Professional Documents
Culture Documents
The Development of Proteinuria and Focal Segmental Glomerulosclerosis in Recipients of Pediatric Donor Kidneys Hayes Et Al
The Development of Proteinuria and Focal Segmental Glomerulosclerosis in Recipients of Pediatric Donor Kidneys Hayes Et Al
Uploaded by
EricWallach0 ratings0% found this document useful (0 votes)
8 views5 pagesasd
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentasd
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
8 views5 pagesThe Development of Proteinuria and Focal Segmental Glomerulosclerosis in Recipients of Pediatric Donor Kidneys Hayes Et Al
The Development of Proteinuria and Focal Segmental Glomerulosclerosis in Recipients of Pediatric Donor Kidneys Hayes Et Al
Uploaded by
EricWallachasd
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 5
November 1991
REFERENCES
1. Anuras 8, Piros J, Bonney W, Forker EL, Colville DS, Corry RJ.
Liver disease in renal tranaplant recipients. Arch Intern Med
197%; 197: 42.
2, Debure A, Degos F, Pol S, etal. Liver diseases and hepatic com:
plications in renal transplent patients. Adv Nephrol 1988; 17:
315,
3. Parfrey PS, Forbes RDC, Hutchinson TA, et al. The impact of
‘enal transplantation on the couree of hepatitis B liver disease.
‘Transplantation 1985; 39: 610.
4, Weissberg JI, Andres LL, Smith Cl, et al. Survival in chronic
hepatitis B: an analysis of 379 patients, Ann Intern Med 1984;
101: 613,
5, Ware AJ, Luby JP, Hollinger B, etal. Etiology of liver disease in
renal transplant patients, Ann Intern Med 1973;
6, Boyce NW, Holdsworth SR, Hooke D, Thomson NM, Athi
'Non-hepattis B associated liver divease in a rensl transplant
population. Am J Kidney Dis 1988; 4: 07,
1. Kuo G, Choo QL, Alter Hi etal. An assy for circulating antibodies
to a major etiologic virus of human non-A non-B hepatitis.
Science 1989; 244 362,
041-1337/9/6206-0813808.00/0,
‘TransPtantaron
Copyright © 1881 by Wiliams & Wilkine
HAYES ET AL.
813
8, Yeoh EK, Chang WK, Kwan JPW. Epidemiology of viral hepatitis
B infection in Hong Kong. In: Lam SK, ed. Viral hepatitis B
infection in the western Pacific region’ vaccine and contro
Singapore: World Scientifie, 1984: 38.
9, Pons F, CempistolJ, Barrera J, et al. Incidence and role of hepatitis
(C virus (HCV) in liver disease of renel transplant patients
[Abstract]. Abstesct no. 434, 13th International Congress of the
‘Transplantation Society, Sen Francisco, August, 1990.
10, Pot 8, Legendre C, Saltiel C, et al. Hepatitis C virus in kidney
‘recipients: epidemiology; impact on renal transplantation (Ab:
Abstract. no. 403, International Symposium on Viral
Hepatitis and Liver Disease, Houston, 1990,
1, Alter HJ, Purcell RH, Shik JW, et al. Detection of antibody to
hepatitis C virus in prospectively followed transfusion recipients
with acute and chronic non-A non-B hepatitis, N Engl J Med
12, Huang CC, Lai MK, Fong MT. Hepatitis B liver disease in cyclo-
sporine-treated renal allograft recipients. Transplantation 1990;
49: 540,
Received 20 December 1990,
Accepted 22 March 1991
Vol 52, 819-817, No. 5, November 1991,
Prntedin CSA
THE DEVELOPMENT OF PROTEINURIA AND FOCAL-
SEGMENTAL GLOMERULOSCLEROSIS IN RECIPIENTS OF
PEDIATRIC DONOR KIDNEYS
Josep M. Hayes,
* Donatp R. STEINMULLER,’ STEVAN B. STREEM’ AND ANDREW C. Novick!
Departments of Urology and Hypertensian/ Nephrology, The Organ Transplantation Center, The Cleveland Clinie Foundation,
Several reports in animals, and sporadic case reports
in humans, have suggested that kidneys with decreased
nephron mass may be more susceptible to the develop-
ment of focal-segmental glomerosclerosis. ‘Thi
prompted a reexamination of our previously reported
group of pediatric donor-adult recipient renal tran:
plant combinations. Data were analyzed from 31 adult
recipients who had received renal transplants from ca-
daver pediatric donors (<6 years) with graft function
for >6 months and no evidence of chronic rejection.
‘These were compared with a control group transplanted
during the same period with adult donor kidneys. Im-
munosuppression consisted of azathioprine/prednisone
or quadruple therapy in 16 and 15 patients respectively.
End-stage renal disease (ESRD) was secondary to
chronic glomerulonephritis (n=9), diabetes mellitus
(n=6), polycystic kidney disease (n=5), and miscell
neous causes (n=11). Twenty patients had radiographic
documentation of renal hypertrophy posttransplant. All
* Department of Urology
* Address correspondence to: Joseph M. Hayes, M.D., The Cleveland
(Clinic Foundation, 9500 Euclid Ave, Desk A100, Cleveland, OH 44195.
Department of Hypertension/Nephrolog.
(Cleveland, Ohi 44106
patients had serial 24-hr urinalysis for protein and cre-
atinine after transplantation during periods of stable
renal function, Ten patients had renal biopsies per-
formed at a mean time from transplant to biopsy of
10.441.6 months. Seven recipients had biopsies that
revealed glomerulosclerosis at 1346 months posttrans-
plant. Protein excretion and serum creatinine in these
Patients were significantly higher than in control pa
tients (1.6£0.37 vs. 0.49+0.15 g/24 hr and 1.96+0.11
‘ya. 1,640.08 mg%: P<0.03 and P<0.01, respectively).
Only 3 of 25 control adult donor recipients developed
proteinuria > 0.8 g/24 hr within 2 years of transplan-
tation vs. 16/31 pediatric donor recipients. No correl
tions with the etiology of ESRD, age (>or< 40 years),
weight, sex, diabetes, hypertension, or the number of
acute rejection episodes could be found. Our data suggest
that adult recipients of pediatric donor renal transplants
may be at greater risk for the development of glomeru-
losclerosis than those recipients receiving adult donor
kidney:
‘The rapidly widening gap between the number of patients
‘awaiting solid organ transplants and the availability of donor
‘organs has prompted many transplant centers to reevaluate
814
and expand their criteria for donor acceptability. The use of
pediatric cadaver donor kidneys has remained controversial
and discrepant results continue to be reported'(1-5). We have
previously reported our experience over the past decade utiliz:
ing these kidneys (6), and have found sequential immunosup-
pressive therapy to improve results when utilizing kidneys from
donors under 6 years of age. The enhanced protection from
‘both ischemic insult and rejection may be of critical importance
in this situation with perhaps less than adequate functional
renal reserve. Concerns regarding an inadequate nephron mas
when these small kidneys are transplanted into adults have
‘been cited by some authors who advocate en bloc transplanta-
tion of both kidneys (8-10),
‘Several reports have highlighted a potential long-term path-
logic change in the kidney with an inadequate nephron m
that is, the development of progressive glomerulosclerosis,
(GS).* Studies in animals (11-13) and sporadic reports in
hhuman (14-17) have suggested an enhanced susceptibility to
the development of GS both in kidneys from younger individ.
‘uals and in individuals with decreased nephron mass, These
studies have prompted us to reexamine our transplant recipi
‘ents who received pediatric cadaver kidneys from donors under
6 years of age.
MATERIALS AND METHODS
Patients. Between May 1977 and June 1987 57 uremic adult patients
received renal transplants utilizing kidneys procured from pediatric
‘eadaver donors aged 0 to 6 years. A group of 25 adult donor (> 16 years
‘of age) renal transplant recipients matched for immunosupprestion,
‘time period of transplantation, recipient ag, histocompatibility, total
and warm ichemia time, incidence of rejection, and diabetic and
retransplant status, served as controls.
Protocols for perioperative and postoperative care. All kidneys were
harvesteden block from heart-beeting cadaver donors and transplanted
1a single units. Ureteroneoeystostomy was performed in all cases
Simple cold storage with Collin solution was used for preservation
Immunosuppression consisted of either conventional therapy with
‘azathioprine, prednisone, and prophylactic antilymphocyte globulin or
sequential therapy utilizing low-dose azathioprine, prednisone, tnd
prophylactic ALG, with conversion to cyclosporine aa previously de
scribed (6). Rejection episodes were treated with intravenous methyl
prednisolone 1.5 g in divided doses and/or ALG (10-20 mg/kg) of
OKTS (5 mg) for 10 days. Renal function was assessed by serum
creatinine, creatinine clearance, and/or glomerular filtration rates by
ts modification of the method of Iaraelit et al. (18). Renal biopsies
‘obtained after the initial 6-month posttransplant period were per
formed in patients with relatively rapid deterioration in renal function
to rule out rejection, or in patients with increasing proteinuria with oF
without stable renal function,
Eligibility criteria, All pediatric cadaver donors had
function and no history of proteinuria or underlying renal
to the many preexisting factors in this study population that might
influence the interpretation of data leading to a diagnosis of GS
posttransplantaton, strict criteria were established for patient entry
into both study and control groups. Patients in whom the etiology of
‘end-stage renal disease (ESRD) could result in the development of
{ocal and/or segmental GS, such aa Fabry's disease, Alpor's syndrome,
oF preexisting GS, were excluded from analysis, Those patients in
whom chronic rejection was suspected by biopsy and a history of
sraduilly deteriorating renal function, estociated temporally with in
‘reasing proteinuria and the development or worsening of hypertension,
were excluded. In most cases these clinical erteria were accompanied
* Abbreviations: ACE, angiotensin-converting enzyme; ESRD, end:
stage renal disease; GS, glomerulosclerosis,
"TRANSPLANTATION
Vol. 52, No.5
by pathologie changes such as vasculitis, ibrin-platelet deposits, sub-
endothelial membranous material deposits, and the absence of foot
process loss and capillary loop collapse on electron microscopy. Those
‘whose biopsies were performed to confirm clinically suspected acute
rejection were exclude.
Patients entered into the analysis had to have no evidence of acute
‘or chronic rejection by the above erteria. Adequate laboratory data
defined as seriel measurements of serum creatinine, creatinine clear.
tance, and 24-hr urinary protein excretion were required. In order to
enture the adequacy ofthe 24-hr urine collection, the specimen had to
contain between 10 and 25 mg of eretinine per kg body weight.
Pathologic criteria used forthe diagnosis of GS included the follow-
ing: focal or segmental GS and/or hyalinosis with minimal or no
pathologic changes in the nonsclerotic glomeruli; tubular lose end
interstitial fibrosis; and immunofluorescence studies revealing focl
and segmental granular deposits of IgM and C in the mesangial regions
of glomeruli. Electron microscopic criteria included foot process fusion
and lose, wrinkled and thickened glomerular capillary basement mem:
branes in the areas of sclerosis, and capillary lop collapse.
‘Statistical methods. Compariton between demographic and disease
history variables, as well as rejection incidence, were analyzed by
Student's ¢ test. Appropriate two-way tables for categorical variables
were developed, with ci-squere analyses ured to test for independence
(19). When sample size was small, andthe expected cll frequency wa
leas than five, the Fisher's exact test was used for analysis (20).
RESULTS
Patient entry and clinical characteristics, Established eligibil-
ity criteria were met by 31 of 57 adult recipients of renal
transplanta utilizing kidneys from pediatric donors age 0-6
years, Summary data on demographic factors, immunosuppres-
ion, and pertinent medical history, including the etiology of
ESRD and the incidence of retransplantation, are shown in
Table 1. The period of follow-up from transplantation was
comparable for the study and control patients. There were no
statistically significant differences noted for recipient age, di-
abetic or retransplant status, or the type of immunotuppres-
ion. In addition, ischemia time and the degree of histocompat-
ibility were similar. No statistically significant correlations
existed between any of the variables in Table 1 and subsequent
proteinuria and/or GS.
‘Rejection and hypertension. Patients in whom historical and/
or pathologic evidence confirmed or suggested a diagnosis of
chronic rejection were eliminated from consideration. Twenty-
‘two and 13 recipients in the study and control groups respec-
tively had one or more acute rejection episodes. This difference
‘was not statistically significant, In the study group 1, 8, and 13
recipients experienced 3, 2, and 1 acute rejection episodes
respectively. In 19 of these 22 patients renal function returned
episodes respectively. In 19 of these 22 patients renal function
returned to baseline after antirejection therapy. Three of the 8
recipients with two rejection episodes lost their grafte as a
result of the second rejection episode. In no recipient was the
development of proteinuria or a diagnosis of GS temporally
related to an acute rejection episode. It is of note that 5
recipients subsequently found to have proteinuria did not have
clinically evident rejection episode. While no significant
correlations were noted between acute rejection episodes and
the subsequent development of GS or proteinuria, « trend
toward an association between rejection and proteinuria may
be present (P=0.06).
Hypertension was present in 14 study group recipients post-
‘transplant. In 3 of these patients the hypertension was stable
‘comparison to pretransplant, and in 11 patients hypertension
[Noversber 1991
‘Tanue 1. Demographic and clinical characteristics of patients
receiving pediatric (study) and adult (control) donor renal transplants
ody BT)
Sex (M/F) 20/11
Recipient age (years)* 374223
Donor age (years)* 33203
‘Time of follow-up 295236
months)"
No. with prior transplants 2
No. with eyclosporine im 15 u
‘munosuppression
Btiology of ESRD
Diabetes mellitus 6 u
Polyeyatic kidney dis 5
(Chronic glomeruloneph- °
tits
Miscellaneous (eg, con- n 6
either developed or worsened posttransplant. Two of these 11
patients were subsequently found to have renal artery stenosis
that responded to percutaneous transluminal angioplasty. Hy
pertension was treated with angiotensin-converting enzyme
(ACE) inhibitors, in conjunction with other antihypertensives,
in 4 patients, and with beta blockers in an additional 3 patients.
‘Twenty-two control group recipients had hypertension post
‘transplant. In 9 of these patients hypertension either developed
‘or worsened posttransplant. ACE inhibitors were utilized as
antihypertensive therapy in 10 of the 22 recipients.
‘No correlations existed between the incidence, severity, or
development of hypertension, or antihypertensive therapy with
or without ACE inhibitors, and the subsequent development of
proteinuria and/or GS. However, a possible trend between
hypertension and the subsequent development of proteinuria
and GS was evident (P=0.08 and P=0.07 respectively). Four
recipients who developed GS had hypertension, and three of
these patients were being treated with ACE inhibitors, while
the remaining patient received a beta blocker. In 2 of 4 recipi-
ents with hypertension and GS, the hypertension was stable
relative to the pretransplant period.
Renal function, proteinuria, and glomerulaselerosis. All recip
ients of pediatric kidneys who were studied early after trans
plantation with ultrasound or CT imaging subsequently under.
‘went a later, repeat study to determine if renal hypertrophy
hhad occurred. In all patients studied (n=20) significant hyper
trophy had occurred, with the kidney doubling, or even tripling,
in estimated volume. In examining the entire group of selected
study patients, a significant difference was noted in serum
creatinine compared with that of control patients, While the
creatinine clearance and GFR performed in a smaller cohort
were not statistically different from those of controls, a trend
toward decreased renal function in the study group is suggested
by the data summarized in Table 2. The serum creatinine for
recipients with GS on biopsy (n=7) and for all recipients with
proteinuria (n=15) was similar to that in the entire study group
(1,910.12, 1,970.17, and 1.96:0.11 respectively).
“Measurements of urinary protein in both study and control
patients was analyzed only during periods of stable renal fune-
tion, that is, in the absence of rejection and of medical or
surgical complications. Data regarding proteinuria in study and
HAYES ET AL.
815
control patients are summarized in Table 3. Urinary protein
fexeretion per 24 hr was significantly greater in the study vs,
control group recipients, Protein excretion greater than 08 g/
24 hr was noted in 15 of 31 study recipients vs. 3 of 25 control
recipients (P<0.01). One control patient with poorly controlled
diabetes, and hypertension treated without ACE. inhibitor
excreted 4g of protein/24 hr and had a stable serum creatinine
Of L8 mg after 8 years of follow-up. Proteinuria in this patient
may have been secondary to recurrent diabetes and exacerbated
by hypertension. All patients with proteinuria, with proteinuria
and no biopsy, and with evidence of GS on biopsy, had signif.
‘cantly inereased urinary protein excretion compared with con
trol patients
Seven recipients were found to have evidence of GS on renal
biopsy performed at a mean time posttransplant of 10.481.6
months. In 3 ofthese recipients renal biopay was performed to
assess an increase in serum creatinine of 0.5 mgt over a 2
‘month period The mean serum creatinine in these 3 recipients
twas 1.7 mg% (range 1.4-2.0 mg%). The remaining 4 recipients
had stable renal function at the time of biopsy, with a mean
serum crentinine of 2.1 mg% (range 1.8-2.3 mp’), and under-
went biopsy ostensibly to assess incressing proteinuria Four
af the 7 patients hed studies posttransplant documenting sig
nificant hypertrophy of the renal transplant
‘The etiology of ESD in these 7 patients was congenital
anomaly or anatomic abnormality (e.g., vesicoureteral reflux
with chronic pyelonephritis) in 4 patienis, and polycystic kid-
ney disease, chronic glomerulonephritis, and diabetes mellitus
in one patient each. ‘The patient with diabetes was well con-
trolled, had his renal biopsy performed at 13 months posttrans-
plantation, and had no evidence ofthe nodular type of GS on
biopsy
Five of these 7 patients with GS had one rejection episode,
which was mild and reversed without impairment in renal
funetion. The remaining 2 patients had two rejection episode
TABLE 2 Assessment of renal function in study and control
ecipients
Study (aS) Control (26) P vue
Renal hypertrophy 20/81
Serum creatinine 1962011 164x009 0.08
(amg’ey"
Creatinine clearance 425845 © L785.2 NSP
(ini/min)
GFR (ml/min) 419245 578104 NS
t
1)
Mean = SEM.
NS: not significant
Tams
Proteinuria im study and control patients
Urinary pro: tein (pes Urinary pro
Urinary pr
teintallpa tentawth tein pe
‘ein tll pa 7
infall PO. ent with proteinuria tents with
ents) proteinuria) ander GS
Study (6/24 337K062 0080.77 2612109
(n=i5) (nell)
1952091
(n=3)
0.05,
816
‘While renal function returned to baseline after the first rejec-
tion episodes, these 2 recipients subsequently lost their allo-
‘rafts to second acute rejection episodes occurring greater than
1 year posttransplant,
DISCUSSION,
‘The concept that @ decrease in the number of functioning
nephrons, beyond an unknown critical limit, may lead to glo-
merular hyperfltration was introduced over 50 years ago (2!)
‘That this physiological adaptation may induce a functional
overload on the remaining renal units, with resultant detrimen-
tal glomerular changes, has been suggested from animal studies
(11, 22, 23). Hostetter et al., based on substantial experimental
evidence, have proposed that this compensatory hyperfiltration
‘may be maladaptive and result in progressive renal injury (22,
23). The work of Olson et al. further supported this hypothesis
by demonstrating in rate that a significant reduction in renal
‘mass resulted in the remnant glomeruli developing various
functional defects such as capillary membrane disruption with
resultant loss of size and charge-selectivity (24). Proteinuria
‘appears to be the hallmark of this glomerulopathic process. It
‘appears that after a critical reduction in renal mass, progressive
destruction of remnant glomeruli occurs, possibly involving
several common pathways, one of which is hyperfiltration of
residual renal units, In addition, protein may independently
influence renal hemodynamics and play a significent role in
pathogenesis, Studies in both animals and humans have dem-
‘onstrated an increase in renal mass, GFR, and renal blood flow
after protein feeding (25-28). Kiprov et al. reported the devel
‘opment of proteinuria and subsequent focal/segmental glomer-
ulosclerosis in surgical pathology and autopsy specimens from
patients with solitary kidneys (14). Thorner et al. described
similar pathologic findings in three children with solitary kid-
neys and chronic renal failure (15). Various case reports have
0 illustrated these abnormalities after surgical removal of
178% of functioning renal mass (29, 30).
Identifying the abnormal development of proteinuria and/or
GS in the setting of renal transplantat
problems. Proteinuria is frequently associated with various
pathologic development post-renal transplantation. GS may
be the primary etiology of ESRD, or secondary to a number of
diseases leading to ESRD such as Alport’s eyndrome, Fabry’s
disease, or primary focal-segmental GS. In addition, other
clinical and pathologic findings in chronic rejection and/or
cyclosporine nephrotoxicity may be similar, although not iden-
tical, to those noted with the development of focal-segmental
bility criteria were established in an attempt to
interpretation of proteinuria or identification of GS
ient population,
‘While the transplantation of pediatric donor kidneys into
adult recipients results in a decreased renal mass relative to
patient size, and may enhance the development of proteinuria,
or GS, pedistric donor kidneys may be inherently more suscep-
tible to these pathologic developments. Okuda et al. found
significantly increased compensatory hypertrophy, proteinuria,
‘and focal glomerulosclerosis in younger rats undergoing uni:
‘nephrectomy (13). While there have been reports with long-
term follow-up of the successful utilization of neonatal anen-
cephalic donors (31), Leunissen et al. reported two adult recip-
iente of en-bloc neonatal kidneys who developed proteinu
tand subsequent focal glomerulosclerosis (16). Woolley et al
"TRANSPLANTATION
Vol. 52, No.8
also reported a case of nephrotic range proteinuria and de novo
focal glomerulosclerosis in an adult recipient of a single kidney
from a 6-year-old donor (17). Whether pediatric kidneys are
inherently more susceptible to this pathologic development
remains unknown. The significant differences in protein excre-
tion noted between our study and control patients, without
differences in factors that might contribute to the development
of proteinuria, further support the preceding hypotheses.
‘A decrease in the relative amount of functioning renal paren-
cchyma due to acute rejection episodes may result in posttrans-
plant proteinuria. In our study patients we were not able to
identify a correlation between acute rejection and proteinuria
‘or GS. In all acute rejection episodes occurring prior to the
identification of proteinuria there was complete reversal with
antirejection therapy, and a return to the level of previous renal
ion. In eddition, most of these rejection o
early after transplantation in a relatively small patient popu-
lation. Functioning renal mass relative to the patient's size is
difficult to as
‘on biopsy had marked compensatory hypertrophy noted, with
at least a doubling in renal volume. Furthermore, no correlation
was noted between recipient weight or donor age and the
development of proteinuria or GS. Diabetes, which may result
in nephropathy and the development of proteinuria and GS,
was present in only 1 of 7 recipients with GS and in 3 of the
15 patients with proteinuria,
Renal function, as assessed by the serum creatinine, was
ignificantly different for all study versus control patients.
However, other parameters of renal function, while suggestive
of a trend, were not significantly different from those of control
patients. It should be noted, however, that follow-up is rela
tively short (3 years), and a longer time period may be required
to demonstrate deterioration of renal function.
In summary, the impact of our findings, as they relate to the
utilization of pediatric donors for renal'transplantation, re-
mains uncertain. Certainly available experimental and clinical
‘evidence would suggest that adult recipients of smaller pediatric
donor kidneys may be at significant risk to develop glomerular
hyperfitration and proteinuria, However, the large number of
confounding variables present in the transplant setting make
GS a difficult entity to study. Further long-term studies should
ideally be done in a controlled, prospective manner with serial
biopsies to evaluate the extent and significance of this potent
complication following the transplantation of smaller pediatric
donor kidneys into adult recipients.
REFERENCES
1. Opelz G. Influence of recipient and donor age in pediatric renal
transplantation. Transplant Int 1988; 1:95.
2, Wengerter K, Matas AJ, Telli VA, Quinn T, Soberman , Veith
J. Transplantation of pediatric donor kidneys to adult recipi-
‘ents: is there a ertial donor age? Ann Surg 1986; 204: 172,
3. Ruder H, Schaefer F, Gretz N, Mohring 8, Scharer K. Donor
Kidneys of infants and very young children are unacceptable for
‘transplantation. Lancet 1988; 2: 168,
4, Fine RN. Renal traneplantation of the infant and young child and
‘the use of pediatric eadaver donor kidneys for traneplantation in
pediatric and adult recipients. Am J Kidney Dis 1988; 12:1.
8, Smith AY, Van Buren CT, Lewis RM, Kerman RH, Kahn BD.
Short-term and long-term function of cadaveric kidneys from
pediatric donors in recipients treated with cyclosporine. Trans-
plantation 1988; 45: 360.
6, Hayes JM, Novick AC, Streem SB, eta The use of singe pediatric
November 1991
cadaver kidneys for transplantation, Transplantation 1988; 45:
106.
17. Hayes JM, Novick AC, Steinmuller DR, et al. Improved results
‘using pediatric cadaver donor kidneys with cyclosporine immu-
nosuppression. Transplant Proc 1988; 20: 200.
8, Meakins JL, Smith BJ, Alexander JW. En bloc transplantation of
both kidneys from pediatric donors into adult patents. Surgery
1993; 71: 72
9, Anderson OS, Jonasson O, Merkel FK, En bloc transplantation of
pediatric kidneys into adult patients. Arch Surg 1974; 108 35.
10, Schneider JR, Sutherland DER, Simmons RL, Fryd DS, Nejarian
‘38. Long-term success with double pediatric cadaver donor renal
‘transplants. Ann Surg 1983; 197: 439,
11, Shimamura T, Morrison AB. A progrestive glomeruloscleross oc.
curring in partial five-sixths nephrectomized rats. Am J Pathol
1975; 78: 95.
12, Brenner BM, Meyer TW, Hostetter TH. Dietary protein intake
tnd the progressive nature of kidney disease: the role of hemo-
lly mediated glomerular injury in the pathogenesis of,
ive glomerular sclerosis in aging, renal ablation, and
intrinsic renal disease. N Engl J Med 1982; 307: 652
18, Okuda §, Motomura K, Sanai , otal. Influence of age on deteri
oration of the remnant kidney in uninephrectomized rats, Clin
Sci 1981; 72: 571
14, Kiproy DD, Colvin RB, McCluskey RT. Focal and segmental
lomerulosclerosis and proteinuria associated with unilateral
renal agenesis. Lab Invest 1982; 6: 276
15, Thorner PS, Arbus GS, Celermajer DS, Baumal R.Focel segmental
slomerulosclerosis and progressive renal failure associated with
‘unilateral kidney. Pediatrics 1984; 73: 806,
16, Leunissen KM, Kootstra G, Bosman PT, van Hooff JP. Focal
slomerulosclerosi in neonatal kidney graft. Lancet 1987; 2 1019.
17, Woolley AC, Rosenberg ME, Burke BA, Nath KA. De novo focal
slomeruloscleross after kidney transplantation, Am J Med 1988;
84: 310,
18. Iraclit AH, Lanz DC, White MG, Hall AZ. Measurement of GFR
utilizing @ single subcutaneous injection of [-labelled sodium
fothalemete (Gloft). Kidney Int 1973, 4:94.
HAYES ET AL.
817
19, Mantel N, Haenszel W. Statistical aspects ofthe anelyses of data
from retrospective studies of disease. INCI 1959; 2: 718.
20, Fisher RA. Statistical methods for research workers. 14th. New
York: Hafner, 1973; 96.
21, Chanutin A, Ferris E. Experimental renal inauficiency produced
by partial nephrectomy. Arch Intern Med 1932; 48: 767
22, Hostetter TH, Olson JL, Rennke HG, Venkatachalam MA, Bren-
ner BM, Hyperfitration in remnant nephrons: a potentially
‘adverse response to renal ablation. Am J Physiol 1981; 241: FBS,
28, Hostetter TH, Rennke HG, Brenner BM. Compensstory renal
‘hemodynamic injury: a final common pathway of residual neph-
zon destruction. Am J Kidney Dis 1982; 1: 310.
24, Olson JL, Hostetter TH, Rennke HG, Brenner BM, Venkatach-
‘alam MA. Altered glomerular permsclectivity and progressive
sclerosis following extreme ablation of renel mass. Kidney Int
1982; 22: 112.
25. MacKay BM, MacKay LL, Addis’T, Factors which determine renal
weight: V. The protein intake. Am J Physiol 1928; 66: 459
26, O'Connor WJ, Summerill RA. The effect of a meal of meat on
‘lomeruar filtration rte in dogs at normal urine lows. J Physiol
1976, 256: 8.
27, Pullman TN, Alving AS, Dern RJ, Landowne M. The influence of
dietary protein intake on specific renal functions in normal man
‘JLab Clin Med 1984; 44: 320
28. Cochran ST, Pagani JJ, Barbaric ZL.
‘mentation, Radiology 1979; 190: 608.
29, Solomon LR, Mallick NP, Lawler W. Progrestive renal fs
‘remnant kidney. Br Med J 1985; 291: 1610.
80, Stahl RAK, Low I, Schoeppe W. Progressive renal failure in a
patient after one and two-thirds nephrectomy. Klin Wochenschr
1988; 6: 508.
41, litaka K, Martin LW, Cox JA, McEney PT, West CD. Transplan-
tation of cadaver kidneys from anencephalic donors, J Pediatr
1978; 93 26.
pphromegaly in hyperal
Received 1 February 1981,
‘Accepted 26 March 1991,
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Michaels Hardware CaseDocument5 pagesMichaels Hardware Casesadyia carmel67% (3)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Avatar Neytiri 1Document48 pagesAvatar Neytiri 1Jheix Diniz100% (5)
- Docket 133Document387 pagesDocket 133EricWallach100% (1)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Process Costing of Sugar IndustryDocument30 pagesProcess Costing of Sugar Industrymeera bhanushali67% (24)
- Article PDFDocument50 pagesArticle PDFEricWallachNo ratings yet
- Netbill Security and Transaction Protocol Cox Tygar and SirbuDocument1 pageNetbill Security and Transaction Protocol Cox Tygar and SirbuEricWallachNo ratings yet
- 1.1 Distributed Electronic Banking: Anna, Zulfikar @theory - Lcs.mit - EduDocument14 pages1.1 Distributed Electronic Banking: Anna, Zulfikar @theory - Lcs.mit - EduEricWallachNo ratings yet
- Consumer Survey of WWW Users: No Claims About Representativeness of The Web Population Are Made. Please See TheDocument30 pagesConsumer Survey of WWW Users: No Claims About Representativeness of The Web Population Are Made. Please See TheEricWallachNo ratings yet
- Canadian "Freeman-on-the-Land" Meeting & Resource GuideDocument3 pagesCanadian "Freeman-on-the-Land" Meeting & Resource GuideEricWallachNo ratings yet
- Dolly Varden Silver CorpDocument3 pagesDolly Varden Silver CorpEricWallachNo ratings yet
- The Politic: Why Is The Pie Fallacy So Prevalent? Why Do So Many Even WellDocument3 pagesThe Politic: Why Is The Pie Fallacy So Prevalent? Why Do So Many Even WellEricWallachNo ratings yet
- The Wal-Mart School of MusicDocument7 pagesThe Wal-Mart School of MusicEricWallachNo ratings yet
- Voelker SecurityDocument68 pagesVoelker SecurityEricWallachNo ratings yet
- Rank University Score CountryDocument6 pagesRank University Score CountryEricWallachNo ratings yet
- Complaint Count by Practice and BusinessDocument239 pagesComplaint Count by Practice and BusinessEricWallach100% (1)
- The Destruction of The Temple and Signs of The End TimesDocument3 pagesThe Destruction of The Temple and Signs of The End TimesEricWallachNo ratings yet
- Rank University Score CountryDocument8 pagesRank University Score CountryEricWallachNo ratings yet
- Mcdonald'S Chicken Nuggets - How Do They Get The Perfect Crisp?Document3 pagesMcdonald'S Chicken Nuggets - How Do They Get The Perfect Crisp?EricWallachNo ratings yet
- To Express Duty or Moral Obligation": of BeingDocument5 pagesTo Express Duty or Moral Obligation": of BeingEricWallachNo ratings yet
- RandomsfDocument21 pagesRandomsfEricWallachNo ratings yet
- 2014 Bungee DropDocument14 pages2014 Bungee DropEricWallachNo ratings yet
- Rank University Score CountryDocument8 pagesRank University Score CountryEricWallachNo ratings yet
- Clarification - Civ Dis.Document1 pageClarification - Civ Dis.EricWallachNo ratings yet
- Nonsolvent ExtractionDocument3 pagesNonsolvent ExtractionHachubeeNo ratings yet
- Overview of Common Nutritional Disorders of Captive Reptiles PDFDocument9 pagesOverview of Common Nutritional Disorders of Captive Reptiles PDFDhasiaNo ratings yet
- CRH Dietary Policies and Procedures.11.2014 Final PDFDocument325 pagesCRH Dietary Policies and Procedures.11.2014 Final PDFShivanipandey100% (2)
- RHA - Open Cut Piping & Manhole Iinstallation (Page 4)Document5 pagesRHA - Open Cut Piping & Manhole Iinstallation (Page 4)tanaNo ratings yet
- Jacobi Water Services PDFDocument15 pagesJacobi Water Services PDFHamed ArianNo ratings yet
- 51 - Nityam Bhagavata Sevaya - Issue 51 - 2016-12-10 PDFDocument9 pages51 - Nityam Bhagavata Sevaya - Issue 51 - 2016-12-10 PDFg_sanilkumarNo ratings yet
- 34 - G R - No - 213486-DigestDocument2 pages34 - G R - No - 213486-DigestNaomi InotNo ratings yet
- Stealth Viruses - The Rife ForumDocument4 pagesStealth Viruses - The Rife ForumpaulxeNo ratings yet
- V 01Document7 pagesV 01SamuelMadailNo ratings yet
- New Ballard ScoreDocument39 pagesNew Ballard ScoreJAMES ROD MARINDUQUENo ratings yet
- FIITJEE Admission Tests '2013Document4 pagesFIITJEE Admission Tests '2013FIITJEE Mumbai Centre100% (4)
- SPN Cement Lost Circulation SystemDocument2 pagesSPN Cement Lost Circulation SystemDoni KurniawanNo ratings yet
- Water: Carah Fe Bacus, RNDocument24 pagesWater: Carah Fe Bacus, RNcoosa liquorsNo ratings yet
- 2021版MobiEye 700 H-046-007582-01 DR60使用说明书(英文)-153-200Document48 pages2021版MobiEye 700 H-046-007582-01 DR60使用说明书(英文)-153-200javo599No ratings yet
- FM200Document20 pagesFM200Matthew BennettNo ratings yet
- Fire Safety in The Home - JGDocument2 pagesFire Safety in The Home - JGJamieGillumNo ratings yet
- Justification From SB 1317 and HB64Document4 pagesJustification From SB 1317 and HB64robinrubinaNo ratings yet
- MGTC Annual Report 2021Document188 pagesMGTC Annual Report 2021Jenny AbdullahNo ratings yet
- Biology 1 and 2 K12Document12 pagesBiology 1 and 2 K12ewwwNo ratings yet
- 105.a.0 - RO-DM Plant Chain Sizing CalcDocument7 pages105.a.0 - RO-DM Plant Chain Sizing Calcmkchy12No ratings yet
- Practice Problems For Thermal Engineering: September 2019Document24 pagesPractice Problems For Thermal Engineering: September 2019Roderick VillanuevaNo ratings yet
- 6242 01 Que 00070118Document16 pages6242 01 Que 00070118a盈仪No ratings yet
- Personal Financial Planning: Presented byDocument11 pagesPersonal Financial Planning: Presented byNeha Sathaye100% (1)
- Stellant DualDocument3 pagesStellant DualAlexandra JanicNo ratings yet
- Tax Calculator FormulaDocument5 pagesTax Calculator FormulaKerwin Lester MandacNo ratings yet
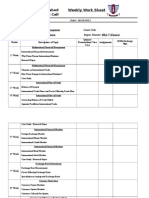
- GC University, Faisalabad Weekly Work Sheet Quality Enhancement CellDocument4 pagesGC University, Faisalabad Weekly Work Sheet Quality Enhancement CellRizwan YousafNo ratings yet
- 7060 MsDocument388 pages7060 MsXenon Diaz PalaciosNo ratings yet