Professional Documents
Culture Documents
J 1600-0501 2000 011S1083 X
J 1600-0501 2000 011S1083 X
Uploaded by
Mr-Ton Drg0 ratings0% found this document useful (0 votes)
5 views18 pagesOriginal Title
j.1600-0501.2000.011S1083.x(1)
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
5 views18 pagesJ 1600-0501 2000 011S1083 X
J 1600-0501 2000 011S1083 X
Uploaded by
Mr-Ton DrgCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 18
Clin Oral Impl Res 2000: 11 (Suppl.
): 83100 Copyright C Munksgaard 2000
Printed in Denmark All rights reserved
ISSN 0905-7161
Chapter 5
Surgical procedures in partially edentulous
patients with ITI implants
Buser D, von Arx T. Surgical procedures in partially edentulous patients
Daniel Buser, Thomas von Arx
with ITI implants.
Clin Oral Impl Res 2000: 11 (Suppl.): 83100. C Munksgaard 2000.
Dept. of Oral Surgery, University of Bern,
Bern, Switzerland
Today, partially edentulous patients represent the majority of patients
seeking treatment with implant-supported prostheses. This chapter presents
the specic aspects of the surgical handling of partially edentulous pa-
tients with either single-tooth gaps, extended edentulous spaces or distal
extension situations. Due to differences in treatment objectives, a distinc-
Key words: esthetic sites ITI
tion is made between sites without esthetic priority (non-esthetic sites) and
implants non-esthetic sites non-
with esthetic priority (esthetic sites). In non-esthetic sites, the primary goal
submerged approach SLA surface
of the surgical therapy is to achieve a predictable hard and soft tissue
submerged approach surgical
integration of the implant to re-establish function with the implant-sup- procedures
ported prosthesis. In esthetic sites, the goal of surgical therapy is to
achieve successful tissue integration and to obtain esthetic soft tissue con- Committee Members:
Leon A. Assael, USA, Jay Beagle, USA,
tours to re-establish both function and esthetics. Therefore, the surgeon
Alexandra Behneke, Germany, Jean-
must have a clear understanding of the specic needs in a given situation,
Pierre Bernard, Switzerland, Daniel
and must master the necessary surgical techniques concerning a correct
Buser, Switzerland, Karl Dula,
implant placement and a correct soft tissue handling to achieve the treat-
Switzerland, Christian Foitzik, Germany,
ment objectives. In non-esthetic sites, a non-submerged approach is
Michael Gahlert, Germany, So lve
clearly preferred, thus avoiding a second-stage procedure for abutment
Hellem, Sweden, Hans Peter Hirt,
connection. If a soft tissue correction is necessary to re-establish keratinized
Switzerland, Hideaki Katsuyama, Japan,
peri-implant mucosa, this is done at the time of implant placement with
Barbara Lehmann, Switzerland, Herbert
mucogingival surgery. In esthetic sites, a submerged implant placement is Niederdellmann, Germany, Stephen
Rimer, USA, Marcel Scacchi,
preferred to achieve esthetically pleasing soft tissue contours. If a soft
Switzerland, Wilfried Schilli, Germany,
tissue augmentation is necessary, this is done at the time of implant place-
Christiaan ten Bruggenkate, The
ment with connective tissue grafts. Thus, the second surgical procedure
Netherlands, A.V. van Gool, The
after 810 weeks of healing is reduced to a mucosaplasty like a punch
Netherlands, Thomas von Arx,
biopsy, avoiding an open ap procedure. Based on favorable properties
Switzerland, Gerhard Wahl, Germany,
of the TPS surface, short implants (6 or 8 mm) and short healing periods
Dieter Weingart, Germany
of 34 months have been successfully utilized in partially edentulous pa-
Prof. Dr. Daniel Buser, Department of
tients in the last 14 years. The introduction of the SLA surface allows a
Oral Surgery, School of Dental Medicine,
further reduction of the healing period to 6 weeks of healing in all sites
University of Berne, Freiburgstrasse 7,
with normal bone density (class IIII). In summary, the ITI philosophy
CH-3010 Berne, Switzerland
offers straightforward surgical concepts to predictably achieve the treat-
Tel.: 41 31 632 25 55
ment objectives with the least demanding surgical protocol, reducing the
Fax: 41 31 632 98 84
related chairtime and costs for the patient and the clinician. e-mail: daniel.buser/zmk.unibe.ch
ITI implants have been increasingly utilized for the
rehabilitation of partially edentulous patients in
the past 14 years. As with Brnemark implants,
the clinical testing of ITI implants started more
than 25 years ago, primarily in fully edentulous
patients for implant-supported bar-type overden-
tures. These implant prototypes were all one-part
implants such as the TPS screw or the type F hol-
83
low-cylinder implant, meaning that the abutment
was an integral part of the implant (monocorp de-
sign). Retrospective studies demonstrated promis-
ing long-term results with these implant types in
this specic indication (Ledermann 1979, 1984;
Babbush et al. 1986; ten Bruggenkate et al. 1990;
Krekeler et al. 1990; Ledermann 1996). In the
1980s, based on this positive clinical experience
Buser & von Arx
with osseointegrated ITI implants in fully edentu-
lous patients, clinicians started to use ITI implants
more and more in various clinical situations in par-
tially edentulous patients, such as single-tooth
gaps, distal extension situations or extended eden-
tulous spaces. This trend was supported by the de-
velopment of two-part ITI implants in 1985/86 (see
chapter 1), since these newly designed implants of-
fered much more exibility for the clinicians from
a prosthetic point of view. This progress has led to
a signicant expansion of implant therapy in the
1990s. Today, more than 80% of patients treated
with dental implants are partially edentulous
(Bernard et al. 1995; Buser et al. 1997).
This development has had certain consequences
for the design and clinical utilization of dental im-
plants. First, the number of inserted implants per
patient has clearly dropped in recent years. The
latest clinical studies reported an average of ap-
proximately two implants per patient (Bernard et
al. 1995; Buser et al. 1997, 1999a). Therefore, most
implant reconstructions are no longer supported
by 46 implants splinted together in a cross-arch
arrangement to reinforce the anchorage base. To-
day, a majority of implant prostheses such as single
crowns or short-span xed partial dentures are
supported by only one or two implants. Second,
implants are frequently placed in areas of the jaw
where the bone density is quite often low, the bone
height reduced, but the functional load high. This
is particularly true for implants in posterior areas
of both jaws. In sites with these anatomical charac-
teristics, short implants have to be utilized quite
often due to a reduced bone height.
Summarizing these aspects, a signicant number
of implants since they are placed in posterior
areas to support single crowns or short-span
bridges have to withstand a clearly increased
functional stress at the bone-implant interface and
at the implant-abutment complex in comparison
with multiple implants being splinted in a cross-
arch arrangement. Therefore, implants have to be
appropriately designed in order to be successful in
these demanding clinical situations. Based on these
increased requirements for dental implants, bio-
mechanical aspects as well as surface properties of
titanium implants have become topics of interest
in implant dentistry in recent years. They are cru-
cial for the long-term success of endosseous im-
plants in demanding clinical situations as outlined
above.
In the following, the surgical procedures used in
partially edentulous patients will be presented in
detail. It was decided by the surgical group of the
ITI Consensus Conference to distinguish between
implant placement in sites without esthetic priority
(non-esthetic sites) and sites with esthetic prior-
84
ity (esthetic sites), since signicant differences in
the surgical approach are apparent between these
two groups.
Implant placement in non-esthetic sites
General remarks
Non-esthetic sites still represent the majority of
sites treated with endosseous implants. This in-
cludes a variety of implant indications listed in
Table 5.1.
The primary objective of implant therapy is
clearly the re-establishment of function, whereas
esthetic aspects are less important. Further objec-
tives include (Table 5.2) the achievement of a long-
term result with the least demanding surgical and
prosthetic procedure for the patient and the clini-
cian, to reduce the chairside time and the related
costs. Hence, a non-submerged approach is clearly
preferred, to avoid a second surgical procedure. If
necessary, special soft tissue techniques are utilized
to maintain or create a keratinized peri-implant
mucosa at the time of implant placement. Conse-
quently, the shoulder of the integrated implant is
normally located at the soft tissue level, allowing
easy access for the subsequent prosthetic pro-
cedures. In most cases, the patients are restored
with cemented restorations utilizing conical solid
abutments. As outlined in chapter 1, the implant-
abutment connection is based on the morse taper
principle, with an 8
o
inner cone (Sutter et al. 1988,
1993). This interface provides an optimal friction
t, thereby transmitting functional loading forces
from the abutment directly to the implant body
and from there into the surrounding bone struc-
ture without exerting undesirable bending mo-
ments to the abutment screw. This connection is
clearly superior from a biomechanical point of
Table 5.1. Various indications in non-esthetic sites
O Distal extension situations in both jaws
O Single-tooth gaps in the mandible
O Single-tooth gaps in the posterior maxilla
O Extended edentulous spaces in the mandible
O Extended edentulous spaces in the posterior maxilla
Table 5.2. Treatment objectives in non-esthetic sites
O Main emphasis: re-establishment of function
O Achievement of long-term stability from a functional point of view
O Least demanding surgical procedure for patient and clinician allowing for successful
tissue integration with high predictability
Non-submerged approach is clearly preferred
O Maintenance or establishment of keratinized peri-implant mucosa
Surgical procedures in partially edentulous patients
view when compared with a at hex-top connec-
tion (Sutter et al. 1993).
In distal extension situations in standard cases,
implant-borne restorations are normally not ex-
tended beyond the rst molar area for functional,
practical and economic reasons. This is in accord-
ance with well-documented long-term studies
evaluating the number of occlusal units necessary
for sufcient masticatory function (Kayser 1989).
If an existing upper second molar requires an oc-
clusal stop to avoid overeruption, the implant-
borne restoration in the mandible can be extended
to the mesial area of the second molar. In these
cases, the mandibular rst molar is replaced by
two implants to be restored with two premolar-
sized units of approximately 8 mm mesio-distal di-
ameter.
The use of premolar-sized units for implant-
borne xed partial dentures (FPDs) is rec-
ommended. This has proven its efcacy in more
than 10 years of clinical experience (Buser et al.
1988; Bragger et al. 1990; Belser et al. 1996a;
Belser & Buser 1997). In fact, a crown of 78 mm
mesio-distal diameter is ideal to allow a harmoni-
ous axial prole gradually emerging from the im-
plant shoulder ( 4.8 mm) to the maximum cir-
cumference. In addition, the occlusal table is re-
duced, hereby diminishing the risk of unfavorable
bending moments for the implants and their com-
ponents. There is only one exception to that rule
namely, the single-tooth replacement in a molar
site. For this indication, the wide-neck implant
(WN 4.8) was developed in the late 1990s. The
larger diameter of 6.5 mm in the shoulder area
allows a harmonious axial prole of the molar
crown.
As far as number and distribution of implants
are concerned, the following guidelines for routine
use have been established over the past 14 years.
Fig. 5.1. ITI philosophy for treating a 3-unit gap: two implants
support a 3-unit FPD with a central pontic. Radiographic fol-
low-up at 5 years with two SLA implants.
85
Fig. 5.2. One implant per missing tooth is used in special cir-
cumstances such as in implant sites with reduced bone height.
The two 6 mm SLA implants are splinted to a longer 10 mm
implant.
Fig. 5.3. A distal extension situation can also be treated with
two implants distally and a 3-unit FPD with a mesial cantilever.
O In case of three missing occlusal units and suf-
cient bone anatomy, the standard solution con-
sists of the placement of two implants to sup-
port a 3-unit FPD with a central pontic (Fig.
5.1).
O The replacement of each premolar unit by one
implant is reserved for clinical situations in
which either diameter-reduced or short implants
of 6 or 8 mm length have to be used (Fig. 5.2).
O If a mesial implant cannot be inserted due to
anatomical restrictions, a 3-unit FPD with a
mesial cantilever has proven to be a viable alter-
native (Fig. 5.3).
O A distal cantilever unit or connection to natural
teeth should only be used in exceptional situ-
ations.
Recently, it has been proposed that at least three
implants be inserted in a distal extension situation,
with the xtures placed in a tripod fashion (the
central implant offset buccally) rather than in a
straight line (Rangert et al. 1997), the idea being
Buser & von Arx
to diminish bending moments and potential bio-
mechanical complications (screw and abutment
loosening, fractures of components of the implant-
abutment complex). This theoretical recommenda-
tion, however, appears impractical from a clinical
point of view because of space limitations in either
mesio-distal or orofacial dimensions, and it in-
creases the related treatment costs signicantly.
With regard to ITI implants, this recommendation
does not apply, since ITI implants (a) achieve a
signicantly stronger bone anchorage with a rough
TPS or a microrough SLA surface when compared
to titanium implants with a machined surface
(Buser et al. 1999b); b) have a much stronger im-
plant-abutment complex based on the morse taper
principle when compared to a at hex-top connec-
tion (Sutter et al. 1993); and c) are preferably re-
stored with cemented restorations in posterior
areas, eliminating the risk for screw loosening
(Buser et al. 1988; Bragger et al. 1990; Belser et al.
1996a; Belser & Buser 1997).
Preoperative examination in non-esthetic sites
Clinical evaluation
During preoperative examination, the following
clinical parameters have to be assessed: (a) the sa-
gittal and transversal relationship, (b) presence of
an intermaxillary distance of at least 33 mm to
allow the preparation of the implant bed with the
shortest drill, (c) the evaluation of the local bone
anatomy, when necessary with a bone mapping
procedure, and (d) the evaluation of the local soft
tissue conditions.
Radiographic evaluation
In standard cases, the utilization of a panoramic
radiograph and/or periapical radiographs is suf-
cient. Quite often, the panoramic radiographs are
combined with steel balls of 5 mm diameter to
evaluate the distortion factor of the radiograph
(Buser et al. 1990). Tomograms or CT scans are
reserved for special clinical situations such as pa-
tients presenting with bone defects. CT scans
should not be used routinely, since they cause a
signicant radiation exposure to the patient (Dula
et al. 1996), and they are quite costly in most coun-
tries.
Selection of implant location
Based on the already outlined concept of using pri-
marily xed partial dentures with premolar-sized
units, the distances from the root surface of ad-
jacent teeth to the central axis of planned implants
are chosen based on the 51219 mm rule. This
rule does not apply in single-tooth gaps, where the
86
central point of the edentulous space is normally
chosen for the preparation of the implant bed.
Selection of implant type
The solid-screw implant, with its various dimen-
sions (S. 4.1, S 4.8, S 3.3, NN 3.3, WN 4.8), is
exclusively utilized in these applications. The se-
lected implant diameter depends on the crest width
available, as outlined in chapter 3. A minimal crest
width of 4.8 mm is required for the diameter-re-
duced screw implant (S 3.3). This implant type
should be splinted with other implants whenever
possible, since it has a certain risk for a fatigue
fracture. It is therefore not suitable for appli-
cations risking excessive bending moments, such
as for the single-tooth replacement of molars or
canines. In the case of a reduced bone height lead-
ing to the utilization of short implants (6 or 8 mm),
the placement of wide-body implants (S 4.8 mm,
WN 4.8) is preferred if the crest width allows for
it (minimal width of 6.2 mm). This is quite often
feasible, particularly in molar sites. In case of short
(6 and 8 mm) or diameter-reduced (S 3.3) im-
plants, additional implants are recommended to
increase the anchoring base in the bone. In ad-
dition, splinting these implants together is rec-
ommended. In these special situations, one im-
plant is utilized per missing tooth. Otherwise, only
two implants are necessary to support a 3- or 4-
unit FPD, and three implants for a 4- or 5-unit
FPD (see above). The narrow-neck implant (NN
3.3) is primarily utilized for single-tooth gaps in
the anterior mandible, whereas the wide-neck im-
plant (WN 4.8) is applied for single-tooth gaps in
the molar area of both jaws.
Selection of implant length
The implant length to be chosen depends on the
vertical bone height and the preoperative radio-
graphic analysis. In standard situations, the long-
Fig. 5.4. Due to the utilization of short 8 mm implants, a sinus
grafting procedure could be avoided.
Surgical procedures in partially edentulous patients
est possible implants up to 12 mm are chosen.
Since bicortical stabilization is not necessary for
ITI implants, with their roughened titanium sur-
face, a security distance of 12 mm to the man-
dibular canal should be respected whenever poss-
ible. This conservative concept offers minimal risk
of damaging the neurovascular bundle (Bernard et
al. 1995). In contrast, a surprisingly high fre-
quency of nerve complications (14% after stage I
surgery; still 4% at three years of follow-up) has
been reported for Brnemark implants with a ma-
chined surface seeking bicortical stabilization on
the roof of the mandibular canal (Higuchi et al.
1995). In the maxilla, the available bone height is
always utilized as much as possible, since a minor
perforation of the maxillary sinus does not appear
to create clinical problems. The successful utiliza-
tion of short 6 or 8 mm ITI implants, with their
excellent bone anchoring properties, makes it fre-
quently possible to avoid demanding surgical pro-
cedures such as sinus grafting in the maxilla or
nerve lateralization in the mandible (Figs 5.4 and
5.5).
Surgical procedure in non-esthetic sites
At the beginning, a midcrestal incision of the mu-
cosa is carried out, whenever possible located in
keratinized mucosa. Following elevation of the
mucoperiosteal aps, the alveolar crest is exam-
ined. Quite often, crest attening is indicated to
achieve a at crest surface. The surgeon, however,
should ensure that an extended opening of cancel-
lous bone is avoided. Subsequently, the appropri-
ate implant positions can be selected and marked
with a small round bur. The utilization of surgical
guides is not advocated for all patients, but is quite
useful in extended edentulous situations without
suitable landmarks, such as a missing canine.
The preparation of the implant bed is carried
out with spiral drills of increasing diameter. These
spiral drills are characterized by an excellent cut-
ting quality and overdrilling of only 0.4 mm, which
is important in posterior sites in the mandible. A
recent in vitro study demonstrated that these drills
are long-lasting with an appropriate sterilization
protocol, since they can be used for the prepara-
tion of more than 50 implant beds (Chappuis
2000). Between the different spiral drills, the util-
ization of round burs and prole drills is rec-
ommended to open the entrance of the implant
bed. Depth gauges of various dimensions are use-
ful to check the direction of the prepared implant
axis and the sink depth. Tapping of the thread is
done in recipient sites with normal bone density
(class IIII), whereas no tapping is carried out in
spongy bone (class IV). Tapping and implant inser-
87
tion can be done either with a hand ratchet or with
an adapter attached to a special contra-angle
handpiece. Implant insertion with the insertion de-
vice requires a very slow speed of approximately
15 rpm. ITI implants are sold with a premounted
insertion device allowing a non-touch handling of
the implant. When the implant reaches the nal
vertical position recognizable by increasing resis-
tance to insertion the insertion device can be eas-
ily detached with the help of a xation key and a
counter-clockwise rotation of the handpiece. The
appropriate insertion depth depends on the clinical
situation and the personal preference of the sur-
geon. In standard situations, the border of the
roughened titanium surface is located either at the
bone crest or slightly below (1 mm). Next, the
appropriate healing caps are selected. In most
cases, a 1.5 mm or a 3 mm healing cap is utilized.
This selection depends on the clinical soft tissue
situation. Wound closure for a non-submerged
healing is initiated by a precise and tension-free
adaptation of the mucosal margins to the implant
post or healing cap. When necessary, the utiliza-
tion of small releasing incisions or small pedicle
aps is recommended. A ne atraumatic suture
material (size 40 or 50) is utilized. When kera-
tinized mucosa is lacking, soft tissue grafting may
be necessary to re-establish a sufcient band of
keratinized mucosa. Usually, a postsurgical radio-
graph is taken to control the implant position and
implant direction. In addition, a postsurgical
radiograph can be indicated for forensic reasons.
Post-operative treatment and healing periods
During the soft tissue healing period of 23 weeks,
chemical plaque control with chlorhexidine-diglu-
conate (0.12%) is recommended. Mechanical
toothbrushing is abandoned in the surgical sites
for at least 2 weeks. Follow-up visits are scheduled
after 7, 14 and 21 days with clinical examination
and wound cleaning. The sutures are removed after
710 days. The healing caps should be exchanged
when really necessary at the earliest after 3
weeks.
The bone healing period for ITI implants with
a TPS surface has progressed sufciently after 3
4 months, as outlined in chapter 3, allowing the
insertion of the appropriate abutment and the
initiation of the prosthetic treatment. During the
bone healing period, functional loading of the in-
serted implant by provisionals such as partial den-
tures should be avoided. The status of the inte-
grated implant is evaluated by clinical examination
and a periapical radiograph.
As already mentioned in chapter 3, the utiliza-
tion of SLA implants allows a further reduction of
Buser & von Arx
88
Surgical procedures in partially edentulous patients
Fig. 5.5 Text, see next page.
89
Buser & von Arx
the healing period. An ongoing multicenter study
has successfully tested a healing period of 6 weeks
for implant sites with normal bone density (class
IIII) in fully and partially edentulous patients.
The preliminary results are promising, with success
rates exceeding 98% at the completion of the heal-
ing period, and will be published in the near future
(Cochran et al. 2001). The surgical procedures in
non-esthetic sites are demonstrated with four case
reports (Figs 5.55.8).
Implant placement in esthetic sites
General remarks
Esthetic sites for implant therapy are primarily
located in the anterior maxilla, including the rst
premolar sites. Main indications are single-tooth
replacement with implant-borne crowns and the
rehabilitation of extended edentulous spaces with
implant-supported multiple crowns or a FPD
(Table 5.3). The primary treatment goal is the re-
establishment of esthetics and function. These in-
dications are demanding for the implant surgeon,
since anatomical and surgical aspects are at least
as important for a satisfying treatment outcome
as prosthetic and technical aspects. The details of
prosthetic treatment planning and therapy in es-
thetic sites are outlined in chapter 8. The following
section will discuss the surgical aspects of how es-
thetically pleasing implant restorations can be
achieved with ITI implants on a predictable level.
The surgical aspects important for optimizing
esthetic implant restorations include (a) implant
insertion in an optimal three-dimensional position
(restoration-driven implant placement, Gar-
ber & Belser 1995), and (b) the achievement and
maintenance of esthetic soft tissue contours (Table
5.4). A correct three-dimensional implant position
includes a correct vertical location of the implant
with a subgingivally located implant shoulder to
avoid a visible cervical metal margin. In cases with
Fig. 5.5. a. Occlusal view of a distal extension situation in the left mandible. b. Status following a midcrestal incision and elevation
of two full-thickness aps. The smoothened alveolar crest is sufcient in width for a standard implant placement. c. After the
implant position is marked with a round bur, the rst bone preparation is made with spiral drill .1 ( 2.2 mm). d. The bone
preparation is increased with the spiral drill .2 ( 2.8 mm). e. The entrance of the bony implant bed is further opened up with the
small prole drill. f. The nal preparation is made with the spiral drill .3 ( 3.5 mm) to a sink depth of approximately 10.5 mm.
g. The occlusal view demonstrates the three bony implant beds with intact buccal and lingual bone walls. h. Due to the medium
bone density (class IIIII), tapping is only performed in the coronal portion of the implant bed. i. The placement of the SLA
implant is performed with the insertion device and the surgical adapter at 15 rpm. The microrough SLA surface is inserted slightly
below the bone crest on the approximal aspects. j. 3 mm healing caps are inserted to extend above the soft tissue level. k. A tension-
free and precise soft tissue adaptation is followed by wound closure with ne interrupted sutures (40 or 50). l. The clinical status
at day 7 showes a normal soft tissue healing. The sutures can be removed. m. The healing period is completed at 6 weeks following
implant placement. Note the excellent soft tissue healing around the 3 SLA implants. n. Conical abutments are inserted at 35 Ncm
to initiate the restoration with a provisional FPD. o. Periapical radiograph at 3 months following functional load with a provisional
restoration. The bone crest levels are excellent. p. Periapical radiograph at 12 months demonstrating the nal ceramometal restora-
tion and stable bone crest levels.
90
a high lip line, a visible metal margin is unaccept-
able nowadays and represents an esthetic failure of
implant therapy. Thus, ITI implants are utilized as
submerged implants in esthetic sites by inserting
them approximately 2 mm deeper into the hard
and soft tissues when compared to standard non-
esthetic implant sites (Buser & Belser 1995). The
deeper placement of ITI implants into the bone
leads to an increased crestal bone resorption, as
demonstrated in experimental and clinical studies
(Hammerle et al. 1996; Hermann et al. 1997). The
latter study in the canine mandible clearly demon-
strated that the vertical position of the implant
shoulder with its microgap at the implant-abut-
ment connection has a signicant impact on crestal
bone resorption. A distance of 1.5 and 2.0 mm be-
tween the rst bone-implant contact and the
microgap at the implant shoulder has been consist-
ently observed. These dimensions seem to be quite
constant and are part of a biologic width observed
not only around natural teeth (Gargiulo et al.
1961), but also around dental implants (Cochran
et al. 1997). Hence, the deeper an implant is in-
serted into the bone, the more bone will be re-
sorbed for a submerged implant following the sec-
ond-stage procedure with abutment connection.
This bone resorption is not a pathological con-
dition but a physiological reaction to the implant
placement. In order to limit the amount of bone
resorption, esthetic plus ITI implants are rec-
ommended for these indications, since surface
properties also inuence the bone reaction follow-
ing implant placement (Buser et al. 1992a; Her-
mann et al. 1997). Esthetic plus implants have a
sprayed-up TPS surface, and the height of the
smoothly machined neck is reduced to 1.8 mm.
Therefore, it is recommended that the deeper im-
plant placement should be done according to the
principle as much as necessary, as little as poss-
ible. An extremely deep implant placement has
clear disadvantages, such as an unfavorable lever-
Surgical procedures in partially edentulous patients
Fig. 5.6. a. Distal extension situation with two ITI implants placed in the premolar
sites. The patient wants to have a third implant in the rst molar site. b. Clinical
status following implant placement and suturing of the mesial papilla. The wound
margins are carefully adapted to the healing cap without gingivectomy. Two small
relieving incisions are made to allow the rotation of the wound margins distally to
the implant. c. The mucosa margins are rotated and sutured with an interrupted
suture. d. Clinical status 3 months following placement of the ITI implant with a
TPS surface.
age arm between clinical crown and implant
length, an increased probing depth in approximal
areas (5 mm), a microgap inaccessible for hy-
giene, and increased crestal bone resorption, as
outlined above.
The correct implant placement in orofacial posi-
tion signicantly inuences the prole of the super-
structure. In particular, the point of emergence
from the soft tissues determines the nal cervical
contour of the restoration. Generally, a proper
emergence prole is desirable, both for esthetic and
hygienic reasons. Therefore, the vestibular aspect
91
of the implant shoulder has to emerge as buccally
as do adjacent natural teeth. In addition, a buccal
bone wall of at least 1 mm thickness should be
present when the implant is inserted. A proper oro-
facial implant position is difcult to obtain when
a buccal atrophy of the alveolar crest is present. In
such cases, bone reconstructive surgery is needed
to locally augment the alveolar process, either
prior to or simultaneously with implant placement
(Buser et al. 1992b, 1996; von Arx et al. 1998; von
Arx & Kurt 1998).
The third aspect to be mentioned in this context
Buser & von Arx
Fig. 5.7. a. Distal extension situation in the right mandible.
Status following preparation of two implant beds. Note the in-
tact buccal and lingual bone walls of sufcient thickness. b. The
buccal ap was released with a distal incision of the periosteum
to allow a precise and tension-free adaptation to the healing
caps. With this technique, no gingivectomy is necessary to
achieve a close adaptation of the mucosa. c. Clinical status at
6 weeks with an excellent soft tissue healing. The two SLA im-
plants are ready for prosthetic restoration. d. Two conical abut-
ments are inserted at 35 Ncm for a cemented implant restora-
tion. e. Clinical status at the 2-year follow-up visit. The peri-
implant soft tissues show no clinical signs of inammation. f.
Periapical radiograph at 2 years indicates stable bone crest
levels around both SLA implants.
is the implant axis, which determines the access for
the occlusal screw. Unfortunately, a discrepancy
between the potential implant axis and the clinical
crown axis is often encountered in the anterior
maxilla due to the anatomy of the alveolar process.
Therefore, the use of a horizontal screw path for a
92
screw-retained single crown is recommended
(Belser & Buser 1997).
The achievement and maintenance of esthetic buc-
cal soft tissues is of utmost importance for an es-
thetic implant restoration. Esthetic soft tissue con-
tours include a harmoniously scalloped gingival
Surgical procedures in partially edentulous patients
Fig. 5.8. a. Distal extension situation in the left maxilla. Status 8 months following a sinus grafting procedure. Three SLA implants
can be inserted. b. Small relieving incisions are applied on the buccal wound margin to allow small rotational aps to be placed in
the interimplant spaces. c. The small aps are rotated. The margins are stabilized with interrupted sutures. d. Clinical status 1 week
following implant placement. The wound shows some signs of secondary wound healing in the interimplant spaces. The sutures can
be removed. e. At 2 weeks, wound healing has progressed further. f. At 8 weeks, the clinical status shows excellent peri-implant soft
tissue conditions. The SLA implants are ready for provisional restoration with three splinted crowns.
line, the avoidance of abrupt vertical changes or
differences in clinical crown length between ad-
jacent teeth, a convex buccal mucosa of sufcient
thickness, and distinct papillae (Belser et al. 1996b;
Belser et al. 1998). Thus, careful soft tissue han-
dling by the implant surgeon is important, includ-
ing an appropriate incision and wound closure
technique. In particular, a submerged implant
placement is recommended in esthetic sites. In ad-
dition, soft tissue grafting is quite often necessary
93
in esthetic sites to improve the esthetic treatment
outcome. Stable soft tissue conditions can primar-
ily be achieved with the presence of a buccal bone
wall of at least 1 mm at the time of implant place-
ment to facilitate bony support of the buccal soft
tissues. Thus, no compromise should be made by
the implant surgeon concerning a sufcient crest
width (implant diameter 2 mm) when the im-
plant is inserted. There is clinical evidence that the
lack of this bone wall can cause soft tissue prob-
Buser & von Arx
94
Surgical procedures in partially edentulous patients
Fig. 5.9. Text, see next page.
95
Buser & von Arx
Fig. 5.9. a. Single-tooth gaps in the anterior maxilla due to a
traumatic tooth loss. b. The implant surgery is initiated with a
palatal incision for a full-thickness ap. c. The ap is elevated
with divergent relieving incisions. The bone crest is smoothened
with a bone scalloping procedure. Approximal bone is not
touched at all. d. Status following preparation of the implant
bed. Note the intact buccal bone wall of at least 1 mm thickness
to serve as soft tissue support. This buccal bone is crucial for
a stable esthetic treatment outcome. e. The implant is inserted
to a correct vertical level. The implant shoulder is located
slightly apical to the cej-level of adjacent teeth. f. The orofacial
position of the implant shoulder is ideal. The point of emer-
gence is comparable with those of adjacent teeth. g. A healing
cap with a buccal bevel is inserted. h. A free connective tissue
graft is harvested in the left palate to improve the soft tissue
thickness and contour on the buccal aspect of the implant. i.
The graft is placed in situ to check the shape and the position.
j. The graft is sutured to the buccal ap to ensure correct posi-
tion and an intimate contact with the vascularized buccal ap.
k. A tension-free wound closure is achieved following the in-
cision of the periosteum. The wound margins are secured with
interrupted sutures (40 or 50). l. The existing partial denture
is shortened and put in place. m. Clinical status at 8 weeks.
Note the convex soft tissues with an excellent contour and
color. The site will now be reopened to gain access to the inte-
grated implant. n. Status following placement of a long healing cap to congure the soft tissue channel to the implant shoulder. o.
The peri-implant soft tissues are nicely healed two weeks following gingivectomy. p. Restoration with a provisional crown to get an
optimal soft tissue conditioning. q. 3 months later, the peri-implant sulcus has been nicely formed. r. Restoration with a screw-
retained ceramometal crown. s. Esthetic treatment outcome. t. The periapical radiograph at 3 years indicates a stable bone crest
level with a steady-state situation.
lems such as gingival recessions or an increased
failure rate for dental implants (Lekholm et al.
1986; Dietrich et al. 1993). In addition, appropri-
ate oral hygiene has to be performed by the patient
to establish and maintain a healthy peri-implant
mucosa.
Preoperative examination in esthetic sites
Clinical evaluation
During preoperative examination, the implant sur-
96
geon must primarily evaluate the anatomical as-
pects of the potential implant site. This includes a
variety of parameters such as the shape and width
of the bone crest, the absence or presence of a buc-
cal undercut, the status of neighboring teeth
(caries lesions, existing llings or crowns, discol-
orations, etc.), the mesio-distal width of the eden-
tulous space, the intermaxillary situation (a deep
bite can cause problems), the absence or presence
of diastemas, the thickness and contour of buccal
soft tissues, the position of papillae, the quality of
Surgical procedures in partially edentulous patients
Table 5.3. Indications in esthetic sites
O Single-tooth gaps in the anterior maxilla
O Extended edentulous spaces in the anterior maxilla
Table 5.4. Surgical aspects to optimize implant esthetics
O Optimal three-dimensional implant position (Restoration-driven implant place-
ment)
Subgingival implant shoulder
Correct orofacial implant position
Appropriate implant axis
O Achievement and maintenance of esthetic soft tissue contours
Harmoniously scalloped gingival line
Intact papillae
Convex buccal soft tissues of sufcient thickness
the gingival tissues (phenotype I or II), and the
location of the smile line (high vs low lip line). In
single-tooth gaps, a minimum mesio-distal width
of 6.57.0 mm is necessary for the placement of a
standard screw implant (S 4.1), whereas a narrow-
neck implant (NN 3.3) requires a minimal width
of 5 mm.
Radiologic evaluation
In standard cases, a periapical radiograph and/or
a panoramic radiograph is sufcient. Tomograms
or CT scans are only indicated in special situ-
ations, such as to evaluate the need for bone aug-
mentation procedures in patients presenting with
bone defects.
Selection of implant type and length
As already outlined in chapter 3, the longest poss-
ible implant is selected up to a maximum of 12 mm
(14 mm sink depth). The implant of rst choice
is the standard screw implant (S 4.1). The narrow-
neck implant (NN 3.3) is often used for the single-
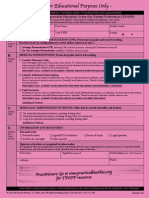
Table 5.5. Surgical procedure for implant placement in esthetic sites (new protocol for ITI implants with SLA surface)
O Crestal incision, slightly palatal
O Buccal relieving incisions only if necessary
O Crest attening as bone scalloping procedure; bone in the approximal area of adjacent teeth is not touched!
O Surgical guides are recommended in cases with multiple missing teeth
O Preparation of implant bed with spiral drills with increasing diameter
O Sink depthimplant length 2 mm
O Use of a prole drill to open the entrance of the bone cavity to allow a deeper implant insertion (approximately 2 mm deeper than in standard sites)
O Tapping in sites with normal bone density, no tapping in sites with spongy bone
O Implant insertion with the premounted insertion device using a slow speed of approximately 15 rpm
O Tapping and implant insertion can be done with a hand ratchet or with an adapter attached to a special contra-angle handpiece
O Utilization of esthetic healing caps with a buccal bevel
O In case of a thin buccal mucosa and/or a concave buccal soft tissue contour, the utilization of a connective tissue graft is recommended
O Precise positioning of the buccal wound margin, in particular of the papillae
O Primary wound closure with tension-free suturing to achieve a submerged healing of the implant
O Reopening procedure with a mucosaplasty after 6 weeks to gain access to the implant
O Initiation of prosthetic treatment at 8 weeks
97
tooth replacement of missing lateral incisors if the
mesio-distal width of the gap is limited (5.06.5
mm). In general, esthetic plus implants are pre-
dominantly used with a sprayed-up TPS surface to
limit postoperative bone resorption in the crestal
area due to the deeper implant placement, as dis-
cussed in detail above.
Surgical procedure in esthetic sites
The surgical procedure used for implant placement
in esthetic sites is summarized in Table 5.5. Follow-
ing local anesthesia, the mucosa is opened with a
crestal incision located slightly on the palatal as-
pect. This assures a sufcient vascularity of the
buccal ap in the papillary area. The incision is
extended through the sulcus of adjacent teeth to
the buccal and palatal aspect of the alveolar crest.
Buccal relieving incisions are only made when
necessary. Subsequently, the buccal and palatal
mucoperiosteal aps are elevated with a ne tissue
elevator to guarantee low-trauma soft tissue han-
dling. This is followed by an intrasurgical site
analysis to evaluate the crest width and the buccal
aspect of the alveolar crest. As outlined in chapter
3, a minimal crest width of 5.5 mm is required for
the placement of a standard screw implant. A crest
attening as bone scalloping procedure is rec-
ommended, since this facilitates easier and more
precise preparation of the implant bed. The sur-
geon should not remove any bone in the approxi-
mal area of adjacent teeth, since this bone is im-
portant for the support and maintenance of the
papillae. The precise position of the implant is
marked with small round burs. The utilization of
surgical guides is recommended in the case of
multiple missing teeth, whereas landmarks of ad-
jacent teeth provide sufcient guidance in most
cases with a single-tooth gap. The preparation of
Buser & von Arx
the implant bed is carried out with standard spiral
drills of increasing diameter (2.2 mm, 2.8 mm and
3.5 mm). This technique reduces the trauma to the
bone tissue, and gives the surgeon a chance to
change the direction of the implant axis when
necessary between the different drill steps. As al-
ready outlined above, a deeper implant placement
is recommended in esthetic sites. As a rule of
thumb, the implants are inserted approximately 2
mm deeper than in standard sites. Hence, the im-
plant bed is prepared to 14 mm if a 12 mm implant
is planned to be inserted. As a consequence of an
esthetic implant placement, the entrance of the
bone cavity has to be prepared with the prole drill
to allow a deeper implant insertion. In addition,
Esthetic plus implants are most often utilized to
limit the amount of bone resorption in the crestal
area. During the different steps of the bone prep-
aration, the availability of different depth gauges
helps the surgeon control the future implant posi-
tion in a horizontal and vertical direction as well
as the implant axis. Prior to implant placement,
the tapping of the thread is done in all sites with
normal bone density (class IIII). In cases with ex-
tremely spongy bone (class IV), no tapping should
be carried out, in order to improve the primary
stability of the implant. Tapping and implant in-
sertion are done either with an adapter attached to
a special contra-angle hand-piece (at 15 rpm) or
with the hand ratchet. Implant placement has re-
cently been further simplied, since the new ITI
insertion device is premounted onto the implant,
allowing a non-touch handling of the implant from
the sterile ampoule.
Following implant placement, the horizontal
and vertical position of the implant shoulder as
well as the primary stability of the implant are
carefully checked. The next step is to select the ap-
propriate healing cap. An esthetic healing cap with
a buccal bevel is recommended to reduce the vol-
ume of the cap in the critical zone of the buccal
soft tissues. This cap is available in two heights (2
and 3.5 mm) and has the clinical advantages that
it will (a) fully cover the implant shoulder, (b) sup-
port the soft tissues in the approximal area, and
(c) preshape a part of the transmucosal soft tissue
tunnel to the implant already during the initial
healing period.
Furthermore, in the case of a thin buccal mu-
cosa and/or a concave buccal soft tissue contour,
the soft tissues are corrected with a grafting tech-
nique at the time of implant placement. This surgi-
cal concept is straightforward and eliminates an
open-ap procedure at the second-stage surgery. In
routine cases, a connective tissue (CT) graft is suf-
cient to improve the thickness and contour of the
buccal mucosa. These grafts are easily harvested in
98
the premolar area of the palate. With buccal reliev-
ing incisions, the CT graft is sutured to the perios-
teum of the mucoperiosteal ap to avoid displace-
ment of the graft during wound closure.
Prior to the completion of the surgical pro-
cedure, the buccal ap, and in particular the papil-
lae, is precisely repositioned. The surgeon should
aim for a precise and tension-free primary wound
closure to allow submerged implant healing on top
of the applied esthetic healing cap. Fine atraumatic
suture material (40 or 50) is recommended. Fol-
lowing surgery, a periapical radiograph is taken to
examine the position and direction of the inserted
implant and its relationship to the roots of ad-
jacent teeth. The existing provisional partial den-
ture is shortened in the edentulous area to avoid
precontact of the prosthesis with the soft tissues
during initial wound healing.
Postoperative treatment
Postsurgical treatment in an esthetic site does not
differ from that in non-esthetic sites. Chemical
plaque control with chlorhexidine-digluconate
(0.12%) is recommended in the rst 23 weeks fol-
lowing implant placement. Suture removal is
scheduled after 710 days, and further clinical ex-
ams are made on days 14 and 21. At day 14, in-
struction on proper hygiene is given to facilitate an
optimal wound healing period.
Reopening with a mucosaplasty
After 810 weeks of healing, a local mucosaplasty
is performed to uncover the integrated implant.
This is done with a 12d blade to gain access to the
implant shoulder. Electrosurgery is contraindi-
cated. The esthetic healing cap is replaced by a
long extension healing cap (3 mm or 4.5 mm) to
nally shape the transmucosal soft tissue tunnel to
the implant shoulder. The soft tissue margins
should not be compressed too much, which is indi-
cated by a severe and lasting blanching of the mu-
cosa.
Abutment insertion
After 12 weeks of healing, the abutment is inserted
and the impression is taken to initiate the pros-
thetic treatment. In standard cases, the octabut-
ment is selected for a screw-retained restoration
(see chapters 6 and 8). The status of the integrated
implant is evaluated by clinical examination and
a radiograph. Usually, implant loading is initiated
after 3 months of healing.
As already mentioned above, the introduction of
the new SLA surface offers a further reduction of
Surgical procedures in partially edentulous patients
the healing period to six weeks in sites with normal
bone density (class IIII). In esthetic sites, how-
ever, the time for soft tissue healing and soft tissue
maturation following implant placement and the
reopening procedure has to be respected to achieve
stable esthetic soft tissues. The reopening pro-
cedure is scheduled at 6 weeks of healing to gain
access to the integrated SLA implant. At 8 weeks,
functional loading is initiated with a provisional,
screw-retained crown.
The surgical procedure is demonstrated with a
case report (Fig. 5.9).
References
Babbush, C., Kent, J.N. & Misiek, D.J. (1986) Titanium
plasma-sprayed (TPS) screw implants for the reconstruction
of the edentulous mandible. Journal of Oral and Maxillo-
facial Surgery 44: 274282.
Belser, U.C. & Buser, D. (1997) Fixed implant restorations. The
prosthetic concept of the ITI Dental Implant System. Video-
tape. Berlin, Chicago: Quintessence Publishing.
Belser, U., Mericske, R., Buser, D., Bernard, J.P., Hess, D. &
Martinet, J.P. (1996a) Preoperative diagnosis and treatment
planning. In: Schroeder, A., Sutter, F., Buser, D., Krekeler,
G., eds. Oral Implantology. Basics, ITI Dental Implant Sys-
tem, 2nd Edition. pp. 231255. New York: Thieme Medical
Publishers Inc.
Belser, U.C., Bernard, J.P. & Buser, D. (1996b) Implant-sup-
ported restorations in the anterior region: prosthetic con-
siderations. Practical Periodontics and Aesthetic Dentistry 8:
875883.
Belser, U.C., Buser, D., Hess, D., Schmid, B., Bernard, J.P. &
Lang, N.P. (1998) Esthetic implant restorations in partially
edentulous patientsa critical appraisal. In: Lang, N.P., ed.
Periodontology 2000: Implant dentistry. Vol. 17, 132150.
Bernard, J.P., Belser, U.C., Szmukler, S., Martinet, J.P., Attieh,
A. & Saad, P.J. (1995) Intere`t de lutilisation dimplants ITI
de faible longueur dans les secteurs posterieurs: resultats
dune etude clinique de 3 ans. Medicine buccale Chirurgie
buccale 1: 1118.
Bragger, U., Buser, D. & Lang, N.P. (1990) Implantat-getragene
Kronen und Bru cken. Indikationen, Therapieplanung und
kronen-bru ckenprothetische Aspekte. Schweizer Monatssch-
rift fur Zahnmedizin 100: 731738.
Buser, D. & Belser, U.C. (1995) Esthetic implant dentistry.
Single tooth replacement with ITI Dental Implants. Video-
tape. Berlin, Chicago: Quintessence Publishing.
Buser, D., Schroeder, A., Sutter, F. & Lang, N.P. (1988) The
new concept of ITI hollow-cylinder and hollow-screw im-
plants: Part 2. Clinical aspects, indications, and early clinical
results. International Journal of Oral and Maxillofacial Im-
plants 3: 173181.
Buser, D., Weber, H.P. & Bragger, U. (1990) The treatment of
partially edentulous patients with ITI hollow-screw im-
plants: presurgical evaluation and surgical procedures. In-
ternational Journal of Oral and Maxillofacial Implants 5:
165174.
Buser, D., Weber, H.P., Donath, K., Fiorellini, J.P., Paquette,
D.W. & Williams, R.C. (1992a) Soft tissue reactions to non-
submerged unloaded titanium implant in beagle dogs.
Journal of Periodontology 63: 225235.
Buser, D., Hirt, H.P., Dula, K. & Berthold, H. (1992b) Mem-
brantechnik/Orale Implantologie. Gleichzeitige Anwendung
von Membranen bei Implantaten mit periimplantaren Kno-
chendefekten. Schweizer Monatsschrift fur Zahnmedizin 102:
14911501.
99
Buser, D., Dula, K., Hirt, H.P. & Schenk, R.K. (1996) Lateral
ridge augmentation using autografts and barrier mem-
branes: a clinical study with 40 partially edentulous patients.
Journal of Oral and Maxillofacial Surgery 54: 420432.
Buser, D., Mericske-Stern, R., Bernard, J.P., Behneke, A.,
Behneke, N., Hirt, H.P., Belser, U.C. & Lang, N.P. (1997)
Long-term evaluation of non-submerged ITI implants. Part
1: 8-year life table analysis of a prospective multi-center
study with 2359 implants. Clinical Oral Implants Research
8: 161172.
Buser, D., Mericske-Stern, R., Dula, K. & Lang, N.P. (1999a)
Clinical experience with one-stage, non-submerged titanium
dental implants. Advances of Dental Research 13: 153.
Buser, D., Nydegger, T., Oxland, T., Cochran, D.L., Schenk,
R.K., Hirt, H.P., Snetivy, D. & Nolte, L.P. (1999b) The inter-
face shear strength of titanium implants with a sandblasted
and acid-etched surface. A biomechanical study in the max-
illa of miniature pigs. Journal of Biomedical Materials Re-
search 45: 7583.
Chappuis, V. (2000) Implantat-Bohrer im Langzeittest. In-vitro
Studie mit den gebrauchlichsten Mehrfachbohrern verschied-
ener Hersteller. Thesis, Medical Faculty, University of
Berne.
Cochran, D.L., Hermann, J.S., Schenk, R.K., Higginbottom,
F.L. & Buser, D. (1997) Biologic width dimensions around
titanium implants. A histometric study on loaded, non-sub-
merged implants in the canine mandible. Journal of Period-
ontology 68: 186198.
Cochran, D.L., Buser, D., ten Bruggenkate, C.M., Weingart, D.,
Taylor, T.M., Bernard, J.P., Peters, F. & Simpson, J.P. (2001)
The use of shortened healing times on ITI implants with a
sandblasted and acid-etched (SLA) surface. Early results
from clinical trials on ITI SLA implants. Clinical Oral Im-
plants Research (Submitted).
Dietrich, U., Lippold, R., Dirmeier, T., Behneke, N. & Wagner,
W. (1993) Statistische Ergebnisse zur Implantatprognose am
Beispiel von 2017 IMZ-Implantaten unterschiedlicher Indi-
kation der letzten 13 Jahre. Zeitschrift fur Zahnarztliche Im-
plantologie 9: 918.
Dula, K., Mini, R., van der Stelt, P.F., Lambrecht, J.T., Schnee-
berger, P. & Buser, D. (1996) Hypothetical mortality risk
associated with spiral computed tomography of the maxilla
and mandible. European Journal of Oral Science 104: 503
510.
Garber, D.A. & Belser, U.C. (1995) Restoration-driven implant
placement with restoration-generated site development.
Compendium of Continuing Education in Dentistry 16: 796
804.
Gargiulo, A.W., Wentz, F.M. & Orban, B. (1961) Dimensions
and relations of the dentogingival junction in humans.
Journal of Periodontology 32: 261267.
Hammerle, C.H.F., Bragger, U., Bu rgin, W. & Lang, N.P. (1996)
The effect of subcrestal placement of the polished surface of
ITI implants on marginal soft and hard tissues. Clinical Oral
Implants Research 7: 111119.
Hermann, J., Cochran, D.L., Nummikowski, P.V. & Buser, D.
(1997) Crestal bone changes around titanium implants. A
radiographic evaluation of unloaded nonsubmerged and
submerged implants in the canine mandible. Journal of Peri-
odontology 68: 11171130.
Higuchi, K.W., Folmer, T. & Kultje, C. (1995) Implant survival
rates in partially edentulous patients: a 3-year prospective
multi-center study. Journal of Oral and Maxillofacial
Surgery 53: 264268.
Kayser, A.F. (1989) The shortened dental arch: a therapeutic
concept in reduced dentitions and certain high risk patients.
International Journal of Periodontics and Restorative Den-
tistry 9: 427449.
Krekeler, G., Schilli, W. & Geiger, H. (1990) Das TPS-Im-
Buser & von Arx
plantat, ein zuverlassiges Retentionselement. Zeitschrift fur
Zahnarztliche Implantologie 6: 229234.
Ledermann, P.D. (1979) Stegprothetische Versorgung des
zahnlosen Unterkiefers mit Hilfe von plasmabeschichteten
Titanschraubenimplantaten. Deutsche Zahnarztliche
Zeitschrift 34: 907911.
Ledermann, P.D. (1984) Das TPS-Schraubenimplantat nach sie-
benjahriger Anwendung. Quintessenz 35: 111.
Ledermann, P.D. (1996) U
ber 20 jahrige Erfahrung mit der so-
fortigen funktionellen Belastung von Implantatstegen in der
regio interforaminalis. Zeitschrift fur Zahnarztliche Im-
plantologie 12: 123136.
Lekholm, U., Adell, R., Lindhe, J., Brnemark, P.I., Eriksson,
B., Rockler, B., Lindvall, A.M. & Yoneyama, T. (1986) Mar-
ginal tissue reactions at osseointegrated titanium xtures.
International Journal of Oral and Maxillofacial Surgery 15:
5361.
Rangert, B.R., Sullivan, R. & Jemt, T.M. (1997) Load factor
control for implants in the posterior partially edentulous
segment. International Journal of Oral and Maxillofacial Im-
plants 12: 360370.
100
Sutter, F., Schroeder, A. & Buser, D. (1988) The new concept
of ITI hollow-cylinder and hollow-screw implants. Part 1.
Engineering and design. International Journal of Oral and
Maxillofacial Implants 3: 161172.
Sutter, F., Weber, H.P., Sorensen, J. & Belser, U.C. (1993) The
new restorative concept of the ITI Dental Implant System:
design and engineering. International Journal of Periodontics
and Restorative Dentistry 13: 409431.
ten Bruggenkate, C.M., Muller, K. & Oosterbeek, H.S. (1990)
Clinical evaluation of the ITI (F-type) hollow cylinder im-
plant. Oral Surgery Oral Medicine Oral Pathology 70: 693
697.
von Arx, T. & Kurt, B. (1998) Implant placement and simul-
taneous peri-implant bone grafting using a micro titanium
mesh for graft stabilization. International Journal of Peri-
odontics and Restorative Dentistry 18: 117127.
von Arx, T., Wallkamm, B. & Hardt, N. (1998) Localized ridge
augmentation using a micro titanium mesh: a report on 27
implants followed from 1 to 3 years after functional loading.
Clinical Oral Implants Research 9: 123130.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Activation and Operational Planning - Ensuring A Succesful TransitionDocument6 pagesActivation and Operational Planning - Ensuring A Succesful TransitionManiqueAbeyratneNo ratings yet
- Family Nursing Care Plan and Teaching PlanDocument1 pageFamily Nursing Care Plan and Teaching PlanJerzene Mae100% (1)
- Supplementary File Survey Question Response OptionsDocument3 pagesSupplementary File Survey Question Response OptionsEliza DNNo ratings yet
- Interdisciplinary Culture FinalDocument3 pagesInterdisciplinary Culture FinalEliza DNNo ratings yet
- 2008 NOHC - JPHDSupplementDocument62 pages2008 NOHC - JPHDSupplementEliza DNNo ratings yet
- Optimal Management of Collagenous Colitis A Review 021016Document9 pagesOptimal Management of Collagenous Colitis A Review 021016Eliza DNNo ratings yet
- Hansen Review CortisolDocument12 pagesHansen Review CortisolEliza DNNo ratings yet
- Erosion SalivaDocument8 pagesErosion SalivaEliza DNNo ratings yet
- !!! Tooth Wear Indices ReviewDocument6 pages!!! Tooth Wear Indices ReviewEliza DNNo ratings yet
- Q2 2023 Digital Health Report PreviewDocument12 pagesQ2 2023 Digital Health Report PreviewNointingNo ratings yet
- Essay About HealthDocument4 pagesEssay About HealthCanNo ratings yet
- Dr. Korkmaz SayinsuDocument8 pagesDr. Korkmaz SayinsuakordtrainingNo ratings yet
- Jurnal Komunitas DMDocument10 pagesJurnal Komunitas DMTria WulandaryNo ratings yet
- Writing A Health Policy Brief With OutlineDocument14 pagesWriting A Health Policy Brief With OutlineyandhiasNo ratings yet
- Breathing Techniques Associated With Improved Health OutcomesDocument34 pagesBreathing Techniques Associated With Improved Health OutcomesJasleen KaurNo ratings yet
- Tourism and Hospitality IndustryDocument12 pagesTourism and Hospitality IndustryIqbal singh100% (1)
- Development and Maintenance of Standards and Accreditation ofDocument38 pagesDevelopment and Maintenance of Standards and Accreditation ofsrimalathi100% (1)
- Type 1 Diabetes Self-Care Manual - ADADocument2 pagesType 1 Diabetes Self-Care Manual - ADAKarthic V.ManiNo ratings yet
- 12 TH JC PDF - SindhuDocument9 pages12 TH JC PDF - SindhuDadi SindhuNo ratings yet
- 1.-IMI - White Papers BookDocument27 pages1.-IMI - White Papers BookyeimyNo ratings yet
- Pharmacy Directory FLORIDADocument180 pagesPharmacy Directory FLORIDAKrupa Patel AminNo ratings yet
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary DetailsamzadsmartNo ratings yet
- 2022 Organ Imaging Review ProgramDocument8 pages2022 Organ Imaging Review ProgramU of T MedicineNo ratings yet
- Sana Insurance PDFDocument6 pagesSana Insurance PDFDameer SanaNo ratings yet
- IP Dental and Pharmacy Books Catalogue 2022Document2 pagesIP Dental and Pharmacy Books Catalogue 2022vmags822No ratings yet
- Missouri Transportable Physician Orders For Patient Preferences Tpopp FormDocument2 pagesMissouri Transportable Physician Orders For Patient Preferences Tpopp FormitargetingNo ratings yet
- Course DetailsDocument7 pagesCourse DetailsGh8jfyjnNo ratings yet
- List of Doctors Parans Update v3.0Document9 pagesList of Doctors Parans Update v3.0Franz CantaraNo ratings yet
- Nursing ManagementDocument61 pagesNursing ManagementRahul RavishankarNo ratings yet
- Ericson Insurance TPA Pvt. LTDDocument1 pageEricson Insurance TPA Pvt. LTDamit patelNo ratings yet
- QualityAssuranceProgram BenchbookDocument66 pagesQualityAssuranceProgram BenchbookRhod Bernaldez EstaNo ratings yet
- Hospital Timplet - 2Document142 pagesHospital Timplet - 2Qairul AzmanNo ratings yet
- CAPMC Brochure2Document2 pagesCAPMC Brochure2Mhmd IrakyNo ratings yet
- Alan E. KazdinDocument423 pagesAlan E. KazdinSalman Baig100% (6)
- Phoenix Sepsis ScoreDocument3 pagesPhoenix Sepsis ScoreNur Amaliah idrusNo ratings yet
- Central Government Health Scheme (CGHS)Document12 pagesCentral Government Health Scheme (CGHS)upsc4all67% (3)
- NBHS4133 Clinical Assessment in Healthcare - SMay19 (Bookmark)Document203 pagesNBHS4133 Clinical Assessment in Healthcare - SMay19 (Bookmark)Klinik 1 Malaysia SegambutNo ratings yet