Professional Documents
Culture Documents
Evaluating: Nursing Care Plan
Uploaded by
John Rey AbadOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Evaluating: Nursing Care Plan
Uploaded by
John Rey AbadCopyright:
Available Formats
1478 UNIT X / Promoting Physiologic Health
Evaluating
Using the overall goals identified in the planning stage of main-
taining or restoring fluid balance, maintaining or restoring pul-
monary ventilation and oxygenation, maintaining or restoring
normal balance of electrolytes, and preventing associated risks
of fluid, electrolyte, and acidbase imbalances, the nurse col-
lects data to evaluate the effectiveness of interventions. Exam-
ples of desired outcomes for the identified goals are found in
Identifying Nursing Diagnoses, Outcomes, and Interventions on
pages 1451 and 1452.
If desired outcomes are not achieved, the nurse, client, and
support person if appropriate need to explore the reasons before
modifying the care plan. For example, if the outcome Urine
output is greater than 1,300 mLper day and within 500 mLof in-
take is not achieved, questions to be considered might include
Have other outcome measures for the goal of achieving fluid
balance been met?
Does the client understand and comply with planned fluid intake?
Is all urinary output being measured?
Are unusual or excessive amounts of fluid being lost by an-
other route (e.g., gastric suction, excessive perspiration,
fever, rapid respiratory rate, wound drainage)?
Are prescribed medications being taken or administered as
ordered?
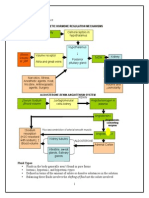
INITIATING, MAINTAINING, AND TERMINATING A BLOOD TRANSFUSION USING A Y-SET continued
S
K
I
L
L
5
2
-
6
EVALUATION
Evaluate the following:
Changes in vital signs or health status
Presence of chills, nausea, vomiting, or skin rash
NURSING CARE PLAN Deficient Fluid Volume
ASSESSMENT DATA NURSING DIAGNOSIS DESIRED OUTCOMES
*
Nursing Assessment
Merlyn Chapman, a 27-year-old sales clerk, reports weakness,
malaise, and flu-like symptoms for 34 days. Although thirsty, she
is unable to tolerate fluids because of nausea and vomiting, and
she has liquid stools 24 times per day.
Deficient Fluid Volume related
to nausea, vomiting, and diar-
rhea as evidenced by de-
creased urine output, increased
urine concentration, weakness,
fever, decreased skin/tongue
turgor, dry mucous mem-
branes, increased pulse rate,
and decreased blood pressure
Electrolyte & Acid/Base Bal-
ance [0600] as evidenced by
not compromised:
Serum electrolytes
Muscle strength
Fluid Balance [0601] as evi-
denced by not compromised:
24-hour intake and output
balance
Urine specific gravity
Blood pressure, pulse, and
body temperature
Skin turgor
Moist mucous membranes
Physical Examination
Height: 160 cm (53)
Weight: 66.2 kg (146 lb)
Mild fever: 38.6C (101.5F)
Pulse: 86 BPM
Respirations: 24/minute
Scant urine output
BP: 102/84 mm Hg
Dry oral mucosa, furrowed
tongue, cracked lips
Diagnostic Data
Urine specific gravity: 1.035
Serum sodium 155 mEq/L
Serum potassium 3.2 mEq/L
Chest x-ray negative
NURSING INTERVENTIONS
*
/SELECTED ACTIVITIES RATIONALE
Electrolyte Management: Hypokalemia [2007]
Obtain specimens for analysis of altered potassium levels (e.g.,
serum and urine potassium) as indicated.
Administer prescribed supplemental potassium (PO, NG, or IV)
per policy.
Monitor for neurologic and neuromuscular manifestations of hy-
pokalemia (e.g., muscle weakness, lethargy, altered level of con-
sciousness).
Urine and serum analysis provides information about extracellu-
lar levels of potassium. There is no practical way to measure in-
tracellular K
.
Low potassium levels are dangerous and Mrs. Chapman may
require supplements.
Potassium is a vital electrolyte for skeletal and smooth muscle
activity.
koz74686_ch52.qxd 11/21/06 1:08 PM Page 1478
CHAPTER 52 / Fluid, Electrolyte, and AcidBase Balance 1479
NURSING CARE PLAN Deficient Fluid Volume continued
NURSING INTERVENTIONS*/SELECTED ACTIVITIES RATIONALE
Monitor for cardiac manifestations of hypokalemia (e.g., hypoten-
sion, tachycardia, weak pulse, rhythm irregularities).
Many cardiac rhythm disorders can result from hypokalemia. It is
critical to monitor cardiac function with hypokalemia.
Electrolyte Management: Hypernatremia [2004]
Obtain specimens for analysis of altered sodium levels (e.g.,
serum and urine sodium, urine osmolality, and urine specific grav-
ity) as indicated.
Provide frequent oral hygiene.
Monitor for neurologic and neuromuscular manifestations of hy-
pernatremia (e.g., lethargy, irritability, seizures, and hyperreflexia).
Monitor for cardiac manifestations of hypernatremia (e.g., tachy-
cardia, orthostatic hypotension).
Urine analysis provides information about retention or loss of
sodium and the ability of the kidneys to concentrate or dilute urine
in response to fluid changes.
Oral mucous membranes become dry and sticky due to loss of
fluid in the interstitial spaces.
Hypernatremia, as a result of low fluid volume, creates a hyper-
tonic vascular space, which causes water to move out of the cells,
including brain cells. This accounts for neurologic symptoms.
The heart responds to a loss of fluid by increasing the heart rate to
compensate with an increase in cardiac output. Low fluid volume
leads to a fall in blood pressure.
Fluid Management [4120]
Weigh daily and monitor trends.
Maintain accurate I & O record.
Monitor vital signs as appropriate.
Give fluids as appropriate.
Administer IV therapy as prescribed.
Weight helps to assess fluid balance.
Accurate records are critical in assessing the patients fluid balance.
Vital sign changes such as increased heart rate, decreased blood
pressure, and increased temperature indicate hypovolemia.
As her nausea decreases encourage her oral intake of fluids as tol-
erated, again to replace lost volume.
Mrs. Chapman has signs of severe fluid volume deficit. She will
probably require intravenous replacement of fluid. This is especially
true because her oral intake is limited because of nausea and
vomiting.
EVALUATION
Outcomes met. Mrs. Chapman remained hospitalized for 48 hours. She required fluid replacement of a total of 5 liters. Her blood pressure
increased to 122/74, pulse rate decreased to a resting level of 74, and respirations decreased to 12/minute. Her urine output increased as
the fluid was replaced and was adequate at > 0.5 mL/kg/hour by the time of discharge. The urine specific gravity was 1.015. Lab work on
the day of discharge was: K: 3.8 and Na: 140. She had elastic skin turgor and moist mucous membranes. She was taking oral fluids and
was able to discuss symptoms of deficient fluid volume that would necessitate her calling her health care provider.
*
The NOC # for desired outcomes and the NIC # for nursing interventions and seleted activities are listed in brackets following the appropriate out-
come or intervention. Outcomes, interventions, and activities selected are only a sample of those suggested by NOC and NIC and should be further
individualized for each client.
APPLYING CRITICAL THINKING
1. What action would you take if Mrs. Chapmans heart became
irregular?
2. Mrs. Chapman is responding inappropriately to your questions;
she seems to be confused. What do you think is happening?
3. Offer suggestions for ways to help Mrs. Chapman increase her
oral intake.
4. Mrs. Chapman asks why you weigh her every morning. How do
you respond?
See Critical Thinking Possibilities in Appendix A.
koz74686_ch52.qxd 11/8/06 2:08 PM Page 1479
You might also like
- Fluid and Electrolytes for Nursing StudentsFrom EverandFluid and Electrolytes for Nursing StudentsRating: 5 out of 5 stars5/5 (12)
- Fluid & ElectrolyteDocument26 pagesFluid & Electrolytesanjana bhatia100% (1)
- Electrolyte Imbalance, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandElectrolyte Imbalance, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsRating: 1 out of 5 stars1/5 (1)
- Hypercalcemia, (High Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHypercalcemia, (High Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Alteration in Fluid and Electrolyte ImbalanceDocument118 pagesAlteration in Fluid and Electrolyte ImbalanceRenuga SureshNo ratings yet
- SIADHDocument19 pagesSIADHhendrik taufik100% (1)
- Hepatic Encephalopathy: Causes, Tests, and Treatment OptionsFrom EverandHepatic Encephalopathy: Causes, Tests, and Treatment OptionsRating: 3.5 out of 5 stars3.5/5 (2)
- Week4 PDFDocument56 pagesWeek4 PDFhelen100% (1)
- Fluid Electrolyte Imbalance NvertedDocument111 pagesFluid Electrolyte Imbalance Nvertedchitrakshi khairnarNo ratings yet
- Fluid and ElectrolytesDocument179 pagesFluid and ElectrolytesTrixie Al Marie75% (4)
- Maternity Nursing ObDocument11 pagesMaternity Nursing ObMayls Sevilla Calizo74% (19)
- Oxford Handbook of Evolutionary Medicine (Martin Brüne Wulf Schiefenhövel) (Z-Library)Document967 pagesOxford Handbook of Evolutionary Medicine (Martin Brüne Wulf Schiefenhövel) (Z-Library)Sam SoeteNo ratings yet
- Fluid Electrolyte Balances and ImbalanceDocument157 pagesFluid Electrolyte Balances and ImbalanceManisha Shakya0% (1)
- Myra Estrin Lavine: Introduction and BiographyDocument14 pagesMyra Estrin Lavine: Introduction and BiographyLouie ColladoNo ratings yet
- Fluidsandelectrolytes 090224074347 Phpapp02Document102 pagesFluidsandelectrolytes 090224074347 Phpapp02IsaacJ22No ratings yet
- Fluids and ElectrolytesDocument11 pagesFluids and Electrolytescarlo evardo100% (2)
- Medical Surgical Fluid and Electrolytes FVD FVEDocument7 pagesMedical Surgical Fluid and Electrolytes FVD FVEMichaelaKatrinaTrinidadNo ratings yet
- Advanced Engineering Surveying Name: Date .Document17 pagesAdvanced Engineering Surveying Name: Date .Nurul Najwa MohtarNo ratings yet
- Land Change Modeler ArcGIS Software BrochureDocument6 pagesLand Change Modeler ArcGIS Software BrochureFabio Leonel Casco GutierrezNo ratings yet
- HyponatremiaDocument42 pagesHyponatremiaAbdu Raheem100% (1)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Sodium, and 350-500 Meq/L of Chloride. The Combined Effects of Serum Hyperosmolarity, Dehydration, and Acidosis Result in Increased Osmolarity in Brain Cells That ClinicallyDocument5 pagesSodium, and 350-500 Meq/L of Chloride. The Combined Effects of Serum Hyperosmolarity, Dehydration, and Acidosis Result in Increased Osmolarity in Brain Cells That ClinicallyMorgan Mitchell100% (10)
- Fluid Electrolytes and Acid-Base BalanceDocument12 pagesFluid Electrolytes and Acid-Base BalanceHajra Al-Khuwaitem100% (1)
- Nursing Care Plan For AnemiaDocument14 pagesNursing Care Plan For AnemiaIbrahimWages100% (4)
- Fluid Imbalance (NCP)Document9 pagesFluid Imbalance (NCP)Putry RainismNo ratings yet
- Ascites, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandAscites, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- NCP For DehydrationDocument3 pagesNCP For Dehydrationpeter_degamo200025% (4)
- Fluid and Electrolyte - 2022Document147 pagesFluid and Electrolyte - 2022Lacangan, Thea YvonneNo ratings yet
- Fluid and Electrolyte Imbalances: Nursing Management Nursing Care Plan Discharge Planning Core CompetenciesDocument40 pagesFluid and Electrolyte Imbalances: Nursing Management Nursing Care Plan Discharge Planning Core Competenciesayazafra100% (1)
- Nursing Care Plan Endometrial CancerDocument2 pagesNursing Care Plan Endometrial Cancerderic87% (15)
- A1.2 Nucleic AcidsDocument83 pagesA1.2 Nucleic AcidsGhenwa DimachkiNo ratings yet
- Endocrine Disorders NotesDocument14 pagesEndocrine Disorders NotesSarahMelissaNo ratings yet
- PRAKRIT™ - Sutra To ScienceDocument8 pagesPRAKRIT™ - Sutra To ScienceSita ShankarNo ratings yet
- FLUID AND ELECTOLYTE IMBALANCE FinalDocument27 pagesFLUID AND ELECTOLYTE IMBALANCE FinalShiva BiradarNo ratings yet
- Neuroscience: Science of The Brain in RussianDocument72 pagesNeuroscience: Science of The Brain in RussianInternational Brain Research Organization100% (4)
- Fitrawati Arifuddin - Nursing Care Plan Deficiency of Fluid VolumeDocument12 pagesFitrawati Arifuddin - Nursing Care Plan Deficiency of Fluid VolumefitrawatiarifuddinNo ratings yet
- Nursing Care Plan HypovolemiaDocument8 pagesNursing Care Plan HypovolemiaGusmila SariNo ratings yet
- 2017 Fluid and Electrolytes LECTURE NOTESDocument34 pages2017 Fluid and Electrolytes LECTURE NOTESHarley Justiniani Dela CruzNo ratings yet
- Fluid and Electrolytes - Balance and DisturbancesDocument129 pagesFluid and Electrolytes - Balance and DisturbancesEmmy SaNo ratings yet
- Group 2: Magallon, Buenaventura Sallaberger, Jayrahnicole Agliam, Jessica May Diño, FortunatoDocument12 pagesGroup 2: Magallon, Buenaventura Sallaberger, Jayrahnicole Agliam, Jessica May Diño, FortunatoMarinela ManaloNo ratings yet
- DKADocument4 pagesDKAJacques BoucalNo ratings yet
- Alterations in Fluid VolumeDocument4 pagesAlterations in Fluid VolumeRichmund Earl GeronNo ratings yet
- Fluid and Electrolyte 10 RDocument87 pagesFluid and Electrolyte 10 RHea YaNo ratings yet
- CULLA - Activity 2Document2 pagesCULLA - Activity 2SheenaGuinoCullaNo ratings yet
- Deficient Fluid Volume Nursing Diagnosis & Care Plan - RNlessonsDocument11 pagesDeficient Fluid Volume Nursing Diagnosis & Care Plan - RNlessonsA.No ratings yet
- Fluid Electrolytes 2Document22 pagesFluid Electrolytes 2QueenClerk VillarteNo ratings yet
- MedSurg Group2Document4 pagesMedSurg Group2Lacangan, Thea YvonneNo ratings yet
- 2a FE, ABG - Paul BiluanDocument62 pages2a FE, ABG - Paul BiluanZhai LabardaNo ratings yet
- Ms. Hicks Case)Document3 pagesMs. Hicks Case)Chelsea AquinoNo ratings yet
- By: Irwan Subekti, Skep, NersDocument26 pagesBy: Irwan Subekti, Skep, NersEric Juan MaldiniNo ratings yet
- Lecture 1 - Fluid & Electrolyre Balance 2021Document44 pagesLecture 1 - Fluid & Electrolyre Balance 2021عمار عاشورNo ratings yet
- Fluids and ElectrolytesDocument26 pagesFluids and ElectrolytesRahul K. JagaNo ratings yet
- Presentation Mia FirstDocument76 pagesPresentation Mia FirstsyedosmanNo ratings yet
- Hepatic Encephalopathy and ComaDocument4 pagesHepatic Encephalopathy and ComaAriana ValenciaNo ratings yet
- Case 1a Answer KeyDocument4 pagesCase 1a Answer KeyChettan Kerala100% (1)
- Fluids and ElectrolytesDocument131 pagesFluids and ElectrolytesGianna j100% (1)
- Fluid, Electrolyte, Acid and Base Imbalances-1-1Document67 pagesFluid, Electrolyte, Acid and Base Imbalances-1-1Muhammad AsifNo ratings yet
- By DR Madhusudan C Associate Professor Department of MedicineDocument39 pagesBy DR Madhusudan C Associate Professor Department of MedicineTeena ChandranNo ratings yet
- General BCN NotesDocument400 pagesGeneral BCN NotesMoses FrancoNo ratings yet
- Hypovolemic ShockDocument36 pagesHypovolemic ShockRia CintyaNo ratings yet
- Hyponatremia 1Document36 pagesHyponatremia 1jack sawdaNo ratings yet
- Tau Chempath Lecture - Fluid & Electrolyte BalanceDocument48 pagesTau Chempath Lecture - Fluid & Electrolyte BalanceJoshua KalundaNo ratings yet
- Bio Begavioral Interventions and Holistic Care For Individuals and Family With Specific Problems in Oxygenation, Fluid and Electrolyte Balance, Metabolic and Endocrine FuntionDocument16 pagesBio Begavioral Interventions and Holistic Care For Individuals and Family With Specific Problems in Oxygenation, Fluid and Electrolyte Balance, Metabolic and Endocrine FuntionLiza AingelicaNo ratings yet
- Shock in Children TutorialDocument37 pagesShock in Children TutorialSsenyonga DominicNo ratings yet
- Nursing DiagnosisDocument4 pagesNursing DiagnosisMavy AndresNo ratings yet
- Acute Renal Failure8Document35 pagesAcute Renal Failure8Andrew MidaNo ratings yet
- Assignment 3Document5 pagesAssignment 3api-577583685No ratings yet
- Metabolic Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandMetabolic Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- MeniereDocument5 pagesMeniereMayls Sevilla CalizoNo ratings yet
- Initial Data Base For Family Nursing PracticeDocument7 pagesInitial Data Base For Family Nursing PracticeMayls Sevilla Calizo0% (1)
- Far Eastern University Assignment in Health Assessment Mayls S. Calizo AO9AO5 March 3, 2010 Prof. Mary Anne R. Pascual Laboratory TestsDocument4 pagesFar Eastern University Assignment in Health Assessment Mayls S. Calizo AO9AO5 March 3, 2010 Prof. Mary Anne R. Pascual Laboratory TestsMayls Sevilla CalizoNo ratings yet
- Earthquake (Ppe)Document8 pagesEarthquake (Ppe)Mayls Sevilla CalizoNo ratings yet
- Nursing Care Plan Jan. 13 2011Document8 pagesNursing Care Plan Jan. 13 2011Mayls Sevilla Calizo100% (1)
- LemonDocument2 pagesLemonMayls Sevilla CalizoNo ratings yet
- Nursing Care Plan Jan. 13 2011Document8 pagesNursing Care Plan Jan. 13 2011Mayls Sevilla Calizo100% (1)
- Hydrant Pillar - NikitaDocument1 pageHydrant Pillar - NikitaCitra mas0% (1)
- 2020 Hales Et Al. Signalling Inclusivity in UG Biology Courses Through Deliberate Framing of Genetics Topics Relevant To Gender Identity Disability and RaceDocument9 pages2020 Hales Et Al. Signalling Inclusivity in UG Biology Courses Through Deliberate Framing of Genetics Topics Relevant To Gender Identity Disability and RaceMichael KevinNo ratings yet
- JetoptimusDocument7 pagesJetoptimusShubh YouTubeNo ratings yet
- 18btc101j Biochem-Unit 1Document134 pages18btc101j Biochem-Unit 1nikteshgNo ratings yet
- Ecological PyramidsDocument13 pagesEcological PyramidsMukesh Kumar SharmaNo ratings yet
- Food Deterioration and Its ControlDocument3 pagesFood Deterioration and Its Controlansar ali100% (3)
- 2016 PDFDocument209 pages2016 PDFsky100% (3)
- 2012 OpenExam AnsKeyDocument11 pages2012 OpenExam AnsKeymartynapetNo ratings yet
- Tamil Nadu State Board Textbooks Samacheer Kalvi Class XII Botany Chapter 5 English MediumDocument15 pagesTamil Nadu State Board Textbooks Samacheer Kalvi Class XII Botany Chapter 5 English MediumSharath KNo ratings yet
- Original Research PaperDocument3 pagesOriginal Research Paperpriyanka728No ratings yet
- A Learning Theory Approach To Attachment Theory: Exploring Clinical ApplicationsDocument22 pagesA Learning Theory Approach To Attachment Theory: Exploring Clinical ApplicationsCláudioToméNo ratings yet
- BCH 332 Lectures 1 and 2 0Document33 pagesBCH 332 Lectures 1 and 2 0asdNo ratings yet
- REVISION TEST MEDICAL ENGLISH I Choose The Correct AnswerDocument3 pagesREVISION TEST MEDICAL ENGLISH I Choose The Correct Answerhoctrenlop080905No ratings yet
- BaSS 2019 Final ProgramDocument37 pagesBaSS 2019 Final ProgramArtanNo ratings yet
- R Reeggaarrddiinngg Tthhee Eexxaam Miinnaattiioonn: GDD ? H@Qka A9Fk KMJ? GFK H9Cakl9FDocument3 pagesR Reeggaarrddiinngg Tthhee Eexxaam Miinnaattiioonn: GDD ? H@Qka A9Fk KMJ? GFK H9Cakl9FAamir HamaadNo ratings yet
- GYNE 5.01 - Neoplastic Disease of The Ovary - Dr. TinioDocument7 pagesGYNE 5.01 - Neoplastic Disease of The Ovary - Dr. TinioMonique BorresNo ratings yet
- Class 10 Bio - Term 1 - Mcqs and Assertion QuestionsDocument10 pagesClass 10 Bio - Term 1 - Mcqs and Assertion QuestionsSTUDENTS DREAM BOX - CBSENo ratings yet
- Ai in Healthcare 202011 201117103639Document17 pagesAi in Healthcare 202011 201117103639羅浩維No ratings yet
- Topic: Our Environment: Subject: Biology CLASS:10Document25 pagesTopic: Our Environment: Subject: Biology CLASS:10sara parkNo ratings yet
- Ico Kin Etic S& Ico Dyn Am Ics: Professor Dr. Najat A. HasanDocument34 pagesIco Kin Etic S& Ico Dyn Am Ics: Professor Dr. Najat A. HasanMelkamu AyeNo ratings yet
- The Combined Chemical DictionaryDocument3 pagesThe Combined Chemical DictionaryDoryNo ratings yet