Professional Documents
Culture Documents
S1877065712X00071 S1877065712008536 Main
S1877065712X00071 S1877065712008536 Main
Uploaded by
omboOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
S1877065712X00071 S1877065712008536 Main
S1877065712X00071 S1877065712008536 Main
Uploaded by
omboCopyright:
Available Formats
The PRM care pathways are short documents, aiming to describe in a strong
and precise manner what PRM care can offer patients, i.e. why and how our
competencies and those of our team of rehabilitation professionals should be
proposed to patients and integrated around their life project. They describe for
each type of patients their specic pathology-related needs, place and objectives
of PRM care, human and material resources needed as well as a proper time line
and expected outcomes.
These pathways bring two novelties: description of the whole pathway of a
patient; an approach based on the consequences instead of the pathology. The
proposal is to group patients relating to their deciencies (paresis, pain,
aphasia. . .) and personal and environmental factors according to the
International Classication of Functioning (WHO). These last parameters
are likely to modify the means to be provided for the same objectives.
Depending on the complexity of the situation, the PRM care pathways are
declined into two ways:
type 1 (Stroke, Traumatic brain injury [TBI], Spinal cord injury [SCI])
relating to the severity of the deciencies. Then 4 categories are proposed for
Stroke, 3 for TBI and 5 for SCI;
type 2 (rotator cuff tear surgery, knee ligamentoplasty, hip arthroplasty, knee
arthroplasty): by stage of care after a simple act, mostly surgical, declined into
two situations relating to the medical complexity.
These pathways were given a warm welcome by many of our partners, as the
National Direction for Care, the Union for the management of the social
insurance facilities, the Federation of French Hospitals.
This approach, broaden to the others medical specialties of the following care
facilities could be the basis for the conception of a new medico-economic tool,
in the view of the new nancing to be applied in France, by creating
homogenous groups of patients, really descriptive of the needs, without being
obliged to use a detailed quantitative description of the acts.
http://dx.doi.org/10.1016/j.rehab.2012.07.755
CO38-002-e
An adaptive signal processing model for neurological
recovery
J. Palicot
SUPELEC/IETR, avenue de la Boulaie, CS 47601, 35576 Cesson-Sevigne,
France
E-mail address: jacques.palicot@supelec.fr.
Keywords: Theoretical model; Adaptive signal processing; Neurological
rehabilitation
In this article, we will apply a classical Adaptive Signal Processing model
(ASP) to neurological recovery. This work is the result of a two-fold experience:
in the eld of ASP in telecommunications, plus 15 years of experience in
neurological rehabilitation. Unlike traditional studies, which derive SP
algorithms from bio-inspired examples, in this article we shall apply ASP to
neurological rehabilitation. The application of this type of theory to the problem
of neurological rehabilitation, which is considered to be an adaptive process,
subject to various assumptions and considerations, will be detailed in the body
of this article. It enables us to shed new light on this type of therapeutic practice
and neuroplasticity, and deduce a certain number of practical conclusions.
The model is based on the hypothesis that rehabilitation as such is the sum of a
very large number of elementary rehabilitations (a function or movement, for
instance), each of which corresponds to an adaptive model. In this article, we
assume that adaptation follows a very typical stochastic gradient algorithm: this
minimises a function known, in conventional ASP, as the Mean Squared Error.
In this case we obtain the well-known Least Mean Square (LMS) algorithm, in
which there is an error which will be taken here as the error between the result
obtained and the nominal function.
Like any stochastic gradient algorithm, the convergence speed and precision
(residual error, known in this context as a sequela) are governed by a
convergence step.
Finally, we will drawa certain number of conclusions that are typical in ASP but
also relevant in terms of neurological rehabilitation. Among these, the following
will be discussed:
convergence/recovery speed;
transitional regime/rapid recovery phase;
stationary regime/stationary phase;
local minima/states of incomplete recovery;
residual error/sequelae;
convergence stability/stability in the patients condition;
time taken to reach a level of residual error/time taken to reach a level of
recovery/theoretical limit of neurological recovery. The main conclusion is that
there is no theoretical limit to the neurological rehabilitation. The sole limit is
the one given by the patient and/or the therapist, in all conscience.
http://dx.doi.org/10.1016/j.rehab.2012.07.756
CO38-003-e
Nutritional status of patients in Physical and
Rehabilitation Medicine (PRM) units
N. Chohra
*
, B. Barrois, C. Gerin, S. Ghemrani
Service de MPR, CH de Gonesse, BP 30071, rue Bernard-Fevrier,
95503 Gonesse, France
*Corresponding author.
E-mail address: nabil.chohra@ch-gonesse.fr.
Keywords: Undernutrition; BMI; PRM
Introduction. Nutritional status is a formal quality indicator in post-acute care
units to screen for frequently encountered undernutrtion.
Objectives. Analyse Body Mass Index (BMI) registered at admission and each
fortnight. Search for correlations between BMI and patients markers in a PRM
unit specialised in musculoskeletal system disease.
Patients and methods. The study involved inpatients in the PRM unit between
September and November 2011. Patients were classied into 4 groups: low
BMI < 18 kg/m
2
, normal 1825 kg/m
2
, overweight 2630 kg/m
2
and obe-
se > 30 kg/m
2
. In each group, average age and average duration of the stay
(DoS) were recorded.
Results. Sixty-eight patients had a musculoskeletal disease. The average age
was 62.7 years. DoS was 25.7 days. The distribution by BMI category was: low
(n = 0), normal (n = 16, 23%, mean age 60 years, DoS 24.3 days), overweight
(n = 28, 41%, mean age 61.8 years, DoS 26.5 days), and obese (n = 24, 35%,
mean age 66.6 years, DoS 24.4 days). The C-reactive protein level, monitored
during the postoperative period, normalized in all cases before day 30.
Discussion. In this PRM musculoskeletal unit, there were no undernourished
patients. This public health problem in geriatrics was not found to be a PRM
problem, but overweight affected 76% of patients.
The obese subjects were the oldest. The DoS was the same in three groups.
Analysis of other indicators of nutritional status disclosed a normal CRP.
Albuminaemia is not systematically assayed.
Conclusion. Excess weight was a frequent nding (76% of patients), however
there were no subjects with low BMI. Work on overweight patients is in
progress. The BMI had no impact on the average duration of hospital stay. The
study should be completed by research on biological signs of undernutrition.
http://dx.doi.org/10.1016/j.rehab.2012.07.757
CO38-004-e
Antibiotherapy for urinary tract infections in patient with
spinal cord or brain injury: Impact of a professional
practices clinical audit
S. Bauler
a,
*
, A. Janoly-Dumenil
a
, S. Bassi
a
, J. Luaute
b
, S. Jacquin-Courtois
b
,
S. Ciancia
b
, F. Costaz
c
, K. Charvier
b
, C. Rioufol
a
, G. Rode
b
a
Service de pharmacie clinique, hopital H.-Gabrielle-SSR, groupement
hospitalier Sud, hospices civils de Lyon, 20, route de Vourles, 69230 Saint-
Genis-Laval, France
b
Service de reeducation neurologique, hopital H.-Gabrielle-SSR, groupement
hospitalier Sud, hospices civils de Lyon, Saint-Genis-Laval, France
c
Service qualite, hopital H.-Gabrielle-SSR, groupement hospitalier Sud,
hospices civils de Lyon, Saint-Genis-Laval, France
*Corresponding author.
E-mail address: stephanie.bauler@chu-lyon.fr.
Protocoles, Qualite des soins (II) / Revue dE
pidemiologie et de Sante Publique 55S (2012) e297e303 e300
Keywords: Urinary tract infection; Antibiotics; Spinal cord injuries; Brain
injuries; Clinical audit
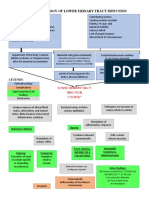
Introduction. Patients with neurological bladder dysfunction develop urinary
tract infections (UTI) which can be very concerning considering their
frequencies, severity and resistances to antibiotics (ATB) [1]. A professional
practice assessment (PPA) began in 2009 through a clinical audit [2], followed
by the diffusion of guidelines. A second audit has been carried out to assess the
impact of guidelines (2011).
Patients and methods. A two-month prospective study was conducted in the 7
neurological rehabilitation clinical units. Data collection included information
about patient, infection and ATB. The evaluation criteria were: initial empiric
ATB choice, dosage, ATB revaluated after 72 h according to antibiogram (for
empiric treatment), ATB duration. The compliance rate of these criteria was
analyzed and compared with results of the previous audit (by comparison of
proportions test when patients number allowed it).
Results. Thirty-eight patients were included in the study (47 15 years).
Fifty-two percent of patients had neurogenic bladder. Patients were treated for
bacterial colonization before an invasive procedure (32%), for prostatitis (42%)
or for a simple urinary tract infection (26%). The initial treatments were empiric
in 26% of cases. The initial choice of ATB was not suitable for 21% of
prescriptions (vs. 45% in 2009, P < 0.05). Ninety-two percent of patients
received the right antibiotic dose (vs. 94%, ns). Empiric treatments were
reevaluated at 72 h in 60% of cases (vs. 92% in 2009). Finally, treatment
durations were not respected in 26% of cases (vs. 52%, P < 0.05).
Discussion. There is a positive evolution in professional practice, including
treatment durations and choice of ATB more adapted compared to the 2009
audit. However, the reassessment of empirical treatment is insufcient, even
though it is a major criterion for quality monitoring in the HAS
recommendations. The implementation of simple indicators with monthly
monitoring is the next step; as it will help to perpetuate our work.
References
[1] J Hosp Infect 2006; 62:4739.
[2] 39th European Symposium of Clinical Pharmacy, Lyon, 2010.
http://dx.doi.org/10.1016/j.rehab.2012.07.758
CO38-005-e
Klebsielle pneumoniae carbapenemase productive epidemic
in a PRM department
N. Bradai
*
, L. Stana, P. Sportouch, C. Scouarnec, V. David, L. Damamme,
J.-M. Guerin, V. Chauvin, A. Yelnik
Service de MPR, universite Paris Diderot, Lariboisie`reF.-Widal, CHU Saint-
Louis, APHP, 200, rue du Faubourg-Sainte-Denis, 75010 Paris, France
*Corresponding author.
E-mail address: nacera.bradai@lrb.aphp.fr.
Introduction. We had to face an epidemic of Klebsielle Pneumoniae
Carbapenemase productive (KPC), a negative Gram bacillus with a high
acquiring and diffusing resistance capacity. The drastic organization needed
during 8 months is described.
Method. Bacillus was found in 2 patients coming fromneurosurgery. Fromthis
day (02/02/2011), the following measures have been applied:
crises centre including hygiene committee of Paris Nord and APHP, direction
and hygiene teams of the hospital, physicians, nurses and rehabilitation teams;
suspension of the admission for 15 days;
reorganization of the department with 2 sectors for contaminated patients and
for suspects of carrying bacillus, then a third one unaffected with new
patients;
geographic and chronologic reorganization of the rehabilitation;
strict isolation in bedroom for contaminated patients (dedicated team,
rehabilitation in bedroom). . .
for each present patient at this time, considered as contact, a weekly rectal
swab, twice per month from august, till discharge even when the were negative;
they beneciated from specic measures for resistant bacillus contaminated
patients.
Results. Forty-four patients were concerned; among them 4 contaminated.
Only one diagnosed among contact and one being admitted, team aware of
contamination. Return to a normal situation after discharge of the last patient
(26/09/11) with this cost: 543 rectal swab; 388 unavailable days for inpatients;
382 days of additional nursing staff; 11 meeting of the crisis centre; increase of
the length of stay related to difculties with discharge of these patients; lack of
15 admissions compared with previous years; high psychological impact.
Conclusion. Fighting against such epidemic in a PRM department is difcult
and needs strictness leading to psychologically painful isolation, lack of change
in rehabilitation and a high nancial cost. We have to be prepared for such
increasing problem.
http://dx.doi.org/10.1016/j.rehab.2012.07.759
CO38-006-e
A prevalence of second-look diagnoses in the post-acute
rehabilitation setting: A new challenge?
M. Iakova
*
, A. Vouilloz, F. Luthi
Departement de lappareil locomoteur, clinique romande de readaptation
SUVA Care, avenue Grand Champsec 90, 1950 Sion, Switzerland
*Corresponding author.
E-mail address: maria.iakova@crr-suva.ch.
Keywords: Second-look diagnoses; Rehabilitation
Purpose. Post-acute care rehabilitation is in full development. Indeed, the
evolution of health systems aims towards an important reduction of hospital stay
and towards an earlier referral of patients with severe conditions. This study
aimed to measure the prevalence of diagnoses made only during the post-acute
rehabilitation phase (the so-called second look diagnoses).
Methods. Patients hospitalized in a post-acute care rehabilitation unit.
Retrospective study over one year using the patients electronic medical charts.
The second-look diagnoses made during the rehabilitation and also
complementary investigations and therapeutic changes were recorded.
Results. During the study, 103 patients (p) received care in our unit following
multiple trauma, prosthesis implantation (hip/knee/shoulder), lower limb
amputation or burn injury. Thirty-seven new diagnoses was recorded in 21 p
(20.4%), 18 males, 3 females, mean age 38 years. Twelve musculoskeletal
injuries were retained. In 25 cases a neurological condition was diagnosed. For
8 patients, more than one second-look diagnosis was established. Symptoms
were the main argument for the revision of the initial diagnoses in 86% of the
cases, and X-ray revision for 14% others. Twenty-nine additional investigations
were required. For all patients, orthopaedic and\or pharmacological treatments,
as well as an adaptation of the rehabilitation protocol were necessary.
Discussion. To our knowledge, there is no a data in the literature about
second-look diagnoses in the post-acute care rehabilitation setting. The 20%
prevalence observed in our study is high. The prevalence of the neurological
conditions was that of musculoskeletal disorders. The vast majority of
diagnoses (95%) were made in multiple trauma patients. The evolution of the
health systems, characterized by a reduction of hospital stay duration, might
contribute to extend this problem. It could also represent a new challenge for
rehabilitation wards in terms of organization and relation with acute care units.
http://dx.doi.org/10.1016/j.rehab.2012.07.760
CO38-007-e
Group workshops as part of guided self-rehabilitation
contracts in spastic paresis: Our 20092012 experience
C. Gault-Colas
*
, A. Behnegar, C. Hennegrave, E. Lamour, S. Joudoux,
T. Santiago, J.-M. Gracies
Service de medecine physique et de readaptation, hopital Albert-Chenevier,
groupe hospitalier Henri-Mondor, 40, rue de Mesly, 94010 Creteil, France
*Corresponding author.
E-mail address: caroline.colas@ach.aphp.fr.
Keywords: Spastic paresis; Contract; Guided self-rehabilitation; Workshop;
Group
Introduction. Guided Self-rehabilitation Contracts (GSC) in paretic patients
(after stroke, head or spinal cord injury, nervous system tumour, multiple
Protocoles, Qualite des soins (II) / Revue dE
pidemiologie et de Sante Publique 55S (2012) e297e303 e301
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (347)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- ghq-28 FORMDocument2 pagesghq-28 FORMombo40% (5)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 2021 Abstract Book FINAL - KNC - 040621Document115 pages2021 Abstract Book FINAL - KNC - 040621purplelydiaNo ratings yet
- Practice Test Pediatric Nursing 100 ItemsDocument17 pagesPractice Test Pediatric Nursing 100 ItemsMichelle Lureineil Dajao100% (3)
- Herbs-Sam CoffmanDocument9 pagesHerbs-Sam CoffmanSilambarasu Karuppiah0% (1)
- Ggi12193 PDF Jsessionid f01t02Document9 pagesGgi12193 PDF Jsessionid f01t02omboNo ratings yet
- 6 Minute Walk Test InstructionsDocument3 pages6 Minute Walk Test InstructionsJill LoveNo ratings yet
- Suck Training PDFDocument2 pagesSuck Training PDFomboNo ratings yet
- Denis ClassificationDocument2 pagesDenis ClassificationomboNo ratings yet
- Alternative FeedingDocument4 pagesAlternative FeedingomboNo ratings yet
- Case AnalysisDocument1 pageCase AnalysisomboNo ratings yet
- Expected Outcomes: What You Should Know: T1-9 Spinal Cord InjuryDocument23 pagesExpected Outcomes: What You Should Know: T1-9 Spinal Cord InjuryomboNo ratings yet
- Richi HW Neurodiv PMR Dept.Document5 pagesRichi HW Neurodiv PMR Dept.omboNo ratings yet
- Case Report: MR - NC, 21 Y.o, Right Handed, Lives in Pasanggrahan Street Cisalak Subang, Reffered FromDocument8 pagesCase Report: MR - NC, 21 Y.o, Right Handed, Lives in Pasanggrahan Street Cisalak Subang, Reffered FromomboNo ratings yet
- WPC 096853Document7 pagesWPC 096853omboNo ratings yet
- 24 - Liquor AnaliseDocument6 pages24 - Liquor AnaliseomboNo ratings yet
- Chapter 7 Examination of Cerebrospinal Fluid and Serous Membrane FluidDocument8 pagesChapter 7 Examination of Cerebrospinal Fluid and Serous Membrane FluidomboNo ratings yet
- Physiology of Pain: Guide To Pain Management in Low-Resource SettingsDocument6 pagesPhysiology of Pain: Guide To Pain Management in Low-Resource SettingsomboNo ratings yet
- Soal Ujian Semester 1 DMDocument10 pagesSoal Ujian Semester 1 DMomboNo ratings yet
- Constipation Biofeedback For Pelvic Floor Dysfunction In: Data Supplement ReferencesDocument5 pagesConstipation Biofeedback For Pelvic Floor Dysfunction In: Data Supplement ReferencesomboNo ratings yet
- Myomed932 The RoleDocument8 pagesMyomed932 The RoleomboNo ratings yet
- Tadic S, Schaefer W, Griffiths D, Resnick N 1. University of PittsburghDocument2 pagesTadic S, Schaefer W, Griffiths D, Resnick N 1. University of PittsburghomboNo ratings yet
- VCUG (Voiding Cystourethrogram) What It IsDocument3 pagesVCUG (Voiding Cystourethrogram) What It IsNinaNo ratings yet
- Urinary RetentionDocument6 pagesUrinary Retentionjakenathanielvelasco50% (2)
- DiGeorge SyndromeDocument11 pagesDiGeorge SyndromeRupesh MohandasNo ratings yet
- Trafficking of Women HarshitaDocument31 pagesTrafficking of Women HarshitaRajkumar SinghalNo ratings yet
- Urinary and Male GenitalDocument116 pagesUrinary and Male GenitalMultazam ZamNo ratings yet
- National Antibiotic Pedia GuidelinesDocument149 pagesNational Antibiotic Pedia GuidelinesGg GreyNo ratings yet
- BRT Surgery - Urology Part 2Document3 pagesBRT Surgery - Urology Part 2Princess Sittie Asiah AbdullahNo ratings yet
- UTI Practicum Make-Up Assignment FINALDocument8 pagesUTI Practicum Make-Up Assignment FINALlmstar98No ratings yet
- Pathophysiology of Lower Urinary Tract InfectionDocument1 pagePathophysiology of Lower Urinary Tract InfectionSTORAGE FILENo ratings yet
- Coc 2022 Reviewed Q & ADocument74 pagesCoc 2022 Reviewed Q & ASneeze LouderNo ratings yet
- Bakteriologi Urin 2020Document23 pagesBakteriologi Urin 2020QUINITA NORONHANo ratings yet
- Pathology of The Male GUTDocument108 pagesPathology of The Male GUTHoque Mohammed Newaz ShorifulNo ratings yet
- Aafp Uti GuidelinesDocument10 pagesAafp Uti GuidelinesCess Lagera YbanezNo ratings yet
- Protocol Book For OBGYNDocument41 pagesProtocol Book For OBGYNShabir BadakhshNo ratings yet
- Homeo-11 RrUBRICSDocument32 pagesHomeo-11 RrUBRICSRashid MahmoodNo ratings yet
- S.C. Madan Homeopathy Cures Where Allopathy Fails: LeseprobeDocument6 pagesS.C. Madan Homeopathy Cures Where Allopathy Fails: LeseprobeTanuj TyagiNo ratings yet
- Alaska Tribal Health Webinar Series Dr. Emily Hogeland Pediatric Hospitalist Alaska Native Medical Center September 3, 2021Document36 pagesAlaska Tribal Health Webinar Series Dr. Emily Hogeland Pediatric Hospitalist Alaska Native Medical Center September 3, 2021solthneNo ratings yet
- Monuril Vs CiproDocument7 pagesMonuril Vs Ciproalaa morsyNo ratings yet
- RenalDocument60 pagesRenalEdmalyn Dela CruzNo ratings yet
- CHCCCS011 Student Assessment Theory Task 06122020 - Ha NguyenDocument29 pagesCHCCCS011 Student Assessment Theory Task 06122020 - Ha NguyenNguyen Ha0% (1)
- DR Jones Cat Health Web Clinic Slides 1222Document222 pagesDR Jones Cat Health Web Clinic Slides 1222Haider Al Zamily100% (1)
- Approach To HematuriaDocument15 pagesApproach To HematuriaArsalan NadeemNo ratings yet
- ACKD Susp Lupus NefritisDocument61 pagesACKD Susp Lupus Nefritisrastu karyanaNo ratings yet
- 2022 December BlueprintDocument38 pages2022 December BlueprintNonoy JoyaNo ratings yet
- Family Case Study - BN4A Group 2Document46 pagesFamily Case Study - BN4A Group 2Rene John Francisco100% (1)
- HLB, NME, M& M OSCE Notes - University of Manchester, WL GanDocument45 pagesHLB, NME, M& M OSCE Notes - University of Manchester, WL GanWeh Loong Gan100% (2)
- Utrine ProlapseDocument22 pagesUtrine ProlapseMuskan RastogiNo ratings yet