Professional Documents
Culture Documents
Diphtheria
Diphtheria
Uploaded by
Lura Sativa0 ratings0% found this document useful (0 votes)
18 views22 pagesdiphteri
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentdiphteri
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
18 views22 pagesDiphtheria
Diphtheria
Uploaded by
Lura Sativadiphteri
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 22
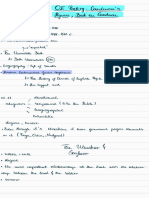
Diphtheria
Is an acute infectious disease of the childhood
characterized by local inflammation of the
epithelial surface , formation of a membrane ,
and severe toxemia
Epidemiology : -
Age groups : Pre school age children
Occurs in the autumn and winter months.
Caused by ---- Gram positive bacilli,
Corynebacterium diphtheria
Cont ..
Source : -
- secretions and discharge from an infected
person or carrier
Human are chief reservoirs
Mode of transmission : -
Contact or through droplets of secretion
Portal of entry :
Respiratory tract
May enter through the conjuntiva or skin
wound
Risk factors
1. Poor nutrition.
2. Outbreak in the community.
3. Crowded or unsanitary living conditions.
4. Low vaccine coverage among infants and
children.
5. Lack of mass immunization programmes
amongst children and adults at high risk.
6. Insufficient information for the general public on
dangers of the disease and the benefits of
immunization.
7. Lack of vaccines in many areas.
Pathogenesis
Entry ------ the bacilli multiply locally in the throat and
elaborate a powerful exotoxin ----- produce local and
systemic symptoms.
Local lesions :
Exotoxin causes necrosis of the epithelial cells and
liberates serous and fibrinous material which forms a
grayish white pseudomembrane
The membrane bleeds on being dislodged
Surrounding tissue is inflamed and edematous
Cont
Systemic lesions :
Exotoxin affects the heart , kidney and CNS
Heart :
Myocardial fibers are degenerated and the
heart is dilated
Conduction disturbance
CNS : polyneuritis
Kidney : renal tubular necrosis
Clinical features
Incubation period : 2 5 days
Constitutional symptoms:
Onset : acute with fever ( 39 C ) , malaise ,
headache and loss of appetite
Child looks very sick and toxic
Delirium
Circulatory collapse ( myocarditis )
Local manifestation
Depend on the site of
lesion:
Nasal diphtheria :
Unilateral or bilateral
serosanguineous ( blood and
serous fluid ) discharge from
the nose
Excoriation of upper lip
Toxemia is minimal
Faucial diphtheria :
Redness and swelling over
fauces
Exudates on the tonsils
coalesces to form grayish
white pseudo membrane
Regional lymph nodes are
inflamed
Sore throat and
dysphagia
Fauces ( throat )
Fauces : - two pillars of mucous membrane.
Anterior : known as the palatoglossal arch and
Posterior : the palatopharyngeal arch
Between these two arches is the palatine tonsil.
Cont
Laryngotracheal diphtheria :
Membrane over the larynx results in
brassy ( hardness ) cough and
hoarse voice
Respiration ------- noisy
Suprasternal and subcostal
recession
Restlessness
Increasing respiratory effort
Use of accessory muscles
Unusual sites :
Conjunctiva and
skin
In the skin :
Ulcers ( tender )
Diagnosis
clinical history , examination and identification of
diphtheria bacilli from the site of lesion.
Culture
Albert`s staining
Fluorescent antibody technique
Schick Test
Schick test: It is an intradermal test,
the test is carried out by injecting
intradermally into the skin of
forearm 0.2 ml of diphtheria toxin,
while into the opposite arm is
injected as a control, the same
amount of toxin which has been
inactivated by heat.
Interpretation
Negative reaction: If a person had immunity to diphtheria,
no reaction will be observed on either arm.
Positive reaction: An area of in duration 10-15 mm in
diameter generally appears within 24-36 hours reaching
its maximum development by 4-7 days, the control arm
shows no change. The person is susceptible to diphtheria.
False positive reaction: A red flush develops in both arms,
the reaction fades very quickly, and disappears by 4
th
day.
This is an allergic type of reaction found in certain
individuals
Combined reaction: the control arm shows pseudo
positive reaction and the test arm is true +ve reaction,
susceptible and need vaccination
Differential diagnosis
Nasal diphtheria :
Foreign body in nose ,
Rhinorrhea
Laryngeal diphtheria :
Croup
Acute epiglottitis
Laryngotracheobronchitis
Peritonsillar abscess
Retropharyngeal abscess
Cont .
Faucial diphtheria :
Acute streptococcal membranous tonsillitis (
high grade fever , child less toxic )
Viral membranous tonsillitis :
high grade fever ,
WBC : normal or low ,
Antibiotic : no effects
Herpetic tonsillitis ( Gingivitis and stomatitis )
Infectious mononeucleosis :
Generalised rash and lymphadenopathy besides
oral mucosal lesions
Treatment
Principles :
Neutralization of free circulating toxin by
administration of antitoxin
Antibiotic to eradicate bacteria
Supportive and symptomatic therapy
Management of complication
Antitoxin
Diphtheria antitoxin :
Pharyngeal or laryngeal diphtheria of 48 hours
duration : 20,000 to 40,000 units.
Nasopharyngeal lesions : 40,000 60,000 units
Extensive disease of 3 or more days duration or
patient with swelling of neck : 80,000 120,000
units
Antitoxin may be repeated if the clinical
improvementis slower
Antibiotics
Penicillin :
Procaine penicilline ( 3 6 lac units IM at 12
hourly intervals till the patient is able to swallow )
Oral penicillin ( 125 250 mg qid )
Erythromycin ( 25 30 mg / kg / day ) for 14
days
Three negative cultures at 24 hours intervals
should be obtained before the patient is
declared free of the organism
Supportive and symptomatic therapy
Bed rest for 2 3 weeks ( to reduce cardiac
complications )
Antipyretics and sedative ( if required )
Monitor rate and rhythm of the heart
Management of complication
Respiratory obstruction :
Humidified oxygen
Tracheostomy
Myocarditis :
Fluids and salt restriction
Sedation and oxygen supply
Diuretics and digoxin
Neurological complications :
Palatal paralysis ( NG feeding )
Generalised weakness ( as polio )
Complications
Myocarditis :
Occurs towards the end of the first or beginning
of second week
Abdominal pain , vomiting , dyspnea ,
tachycardia
Neurological complications : ( Traid )
Palatal paralysis ( 2 weeks )
General polyneuritis ( 3 6 weeks )
Loss of accommodation ( 3 weeks )
Renal complications :
Oliguria and proteinuria indicate kidney
complications
Prevention
Vaccination: Immunisation with diphtheria toxoid,
combined with tetanus and pertussis toxoid (DTP
vaccine), should be given to all children at two,
three and four months of age. Booster doses are
given between the ages of 3 and 5 .
The child is given a further booster vaccine
before leaving school and is then considered to
be protected for a further 10 years (16 18
years).
Prognosis
Death may occur due to : -
Respiratory obstruction
Myocarditis
Respiratory paralysis
You might also like
- Core Values and Formalization As Determinants of Individual Behavior in An Organization A Managerial PerspectiveDocument14 pagesCore Values and Formalization As Determinants of Individual Behavior in An Organization A Managerial PerspectiveMonica PalaciosNo ratings yet
- The Role of Beliefs in Teacher Agency: A Critical AnalysisDocument9 pagesThe Role of Beliefs in Teacher Agency: A Critical AnalysisSapna Shyam JeetahNo ratings yet
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- HIV in ENTDocument25 pagesHIV in ENTDeepak KumarNo ratings yet
- Ent Ospe Badhahin v1 7 PDFDocument26 pagesEnt Ospe Badhahin v1 7 PDFWasi OsmanNo ratings yet
- Drtbalu'S Otolaryngology Online: TracheomalaciaDocument3 pagesDrtbalu'S Otolaryngology Online: TracheomalaciaAnish RajNo ratings yet
- Chronic RhinosinusitisDocument36 pagesChronic RhinosinusitisAritro BhattacharjiNo ratings yet
- Acute Laryngitis: Li SGD 21 LBM 5Document40 pagesAcute Laryngitis: Li SGD 21 LBM 511juni09No ratings yet
- Sailedinitis PDFDocument8 pagesSailedinitis PDFNavatha MorthaNo ratings yet
- Otitis Media With EffusionDocument3 pagesOtitis Media With EffusionAnish RajNo ratings yet
- Surgical Treatment of Postintubation Tracheal StenosisDocument40 pagesSurgical Treatment of Postintubation Tracheal StenosisJessieca LiusenNo ratings yet
- Keratosis ObturansDocument12 pagesKeratosis ObturansRahma LuthfaNo ratings yet
- Ear, Nose and Throat EmergenciesDocument3 pagesEar, Nose and Throat Emergenciesfmta100% (1)
- Benign Malignant LarynxDocument28 pagesBenign Malignant LarynxfaizNo ratings yet
- ScenarioDocument23 pagesScenarioAakashNo ratings yet
- Surgical Management of Thyroid NeoplasmsDocument15 pagesSurgical Management of Thyroid NeoplasmsalameluNo ratings yet
- Stenosis, Scleroma, TracheostomyDocument22 pagesStenosis, Scleroma, Tracheostomysimi yNo ratings yet
- Nasopharyngeal AngiofibromaDocument51 pagesNasopharyngeal Angiofibromakamal saudNo ratings yet
- Stridor in Children: By: Maj Vishal Gaurav Moderator: DR A SethiDocument33 pagesStridor in Children: By: Maj Vishal Gaurav Moderator: DR A SethiVishal GauravNo ratings yet
- CPR 1Document12 pagesCPR 1Renju JoseNo ratings yet
- Tumours of HypopharynxDocument32 pagesTumours of HypopharynxDurrikamil khattakNo ratings yet
- Maxillary Sinus CarcinomaDocument4 pagesMaxillary Sinus CarcinomaSuresh MettaNo ratings yet
- Headache-An ENT ProblemDocument59 pagesHeadache-An ENT ProblemMrudula MukiriNo ratings yet
- DysphagiaDocument4 pagesDysphagiaMicaNo ratings yet
- CSF RhinorrhoeaDocument12 pagesCSF RhinorrhoeaRohit Chandrasekhar100% (1)
- Ragay - Notes of EentDocument15 pagesRagay - Notes of Eentaynin39No ratings yet
- Otitis Externa: Investigation and Evidence-Based TreatmentDocument45 pagesOtitis Externa: Investigation and Evidence-Based TreatmentSonya HyekyoNo ratings yet
- Ent Emergencies NKDocument39 pagesEnt Emergencies NKGx NavinNo ratings yet
- Basic Sinus AnatomyDocument71 pagesBasic Sinus AnatomyTalal AlanzyNo ratings yet
- E.N.T Guide For Medical Students: Neck Examination: Dr. Giovanni Henry ENT Resident 2016Document79 pagesE.N.T Guide For Medical Students: Neck Examination: Dr. Giovanni Henry ENT Resident 2016John M. HemsworthNo ratings yet
- The Nose & Paranasal SinusesDocument17 pagesThe Nose & Paranasal SinusesMarera DomnicNo ratings yet
- Tonsillitis & TonsillectomyDocument18 pagesTonsillitis & TonsillectomyLuqman HakimNo ratings yet
- JnaDocument34 pagesJnaDeepak KumarNo ratings yet
- Ent PPT On Pharyngeal AbscessDocument20 pagesEnt PPT On Pharyngeal AbscessDocwocNo ratings yet
- Pharyngeal Tumours2Document46 pagesPharyngeal Tumours2miramirajalalNo ratings yet
- External Ear DisordersDocument48 pagesExternal Ear DisordershemaanandhyNo ratings yet
- Chemoprevention Head Neck MalignanciesDocument3 pagesChemoprevention Head Neck MalignanciesSuprit Sn100% (2)
- Photodynamic Therapy As Adjuvant Treatment of Extensive Basal Cell Carcinoma Treated With Mohs Micrographic SurgeryDocument19 pagesPhotodynamic Therapy As Adjuvant Treatment of Extensive Basal Cell Carcinoma Treated With Mohs Micrographic SurgerydocanggunNo ratings yet
- Anatomy and Physiology of Hearing SystemDocument63 pagesAnatomy and Physiology of Hearing SystemKharenza Vania Azarine Bachtiar100% (1)
- Chronic TonsillitisDocument47 pagesChronic Tonsillitissuci0% (1)
- Upper Airway ObstructionDocument17 pagesUpper Airway ObstructionRai Hana100% (1)
- Cortical Mastoid SurgeryDocument22 pagesCortical Mastoid Surgerymanu100% (1)
- TympanoplastyDocument4 pagesTympanoplastyMelly Selvia ANo ratings yet
- Nasal Septal Hematoma DrainageDocument21 pagesNasal Septal Hematoma DrainageRaja AlfatihNo ratings yet
- Chronic Suppurative Otitis Media A Model Case Sheet by DrtbaluDocument2 pagesChronic Suppurative Otitis Media A Model Case Sheet by DrtbaluMaria Arifuddin0% (1)
- Laryngeal CancerDocument41 pagesLaryngeal CancerNidya PutriNo ratings yet
- ENT Emergencies - DR Azwar Ridwan, SP - THT-KLDocument51 pagesENT Emergencies - DR Azwar Ridwan, SP - THT-KLHayatul AkmaLiaNo ratings yet
- AtelektasisDocument15 pagesAtelektasisMuhammad Ade RahmanNo ratings yet
- Tracheostomy: Dr. Amar KumarDocument18 pagesTracheostomy: Dr. Amar KumarSudhanshu ShekharNo ratings yet
- Temp Bone Trauma Slides 051012Document55 pagesTemp Bone Trauma Slides 051012RaihanFarhanaNo ratings yet
- Parapharyngeal Space TumorsDocument60 pagesParapharyngeal Space TumorsHossam ThabetNo ratings yet
- OtomycosisDocument10 pagesOtomycosisMichael SihombingNo ratings yet
- WK13 CDN - Meningitis, Poliomyelitis, Leprosy, Tetanus, Red TideDocument43 pagesWK13 CDN - Meningitis, Poliomyelitis, Leprosy, Tetanus, Red TidePotato PceeNo ratings yet
- Name: Bhanderi Akashkumar H. Clinical Clerk BCCM. ROTATION: OCT. 11-20, 2020Document7 pagesName: Bhanderi Akashkumar H. Clinical Clerk BCCM. ROTATION: OCT. 11-20, 2020Venkatesh GarikapatiNo ratings yet
- STDDocument49 pagesSTDArnzz AgbulosNo ratings yet
- Common Ent DisordersDocument20 pagesCommon Ent DisordersattaheeraNo ratings yet
- Uk PFAPADocument5 pagesUk PFAPAPrerna SehgalNo ratings yet
- Cranial Nerves: Hemachandran G Bot 2 Year RA1821002010077Document17 pagesCranial Nerves: Hemachandran G Bot 2 Year RA1821002010077HEMA CHANDRAN100% (1)
- Neck Mass ProtocolDocument8 pagesNeck Mass ProtocolCharlene FernándezNo ratings yet
- OtosclerosisDocument44 pagesOtosclerosisSonal Sharma100% (1)
- Mediastinal Tumors, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandMediastinal Tumors, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Antimicrobial Stewardship PhicnaDocument73 pagesAntimicrobial Stewardship PhicnaLovely Acabado TampocoNo ratings yet
- Natural Reservoir: How Can I Protect My Pet From Rabies?Document3 pagesNatural Reservoir: How Can I Protect My Pet From Rabies?Lovely Acabado TampocoNo ratings yet
- Respiratory FailureDocument5 pagesRespiratory FailureLovely Acabado Tampoco100% (1)
- EMTDocument73 pagesEMTLovely Acabado TampocoNo ratings yet
- Hypoxemic Resp. FailureDocument52 pagesHypoxemic Resp. FailureLovely Acabado TampocoNo ratings yet
- StressDocument30 pagesStressLovely Acabado TampocoNo ratings yet
- Surgical Hand WashingDocument1 pageSurgical Hand WashingLovely Acabado TampocoNo ratings yet
- Schizophrenia Schematic Diagram: Positive (Hard) Symptoms: Negative (Soft) SymptomsDocument1 pageSchizophrenia Schematic Diagram: Positive (Hard) Symptoms: Negative (Soft) SymptomsLovely Acabado Tampoco100% (1)
- Concept of AnxietyDocument52 pagesConcept of AnxietyLovely Acabado TampocoNo ratings yet
- Personality DisordersDocument42 pagesPersonality DisordersLovely Acabado Tampoco100% (1)
- A Teaching Method Comprises The Principles and Methods Used For InstructionDocument19 pagesA Teaching Method Comprises The Principles and Methods Used For InstructionLovely Acabado TampocoNo ratings yet
- Neuro BrandingDocument41 pagesNeuro BrandingZia AhmedNo ratings yet
- CACCIATORE, Et Al v. COUNTY OF BERGEN, Et Al - Document No. 31Document26 pagesCACCIATORE, Et Al v. COUNTY OF BERGEN, Et Al - Document No. 31Justia.comNo ratings yet
- Munasque vs. CADocument2 pagesMunasque vs. CASam FajardoNo ratings yet
- Buddhist Film Collection 270Document34 pagesBuddhist Film Collection 270Kev0192No ratings yet
- Parts of A Persuasive EssayDocument28 pagesParts of A Persuasive EssayHannaNo ratings yet
- Conversion Design: EcommerceDocument48 pagesConversion Design: EcommerceasthapriyamvadaNo ratings yet
- Advanced Cambridge TestDocument2 pagesAdvanced Cambridge TestbajickaNo ratings yet
- BM400V1ABDocument364 pagesBM400V1ABNeivi CfNo ratings yet
- Format Incident Report New 2019Document2 pagesFormat Incident Report New 2019Meliza RollanNo ratings yet
- English Practice Book 4Document19 pagesEnglish Practice Book 4akilasrivatsavNo ratings yet
- Missing PersonDocument24 pagesMissing PersonmichaNo ratings yet
- Credit Transactions: Group 1Document46 pagesCredit Transactions: Group 1Joovs Joovho100% (1)
- MyTradeTV Glass and Glazing Digital Magazine July 2015Document148 pagesMyTradeTV Glass and Glazing Digital Magazine July 2015Lee ClarkeNo ratings yet
- Y12 2nd Year Internship DetailsDocument27 pagesY12 2nd Year Internship DetailsKartikeyBhargavNo ratings yet
- Comparison of Early Measurements of The Distraction Index, Norberg Angle On Distracted View and The of Ficial Radiographic Evaluation of The Hips of 215 Dogs From Two Guide Dog Training SchoolsDocument7 pagesComparison of Early Measurements of The Distraction Index, Norberg Angle On Distracted View and The of Ficial Radiographic Evaluation of The Hips of 215 Dogs From Two Guide Dog Training SchoolsAna CicadaNo ratings yet
- Rohan ResumeDocument2 pagesRohan ResumeRohanNo ratings yet
- The Wanderer & Seafearer - 230228 - 151524Document8 pagesThe Wanderer & Seafearer - 230228 - 151524Nikolett LakatosNo ratings yet
- Britni Freiboth's Resume 2010Document2 pagesBritni Freiboth's Resume 2010api-51238443No ratings yet
- Membangun Teori Dan Konsep Asuhan Kebidanan Kehamilan, Persalinan, Nifas, BBL, KB Dan KesproDocument28 pagesMembangun Teori Dan Konsep Asuhan Kebidanan Kehamilan, Persalinan, Nifas, BBL, KB Dan KesproNikytaNo ratings yet
- 5 SustainableMarketingDocument554 pages5 SustainableMarketingSandesh TariNo ratings yet
- TCSDocument17 pagesTCSFahad MaqsoodNo ratings yet
- English 10 ReviewerDocument4 pagesEnglish 10 Reviewerathea garciaNo ratings yet
- Jasunjski Manastir Svetog Jovana PreteceDocument6 pagesJasunjski Manastir Svetog Jovana PreteceMaja JovanovicNo ratings yet
- FAQs in C LanguageDocument256 pagesFAQs in C LanguageShrinivas A B0% (2)
- Lourdes Andrade Science Reflection Final WebDocument2 pagesLourdes Andrade Science Reflection Final Webapi-270549230No ratings yet
- 3.1 Thermal PhysicsDocument10 pages3.1 Thermal Physicsmardel11No ratings yet
- Rejda rmiGE ppt01Document25 pagesRejda rmiGE ppt01Fadi OsamaNo ratings yet
- A Report On: Bachelor of Technology IN Civil EngineeringDocument31 pagesA Report On: Bachelor of Technology IN Civil EngineeringKalyan Reddy AnuguNo ratings yet