
repair of the urethra. Intuitively, this would seem to be a
sensible approach but in practice, a circumferential repair
needs to be staged to give satisfactory results or, if performed
in one stage, tends to give less satisfactory results than the
alternative approach of incising the stricture and then putting
on a patch to restore urethral calibre at that point
(stricturotomy and patch).
ANASTOMOTI C URETHROPLASTY
Anastomotic urethroplasty is generally only applicable in two
situations. Firstly, for short strictures of the bulbar urethra,
no more than 12 cm long, which are generally attributable
to external trauma or are otherwise idiopathic in origin
(possibly congenital). The external trauma is usually a fall
astride injury. The second situation is a pelvic fracture related
injury of the membranous urethra or bulbo-membranous
junction.
The general principles here are to mobilise the bulbar
urethra fully, capitalising on its elasticity to overcome any
defect in length as a result of excision of a short stricture or to
bridge a gap caused by complete disruption because of
external trauma. Should the elasticity of the urethra and
mobilisation alone be insufficient to bridge any defect then
the second general principle is to straighten out the natural
curve of the bulbar urethra by a sequential series of
manoeuvres including separation of the crura at the base of
the penis, wedge pubectomy of the inferior pubic arch, and, if
necessary, re-routing of the urethra around the shaft of the
shaft of the penis until the course of the bulbar urethra from
the penoscrotal junction to the apex of the prostate is a
straight line rather than the semi-circle that it normally is
(fig 3).
1416
SUBSTI TUTI ON URETHROPLASTY
Unlike anastomotic urethroplasty this can be used anywhere
in the urethra. When an anastomotic repair is possible and
appropriate this should be used in preference because it gives
better and more durable results. Substitution urethroplasty
should not therefore be used universally; it should be used
selectively for those strictures of the bulbar urethra that are
too long for an anastomnotic repair and all strictures of the
penile urethra in which an anastomotic repair would cause
unacceptable penile deformity on erection.
As a stricturotomy and patch is generally more successful
than an excision and circumferential repair then this is the
procedure of choice unless a urethral segment positively
needs to be excised as after previous surgery for hypospadias
when the urethra is irretrievably scarred, in lichen sclerosus
when it is irretrievably fibrotic, or in rare situations such as
with urethral arteriovenous malformations or tumours.
17
WHAT SORT OF A PATCH SHOULD BE USED?
It might seem intuitive that a skin flap, which brings with it
its own blood supply, would give better results than a free
graft, which has to develop its own blood supply having been
raised from a remote site. This is not however the case in
most circumstances.
18 19
Indeed, for most strictures the
results are just as good with a graft as with a flap as long
as the graft is a thin, full thickness graft with a dense sub-
dermal plexus such as full thickness graft of penile shaft skin
or foreskin, a post-auricular (from behind the ear) full
thickness graft, or a buccal mucosal graft (from inside of the
cheek). Buccal mucosa is currently the preferred graft
material, if only because it has the least donor site
morbidity.
2022
Occasionally a flap must be used when the local conditions
are not favourable for a graft as when there is extensive
scarring from previous surgery or active infection or previous
radiotherapy or when the stricture is unusually long or trans-
sphincteric. In such cases a flap of local genital skin pedicled
on the dartos layer of the penis (which is highly vascular) is
preferred.
23 24
When a segment of urethra has to be excised, usually
because of dense scarring in the penile urethra for whatever
reason, then a circumferential repair must be performed. It is
possible to do this in one stage, particularly for short
strictures in the most distal part of the penile urethra, but
in other circumstances a two stage repair is safer and gives
the best long term results.
7
In such circumstances a graft is
interposed as a flat plate between the two ends of the urethra
where a segment has been excised (or between the end of the
urethra and the external meatus if it is the most distal
A B
3
1
2
3
4
5
Figure 3 Illustrates how straightening
out the natural curve of the bulbar
urethra allows the surgeon to bridge a
considerable defect in urethral length.
The numbers are distances in
centimetres from the penobulbar
junction to the apex of the prostate at
usual radiographic magnifications.
Urethral strictures 491
www.postgradmedj.com
segment of the urethra that is involved). The flat plate is then
rolled in to form a tube and closed in layers at a second stage
three to six months later.
STRI CTURES BY SI TE AND TYPE
The urethra is typically described as having an anterior and
posterior segment. The anterior segment is surrounded by
corpus spongiosum and is divided into the penile (or
pendulous in American terminology) and bulbar segments.
The bulbar segment is the part enclosed by the bulbo-
spongiosus muscle. The posterior urethra is surrounded by
the prostate and the urethral sphincter and is divided into the
prostatic and membranous parts respectively. There is
insufficient space here to discuss any more sophisticated
anatomical sub-division of the posterior urethra; likewise,
strictures of the bladder neck and of the prostatic urethra,
usually the result of surgical treatment, particularly new
technology such as cryotherapy and laser therapy, which are
not generally considered as urethral strictures, will not be
considered here.
Posterior urethral strictures of the membranous urethra or
bulbo-membranous junction are usually the result of pelvic
fracture related urethral injury and are treated by anastomo-
tic urethroplasty in which the full range of manoeuvres
referred to above may be used and that may be an extremely
difficult surgical undertaking.
1416
Membranous urethral
strictures are sometimes the result of instrumentation as in
transurethral resection of the prostate in which case they are
known as sphincter strictures because it is fibrosis within
the urethral sphincter mechanism that is the primary
problem. To reserve sphincter function and therefore avoid
incontinence such strictures are best treated by urethral
dilatation where possible.
In the anterior urethra, bulbar urethral strictures are more
common than penile urethral strictures except in specialist
units where penile urethral strictures, because of previous
hypospadias surgery or lichen sclerosis,
25
are becoming
increasingly common. Short bulbar strictures as a result of
trauma or otherwise congenital are best treated by anasto-
motic urethroplasty. If a bulbar stricture is too long for
anastomotic urethroplasty, as is commonly the case, then a
stricturotomy and patch procedure is performed. When
anastomotic urethroplasty is possible this is usually a simple
and straightforward procedure when compared with anasto-
motic urethroplasty of the posterior urethra. A stricturotomy
and patch will usually use a buccal mucosal graft as a
patch.
2022
In the penile urethroplasty a stricturotomy and patch is
possible for simple strictures
26
but in more complicated
circumstances an excision and circumferential repair will be
necessary in which buccal mucosa may be used unless
preputial or penile shaft skin would be more appropriate. For
more complication situations, a staged reconstruction will be
used.
17
THE FUTURE OF URETHRAL STRI CTURE SURGERY
The results of anastomotic repair are so good and so well
sustained that it seems unlikely that this will be superseded
at any stage in the foreseeable future by any new develop-
ment.
Most strictures requiring substitution urethroplasty also do
well with modern surgical technique but if the procedure
could be performed endoscopically rather than by open
surgery then this would clearly be an advantage to the
patient. The real problems are the more complicated
strictures, which are generally longer and have already
undergone previous surgery and have recurred. They are also
typically in the penile urethra and associated with lichen
sclerosis. Many urologists hopes have been raised by
developments in tissue engineering to provide an alternative
source of material for repair of these difficult strictures. I am
somewhat sceptical about these developments because I do
not think it is the lack of the material that is the problemI
think it is the nature of the underlying disease. Future
surgical developments, in my opinion, will be the conse-
quence of a better understanding of the nature of the disease
in such patients and from a different approach to treating the
diseased but not actually strictured urethra rather than from
improvement in technique alone.
Funding: none.
Conflicts of interest: none.
REFERENCES
1 Chambers R, Baitera B. The anatomy of urethral stricture. BJU
1977;49:54551.
2 Romero Perez P, Mira Linares A. Complications of the lower urinary tract
secondary to urethral stenosis. Actas Urol Esp 1996;20:78693.
3 Devereux M, Burfield G. Prolonged follow-up of urethral strictures treated by
intermittent dilatation. BJU 1970;42:2319.
4 Pansadoro V, Emiliozzi P. Internal urethrotomy in the management of anterior
urethral strictures: long-term follow up. J Urol 1996;156:735.
5 Steenkamp J, Heyns C, De Kock M. Internal urethrotomy versus dilatation as
treatment for male urethral strictures: a prospective, randomised comparison.
J Urol 1997;157:98101.
6 Heyns C, Steenkamp JW, De Kock ML, et al. Treatment of male urethral
strictures: is repeated dilatation of internal urethrotomy useful? J Urol
1998;160:3568.
Summary of the general pri nci pl es of
urethropl asty
N
Urethral and visual internal urethrotomy are equally
effective
N
50% of short bulbar strictures are cured by the very first
dilatation or urethrotomy
N
Penile urethral strictures are rarely cured by dilatation
or urethrotomy
N
If a patient develops a recurrent stricture after a
previous urethrotomy or dilatation, however long the
interval, further instrumentation is never curative
N
The only curative alternative is urethroplasty
N
Whenever a urethroplasty is necessary an anastomotic
urethroplasty is preferable because it has a lower re-
stricture rate, success is maintained long term and the
complication rate is lower
N
Substitution urethroplasty is necessary for longer
bulbar strictures and all strictures of the penile urethra
N
For most urethral strictures requiring substitution
urethroplasty a stricturotomy and patch is preferable
to excision and a tube-graft flap
N
Grafts and flaps are equally good in most circum-
stances
N
In the bulbar urethra grafts are quicker and easier
N
A dorsal stricturotomy and patch has a higher success
rate and a lower complication rate than ventral
stricturotomy and patch
N
Buccal mucosal grafting has advantages for strictur-
otomy and patch in the bulbar urethra
N
In the penile urethra a flap is quicker and easier
N
When a circumferential repair is required a two stage
reconstruction is safer and more reliable than a one
stage technique
492 Mundy
www.postgradmedj.com
7 Harriss D, Beckingham IJ, Lemberger RJ, et al. Long-term results of intermittent
low-friction self-catheterisation in patients with recurrent urethral strictures.
BJU 1994;74:7902.
8 Milroy E, Chapple C, Wallsten H. A new stent for the treatment of urethral
strictures: preliminary report. BJU 1989;63:3926.
9 Badlani G, Press SM, Defaclo A, et al. Urolume endourethral prosthesis for the
treatment of urethral strictures disease: long-term results of the North
American multicenter urolume trial. Urology 1995;45:84656.
10 Milroy E, Allen A. Long-term results of urolume urethral stent for recurrent
urethral strictures. J Urol 1996;155:9048.
11 Mundy A. Results and complications of urethroplasty and its future. BJU
1993;71:3225.
12 Andrich DE, Mundy AR. Urethral strictures and their surgical treatment. BJU Int
2000;86:57180.
13 Turner-Warwick R. Urethral stricture surgery. In: Mundy A, ed.
Current operative surgeryurology. London: Bailliere Tindall,
1988:160218.
14 Webster G, Ramon J. Repair of pelvic fracture posterior urethral defects using
an elaborated perineal approach: experience with 74 cases. J Urol
1991;145:7448.
15 Koraitim M. The lessons of 145 post traumatic posterior urethral strictures
treated in 17 years. J Urol 1995;153:636.
16 Mundy A. Reconstruction of posterior urethral distraction defects. Atlas Urol
Clin North Am 1997;165:14925.
17 Greenwell T, Venn S, Mundy A. Changing practice in anterior urethroplasty.
BJU Int 1998;83:6315.
18 Jordan G, Devine P. Application of tissue transfer techniques to the
management of urethral strictures. Semin Urol 1987;5:21935.
19 Wessels H, McAninch J. Current controversies in anterior urethral stricture
repair: free-graft versus pedicled skin-flap reconstruction. World J Urol
1998;16:17580.
20 Barbagli G, Selli C, di Cello V, et al. A one-stage dorsal free-graft
urethroplasty for bulbar urethral strictures. BJU 1996;78:92932.
21 Iselin C, Webster G. Dorsal onlay urethroplasty for urethral stricture repair.
World J Urol 1998;16:1815.
22 Andrich D, Mundy A. The Barbagli procedure gives the best results for patch
urethroplasty of the bulbar urethra. BJU Int 2001;88:3859.
23 Mundy A. The long-term results of skin inlay urethroplasty. J Urol
1972;107:97780.
24 Quartey J. One-stage penile/preputial island flap urethroplasty for urethral
stricture. J Urol 1985;134:47487.
25 Venn S, Mundy A. Urethroplasty for balanitis xerotica obliterans. BJU
1998;81:7357.
26 Orandi A. One-stage urethroplasty. BJU 1968;40:71719.
Clinical EvidenceCall for contributors
Clinical Evidence is a regularly updated evidence-based journal available worldwide both as
a paper version and on the internet. Clinical Evidence needs to recruit a number of new
contributors. Contributors are healthcare professionals or epidemiologists with experience in
evidence-based medicine and the ability to write in a concise and structured way.
Areas for which we are currently seeking contributors:
N
Pregnancy and childbirth
N
Endocrine disorders
N
Palliative care
N
Tropical diseases
We are also looking for contributors for existing topics. For full details on what these topics
are please visit www.clinicalevidence.com/ceweb/contribute/index.jsp
However, we are always looking for others, so do not let this list discourage you.
Being a contributor involves:
N
Selecting from a validated, screened search (performed by in-house Information
Specialists) epidemiologically sound studies for inclusion.
N
Documenting your decisions about which studies to include on an inclusion and exclusion
form, which we keep on file.
N
Writing the text to a highly structured template (about 1500-3000 words), using evidence
from the final studies chosen, within 8-10 weeks of receiving the literature search.
N
Working with Clinical Evidence editors to ensure that the final text meets epidemiological
and style standards.
N
Updating the text every 12 months using any new, sound evidence that becomes available.
The Clinical Evidence in-house team will conduct the searches for contributors; your task is
simply to filter out high quality studies and incorporate them in the existing text.
If you would like to become a contributor for Clinical Evidence or require more information
about what this involves please send your contact details and a copy of your CV, clearly
stating the clinical area you are interested in, to CECommissioning@bmjgroup.com.
Call for peer reviewers
Clinical Evidence also needs to recruit a number of new peer reviewers specifically with an
interest in the clinical areas stated above, and also others related to general practice. Peer
reviewers are healthcare professionals or epidemiologists with experience in evidence-based
medicine. As a peer reviewer you would be asked for your views on the clinical relevance,
validity, and accessibility of specific topics within the journal, and their usefulness to the
intended audience (international generalists and healthcare professionals, possibly with
limited statistical knowledge). Topics are usually 1500-3000 words in length and we would
ask you to review between 2-5 topics per year. The peer review process takes place
throughout the year, and out turnaround time for each review is ideally 10-14 days.
If you are interested in becoming a peer reviewer for Clinical Evidence, please complete the
peer review questionnaire at www.clinicalevidence.com/ceweb/contribute/peerreviewer.jsp
Urethral strictures 493
www.postgradmedj.com
You might also like
- ASPEN Enteral Nutrition Handbook, 2nd EditionDocument249 pagesASPEN Enteral Nutrition Handbook, 2nd EditionYohana Elisabeth Gultom100% (4)
- Teeth RestorabilityDocument6 pagesTeeth RestorabilityMuaiyed Buzayan AkremyNo ratings yet
- Teknik Operasi Splenektomi 2Document31 pagesTeknik Operasi Splenektomi 2sphericalfaNo ratings yet
- To Perforasi GasterDocument27 pagesTo Perforasi GasterPuthu BelegugNo ratings yet
- Pande Komang Gerry Paramesta: Decision Making in Bowel Obstruction: A Review byDocument32 pagesPande Komang Gerry Paramesta: Decision Making in Bowel Obstruction: A Review byanon_550250832100% (1)
- Striktur UrethraDocument7 pagesStriktur UrethraEl-yes Yonirazer El-BanjaryNo ratings yet
- BPHDocument10 pagesBPHMichelle SalimNo ratings yet
- Mediastinal Tumors: Kibrom Gebreselassie, MD, FCS-ECSA Cardiovascular and Thoracic SurgeonDocument52 pagesMediastinal Tumors: Kibrom Gebreselassie, MD, FCS-ECSA Cardiovascular and Thoracic SurgeonVincent SerNo ratings yet
- Diaphragma InjuryDocument18 pagesDiaphragma InjuryAhmedNo ratings yet
- Thyroid Cancer Diagnosis and ManagementDocument45 pagesThyroid Cancer Diagnosis and Managementapi-3704562100% (1)
- 2013 - Pancreaticoduodenectomy (Whipple Procedure) TechniquesDocument11 pages2013 - Pancreaticoduodenectomy (Whipple Procedure) TechniquesOlteanu IonutNo ratings yet
- Perforasi GasterDocument29 pagesPerforasi GasterrezaNo ratings yet
- Surgery of PancreasDocument30 pagesSurgery of PancreasmackieccNo ratings yet
- Jurnal CA TyroidDocument4 pagesJurnal CA TyroidErvina ZelfiNo ratings yet
- Jurnal Tyroid PDFDocument3 pagesJurnal Tyroid PDFVinnaNo ratings yet
- Trauma UrogenitalDocument17 pagesTrauma UrogenitalsultantraNo ratings yet
- Xanthogranulomatous PyelonephritisDocument14 pagesXanthogranulomatous PyelonephritisalaaNo ratings yet
- Abdominal Trauma - Dr. Febiansyah Ibrahim, SPB-KBDDocument32 pagesAbdominal Trauma - Dr. Febiansyah Ibrahim, SPB-KBDPrandyNo ratings yet
- Salter 15Document70 pagesSalter 15Kahfi Rakhmadian KiraNo ratings yet
- CCDuodenum Periampullary Neoplasms ChuDocument68 pagesCCDuodenum Periampullary Neoplasms ChuSahirNo ratings yet
- Metastasis Bone DiseaseDocument11 pagesMetastasis Bone DiseasedrkurniatiNo ratings yet
- Kompartemen SindromDocument9 pagesKompartemen SindromPutri PratiwiNo ratings yet
- Subcutaneous: EmphysemaDocument70 pagesSubcutaneous: EmphysemaWer TeumeNo ratings yet
- ColostomyDocument45 pagesColostomydrqiekiNo ratings yet
- Pediatric Surgery Day 1Document267 pagesPediatric Surgery Day 1ironbuangNo ratings yet
- 2017 Bone Modifying Agents in Met BC Slides - PpsDocument14 pages2017 Bone Modifying Agents in Met BC Slides - Ppsthanh tinh BuiNo ratings yet
- OsteosarkomaDocument2 pagesOsteosarkomaLinawati DLNo ratings yet
- ANATOMI ColorectalDocument16 pagesANATOMI ColorectalShannonCPMNo ratings yet
- Akses Vena Central: Anestesiologi Dan Reanimasi RSUD TasikmalayaDocument28 pagesAkses Vena Central: Anestesiologi Dan Reanimasi RSUD TasikmalayaSaeful AmbariNo ratings yet
- Early Detection and Management Colorectal CancerDocument59 pagesEarly Detection and Management Colorectal CancerAbduh BIKNo ratings yet
- Skull Cervical X-RayDocument15 pagesSkull Cervical X-RayAwal AlfitriNo ratings yet
- Wound de His Cence FinalDocument26 pagesWound de His Cence Finaldanil armandNo ratings yet
- Trauma BuliDocument32 pagesTrauma BulimoonlightsoantaNo ratings yet
- Principles of Management of Soft Tissue SarcomaDocument33 pagesPrinciples of Management of Soft Tissue Sarcomabashiruaminu100% (1)
- MESSDocument9 pagesMESStaufik sofistiawanNo ratings yet
- Anal Stenosis and Mucosal EctropionDocument7 pagesAnal Stenosis and Mucosal EctropionpologroNo ratings yet
- Bladder Substitution and Urinary DiversionDocument58 pagesBladder Substitution and Urinary DiversionlifespotNo ratings yet
- Chronic Limb IschemiaDocument29 pagesChronic Limb IschemiaSadia NaveedNo ratings yet
- Nervus Laryngeus RecurrensDocument5 pagesNervus Laryngeus RecurrensAri Julian SaputraNo ratings yet
- HypospadiaDocument45 pagesHypospadiaMartha P100% (1)
- CURRENT STATUS of HAL-RAR (Haemorrhoids Casee and Treatment in Indonesia) Prof - Dr.dr. Ing - Riwanto, SPB-KBDDocument43 pagesCURRENT STATUS of HAL-RAR (Haemorrhoids Casee and Treatment in Indonesia) Prof - Dr.dr. Ing - Riwanto, SPB-KBDHengky TanNo ratings yet
- Systemic Therapies of CRC: Johan KurniandaDocument56 pagesSystemic Therapies of CRC: Johan KurniandaANISA RACHMITA ARIANTI 2020No ratings yet
- Chest TubeDocument8 pagesChest TubeTaufik Nur YahyaNo ratings yet
- Torsio Testis2016Document6 pagesTorsio Testis2016Patrico Rillah SetiawanNo ratings yet
- Acute Abdomen and PeritonitisDocument17 pagesAcute Abdomen and PeritonitisAnisaPratiwiArumningsihNo ratings yet
- Breast Cancer: Katherine Macgillivray & Melissa PoirierDocument62 pagesBreast Cancer: Katherine Macgillivray & Melissa PoirierJonathan Darell WijayaNo ratings yet
- The Surgical Anatomy of The Nerve Laryngeal RecurrensDocument2 pagesThe Surgical Anatomy of The Nerve Laryngeal RecurrensvaNo ratings yet
- Rangkuman Salter Bab 14Document64 pagesRangkuman Salter Bab 14Febee NathaliaNo ratings yet
- Colonoscopy CecilDocument14 pagesColonoscopy Cecilyaba100% (1)
- U04 Fxs of Humeral ShaftDocument88 pagesU04 Fxs of Humeral Shaftadrian_mogosNo ratings yet
- Tokyo Guidelines 2018 Flowchart For The Management of Acute CholecystitisDocument43 pagesTokyo Guidelines 2018 Flowchart For The Management of Acute Cholecystitisfranciscomejia14835No ratings yet
- 2010 TNM Staging Colorectal CADocument2 pages2010 TNM Staging Colorectal CAbubbrubb20063998No ratings yet
- Tracheostomy: Berlian Chevi A. 20184010030Document26 pagesTracheostomy: Berlian Chevi A. 20184010030Berlian Chevi e'Xgepz ThrearsansNo ratings yet
- PCNDocument3 pagesPCNAzirah TawangNo ratings yet
- Intestinal Stomas - AKTDocument49 pagesIntestinal Stomas - AKTTammie YoungNo ratings yet
- Distribusi Patah Tulang Panjang TerbukaDocument73 pagesDistribusi Patah Tulang Panjang TerbukaCininta Anisa SavitriNo ratings yet
- Diagnosis and Classification of Urethral InjuriesDocument13 pagesDiagnosis and Classification of Urethral Injuriesleo100% (2)
- Oeis SyndromeDocument9 pagesOeis SyndromeADEENo ratings yet
- Cystostomy NewDocument32 pagesCystostomy Newkuncupcupu1368No ratings yet
- Colonic Volvulus: Disusun Oleh: Dhea Faizia Tasya (2110221036) Pembimbing: Dr. Yulia Rachmawati, Sp. Rad (K)Document25 pagesColonic Volvulus: Disusun Oleh: Dhea Faizia Tasya (2110221036) Pembimbing: Dr. Yulia Rachmawati, Sp. Rad (K)Dhea Faizia TasyaNo ratings yet
- Stenosing Tenosynovitis, (Trigger Finger) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandStenosing Tenosynovitis, (Trigger Finger) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- 1543 2742 Article p13Document8 pages1543 2742 Article p13Yohana Elisabeth GultomNo ratings yet
- Platelet To Lymphocyte Ratio As A Potential.27Document8 pagesPlatelet To Lymphocyte Ratio As A Potential.27Yohana Elisabeth GultomNo ratings yet
- Prognostic Markers Compared To CD3 TIL in Locally.83Document7 pagesPrognostic Markers Compared To CD3 TIL in Locally.83Yohana Elisabeth GultomNo ratings yet
- 2020 ESC Guidelines On Sports Cardiology and Exercise in Patients With Cardiovascular DiseaseDocument80 pages2020 ESC Guidelines On Sports Cardiology and Exercise in Patients With Cardiovascular DiseaseKlaraNo ratings yet
- Modern Aspects of Burn Injury ImmunopathogenesisDocument12 pagesModern Aspects of Burn Injury ImmunopathogenesisYohana Elisabeth GultomNo ratings yet
- Please Take This Boarding Pass To The Airport For Your IghtDocument1 pagePlease Take This Boarding Pass To The Airport For Your IghtYohana Elisabeth GultomNo ratings yet
- J Cachexia Sarcopenia Muscle - 2022 - Paval - A Systematic Review Examining The Relationship Between Cytokines and CachexiaDocument15 pagesJ Cachexia Sarcopenia Muscle - 2022 - Paval - A Systematic Review Examining The Relationship Between Cytokines and CachexiaYohana Elisabeth GultomNo ratings yet
- Handout - 2!22!22 Nutrition Implication On Long Covid ASPENDocument54 pagesHandout - 2!22!22 Nutrition Implication On Long Covid ASPENYohana Elisabeth GultomNo ratings yet
- Inflammation Marker and Micronutrient DeficiencyDocument19 pagesInflammation Marker and Micronutrient DeficiencyYohana Elisabeth GultomNo ratings yet
- Hypocalcemia: Michelle Sergel (PDocument15 pagesHypocalcemia: Michelle Sergel (PYohana Elisabeth GultomNo ratings yet
- Hypocalcemia Pada Beta Thalassemia PDFDocument3 pagesHypocalcemia Pada Beta Thalassemia PDFYohana Elisabeth GultomNo ratings yet
- Bladder: Male Urethra and Its SegmentsDocument33 pagesBladder: Male Urethra and Its SegmentsYohana Elisabeth GultomNo ratings yet
- PeritonitisDocument9 pagesPeritonitismardsz100% (4)
- Essay Sex AbuseDocument4 pagesEssay Sex AbuseFang KenNo ratings yet
- Psychoimmunology Essay by DR Romesh Senewiratne-Alagaratnam (MD)Document32 pagesPsychoimmunology Essay by DR Romesh Senewiratne-Alagaratnam (MD)Dr Romesh Arya Chakravarti100% (2)
- An Alternative Impression Technique For Mobile TeethDocument25 pagesAn Alternative Impression Technique For Mobile TeethmujtabaNo ratings yet
- CaDocument10 pagesCaShielany Ann Abadingo100% (1)
- Diet Readiness QuestionnaireDocument3 pagesDiet Readiness Questionnairesavvy_as_98100% (1)
- ATLSDocument22 pagesATLSHemant Khambhati78% (9)
- Obesity: Differential DiagnosisDocument0 pagesObesity: Differential Diagnosisrasputin22100% (1)
- Medical EthicsDocument27 pagesMedical Ethicspriyarajan007No ratings yet
- Cerebral Aneurysm FINALDocument33 pagesCerebral Aneurysm FINALkanejasper0% (2)
- Surgical TechniqueDocument52 pagesSurgical TechniqueKutub SikderNo ratings yet
- Atlas of Abdominal Wall ReconstructionDocument14 pagesAtlas of Abdominal Wall ReconstructionEmmanuel BarriosNo ratings yet
- b2 CoolDocument2 pagesb2 CoolGanesh kumarNo ratings yet
- Oral and Maxillofacial PathologyDocument79 pagesOral and Maxillofacial PathologyMai AnhNo ratings yet
- Viaro 2022 - 2Document8 pagesViaro 2022 - 2moikaufmannNo ratings yet
- Formulir Klaim Rawat InapDocument2 pagesFormulir Klaim Rawat InapGoris DonkeyNo ratings yet
- Inhaled Budesonide in The Treatment of Early COVID-19Document10 pagesInhaled Budesonide in The Treatment of Early COVID-19Dusan OrescaninNo ratings yet
- Xanax Drug CardDocument3 pagesXanax Drug Cardnasir khanNo ratings yet
- HKG - Exercise Prescription (Doctor's Handbook)Document126 pagesHKG - Exercise Prescription (Doctor's Handbook)Chi-Wa CWNo ratings yet
- Roleplay FastfoodDocument9 pagesRoleplay FastfoodIndra DarmaNo ratings yet
- IE Humeral Neck FractureDocument9 pagesIE Humeral Neck FractureEarll Justin N. DataNo ratings yet
- Case Study 2Document3 pagesCase Study 2Thesa Ray PadernalNo ratings yet
- OT RotationDocument5 pagesOT RotationAnnbe BarteNo ratings yet
- NCM 100 - Lecture Final ExaminationDocument4 pagesNCM 100 - Lecture Final ExaminationjafcachoNo ratings yet
- Cardiogenic Brain Abscess in ChildrenDocument28 pagesCardiogenic Brain Abscess in ChildrenDina MarselinaNo ratings yet
- NUR 450 Unit 3 Exam Blueprint Summer 2019 LIU UniversityDocument2 pagesNUR 450 Unit 3 Exam Blueprint Summer 2019 LIU UniversityMohammad Malik100% (1)
- English For ChemistryDocument53 pagesEnglish For ChemistryNoah FathiNo ratings yet
- 21 FoodImpaction 20150102105737 PDFDocument4 pages21 FoodImpaction 20150102105737 PDFDina NovaniaNo ratings yet
- Diabetes InsipidusDocument2 pagesDiabetes InsipidusLuiciaNo ratings yet