Professional Documents
Culture Documents
Acid-Base Disorders Worksheet Guide
Uploaded by
Beck33ers5826Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acid-Base Disorders Worksheet Guide
Uploaded by
Beck33ers5826Copyright:
Available Formats
Acid-Base Disorders Worksheet
Step #1: Gather the necessary data (a P1 and an ABG).
Preferably, these values are all obtained from the same blood sample. At
WRAMC, ordering an ABG and a P1 (Chem 7) will give you all of the
information you need.
pH
pCO2
pO2
HCO3
Step #2: Look at the pH. If it is > 7.4, then pt has primary alkalosis, proceed to
Step 3a. If pH < 7.4, then pt has primary acidosis, proceed to step 3b.
Patient has primary:
acidosis
| alkalosis
Step #3: Look at the PCO2.
3a: If PCO2 is > 40, then pts alkalosis is metabolic; if < 40 then respiratory.
3b: If PCO2 is > 40, then pts acidosis is respiratory; if < 40, then metabolic.
Process is:
respiratory | metabolic
Step #4: Check if patient has a significant anion gap (> 12-18). (Formula for
this is: Na Cl HCO3.) If they do, then they have a metabolic acidosis in
addition to (or confirmatory of) whatever Steps #1 and #2 yielded. If no
significant gap, then skip to Step #6.
Patient has | does not have
metabolic acidosis.
Step #5: Calculate the excess anion gap. (Pts gap 12 + pts serum bicarb)
If gap excess > 30, then pt has an underlying metabolic alkalosis in addition to
whatever disorders Steps #1 through #4 yielded.
If gap excess < 23, then pt has an underlying metabolic acidosis in addition to
whatever disorders Steps #1 through #4 yielded.
Patient has underlying
metabolic:
acidosis
| alkalosis
Step #6: Figure out whats causing the problem(s), using the differentials below.
Anion Gap
Metabolic Acidosis
Non-Gap
Metabolic Acidosis
Acute Respiratory
Acidosis
Metabolic
Alkalosis
Respiratory
Alkalosis
MUDPILERS
HARDUPS
anything that causes
hypoventilation, i.e.:
CLEVER PD
CHAMPS
Methanol
Uremia
DKA/Alcoholic KA
Paraldehyde
Isoniazid
Lactic Acidosis
Etoh/Ethylene Glycol
Rhabdo/Renal Failure
Salicylates
Hyperalimentation
Acetazolamide
Renal Tubular Acidosis
Diarrhea
Uretero-Pelvic Shunt
Post-Hypocapnia
Spironolactone
Contraction
Licorice*
Endo: (Conns/
anything that causes
hyperventilation, i.e.:
Cushings/Bartters)*
CNS disease
Hypoxia
Anxiety
Mech Ventilators
Progesterone
Salicylates/Sepsis
CNS Depression
(drugs/CVA)
Airway Obstruction
Pneumonia
Pulmonary Edema
Hemo/Pneumothorax
Myopathy
(Chronic respiratory
acidosis is caused by
COPD and restrictive
lung disease)
Vomiting
Excess Alkali*
Refeeding Alkalosis*
Post-hypercapnia
Diuretics*
*assoc with high urine CL levels
Step #7: Fix it!
Used with permission of Dr. Erik Rupard. Ref: Haber, A practical approach to acid-base disorders. West J Med 1991. Aug; 155:146-151. Last revised June 10, 2009.
You might also like
- Arterial Blood Gas Analysis - making it easyFrom EverandArterial Blood Gas Analysis - making it easyRating: 4.5 out of 5 stars4.5/5 (4)
- Monitoring and Intervention for the Critically Ill Small Animal: The Rule of 20From EverandMonitoring and Intervention for the Critically Ill Small Animal: The Rule of 20No ratings yet
- 8-Step Guide To ABG Analysis - Tic-Tac-Toe Method - NurseslabsDocument10 pages8-Step Guide To ABG Analysis - Tic-Tac-Toe Method - Nurseslabsபிரேம் குமார் ராஜாமணி100% (2)
- Acid Base Balance: Carol Johns, MSN, RNDocument36 pagesAcid Base Balance: Carol Johns, MSN, RNkatrinasdNo ratings yet
- Congenital Heart DefectsDocument1 pageCongenital Heart DefectsBeck33ers5826No ratings yet
- Arterial Blood Gas AnalysisDocument43 pagesArterial Blood Gas AnalysisLoribel Coma100% (1)
- Saumya Gupta Moderator: Dr. Vishal GuptaDocument41 pagesSaumya Gupta Moderator: Dr. Vishal Guptaimranqazi11No ratings yet
- Acid Base BalanceDocument46 pagesAcid Base Balanceleesteph78No ratings yet
- Interpretation of Arterial Blood Gases (Abgs) I David A. Kaufman, MD DDocument17 pagesInterpretation of Arterial Blood Gases (Abgs) I David A. Kaufman, MD DingridpuspitaNo ratings yet
- Pediatrics Clerkship Shelf ReviewDocument78 pagesPediatrics Clerkship Shelf Reviewlcaskidsn12s100% (1)
- American Thoracic Society - Interpretation of Arterial Blood Gases (ABGs)Document8 pagesAmerican Thoracic Society - Interpretation of Arterial Blood Gases (ABGs)muhammadridhwanNo ratings yet
- Acid Base Disorders JAPIDocument5 pagesAcid Base Disorders JAPIVitrag_Shah_1067No ratings yet
- ABG Interpretation - ATSDocument5 pagesABG Interpretation - ATSHAMMYER ALROKHAMINo ratings yet
- Critical Heart Disease in Infants and Children PDFDocument997 pagesCritical Heart Disease in Infants and Children PDFBeck33ers5826No ratings yet
- Arterial Blood Gas AnalysisDocument28 pagesArterial Blood Gas Analysishendra_darmawan_4No ratings yet
- Interpretation of Arterial Blood Gases (ABGs)Document6 pagesInterpretation of Arterial Blood Gases (ABGs)afalfitraNo ratings yet
- Acid-Base Disorders and The ABGDocument28 pagesAcid-Base Disorders and The ABGPaul KelnerNo ratings yet
- Acid-Base Made EasyDocument14 pagesAcid-Base Made EasyMayer Rosenberg100% (10)
- A Quick Guide to Metabolic Disease Testing Interpretation: Testing for Inborn Errors of MetabolismFrom EverandA Quick Guide to Metabolic Disease Testing Interpretation: Testing for Inborn Errors of MetabolismNo ratings yet
- Blood Gas TestDocument6 pagesBlood Gas TestyudhafpNo ratings yet
- Acid Base WorksheetDocument1 pageAcid Base WorksheetMarshallMcGoughNo ratings yet
- Interpreting ABGs: A 6-Step ApproachDocument7 pagesInterpreting ABGs: A 6-Step ApproachGaby FernándezNo ratings yet
- Acid-Base Disorder CasesDocument40 pagesAcid-Base Disorder CaseslrostomeNo ratings yet
- Interpreting ABGs in 6 stepsDocument16 pagesInterpreting ABGs in 6 stepsRuby Ann Cañero HigoyNo ratings yet
- Michael Chansky Acid Base Made Easy HandoutDocument18 pagesMichael Chansky Acid Base Made Easy HandoutTeguh RamadhanNo ratings yet
- Metabolic Acidosis CasesDocument20 pagesMetabolic Acidosis CaseswiamNo ratings yet
- Arterial Blood Gas InterpretationsDocument7 pagesArterial Blood Gas InterpretationsErin TraversNo ratings yet
- Abg PrimerDocument22 pagesAbg PrimerAraceli Ecot CalunodNo ratings yet
- Chairman Rounds: Medicine I Jesse Lester, Kannan Samy, Matt Skomorowski, Dan VerrillDocument25 pagesChairman Rounds: Medicine I Jesse Lester, Kannan Samy, Matt Skomorowski, Dan VerrillFiorellaBeatrizNo ratings yet
- Abg TutorialDocument4 pagesAbg TutorialfritzroseNo ratings yet
- ABG InterpretationDocument23 pagesABG Interpretationprateekbatra0% (1)
- "Blood Gas Analysis in A Nutshell: DR Anshuman MishraDocument28 pages"Blood Gas Analysis in A Nutshell: DR Anshuman MishraMinaz PatelNo ratings yet
- Interpretasi AGDDocument129 pagesInterpretasi AGDIta SobaNo ratings yet
- ABG AnalysisDocument57 pagesABG AnalysisHardik RathodNo ratings yet
- ABG AnalysisDocument46 pagesABG Analysisregole100% (1)
- Michael Chansky Acid Base Made Easy Handout PDFDocument18 pagesMichael Chansky Acid Base Made Easy Handout PDFAustine OsaweNo ratings yet
- Abg Analysis & Acid-Base Disorders: DR - Anitha KsDocument24 pagesAbg Analysis & Acid-Base Disorders: DR - Anitha KsanithaNo ratings yet
- So What Does The Blood Gas Analysis Actually Measure?Document12 pagesSo What Does The Blood Gas Analysis Actually Measure?Veterinarska Bolnica Zavetišče BrežiceNo ratings yet
- Arterial Blood Gas Analysis ExplainedDocument52 pagesArterial Blood Gas Analysis Explainedimranqazi11No ratings yet
- AbgDocument7 pagesAbgChin ChanNo ratings yet
- GasometriaDocument8 pagesGasometriaEslândia SampaioNo ratings yet
- Acid-Base MSC CasesDocument16 pagesAcid-Base MSC Casesmonday125No ratings yet
- Acid-Base Disturbance in a Man with Alcoholic Liver Disease and HypotensionDocument92 pagesAcid-Base Disturbance in a Man with Alcoholic Liver Disease and HypotensionManmeet SNo ratings yet
- The Acid Base Balance: Faculty of Medicine Anesthesia and Intensive Care DepartmentDocument36 pagesThe Acid Base Balance: Faculty of Medicine Anesthesia and Intensive Care DepartmentCamelia A. ParuschiNo ratings yet
- Kursus Critical Care Respiratory FunctionDocument63 pagesKursus Critical Care Respiratory FunctionJeyaganesh SellvarajuNo ratings yet
- American Thoracic Society - Interpretation of Arterial Blood Gases (ABGs)Document7 pagesAmerican Thoracic Society - Interpretation of Arterial Blood Gases (ABGs)humberto_2No ratings yet
- ABG InterpretationDocument64 pagesABG InterpretationSiva RamanNo ratings yet
- Moderator: Dr. R. K. Yadav (MD) Presented By: Ashish JaisawalDocument47 pagesModerator: Dr. R. K. Yadav (MD) Presented By: Ashish Jaisawalimranqazi11No ratings yet
- Acid - Base BalanceDocument41 pagesAcid - Base BalanceEgun Nuel DNo ratings yet
- Acid BaseDocument6 pagesAcid BaseJoshua Adam SultanNo ratings yet
- ABG InterpretationDocument1 pageABG InterpretationtrialqwNo ratings yet
- Acid BaseDocument81 pagesAcid Basenader siamNo ratings yet
- Pneumonia - Kyphoscoliosis - Morbid Obesity - Drug OverdoseDocument3 pagesPneumonia - Kyphoscoliosis - Morbid Obesity - Drug OverdoseJessica nonyeNo ratings yet
- Acid Base PhysiologyDocument4 pagesAcid Base PhysiologyGhadeer EbraheemNo ratings yet
- Interpretation of Arterial Blood GasesDocument5 pagesInterpretation of Arterial Blood GasesRiska PashaNo ratings yet
- Acid-base Disorders ExplainedDocument12 pagesAcid-base Disorders ExplainedZafar Iqbal ManjNo ratings yet
- ABG Test ExplainedDocument29 pagesABG Test ExplainedgopscharanNo ratings yet
- Arterial-Blood Gas AnalysisDocument49 pagesArterial-Blood Gas AnalysisGovernance Book100% (1)
- KGD - Referensi Resuscitation Council (UK) ABG Analysis WorkshopDocument13 pagesKGD - Referensi Resuscitation Council (UK) ABG Analysis WorkshopAgung Nugroho OteNo ratings yet
- Blood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSIDocument39 pagesBlood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSISalsabila RahmaNo ratings yet
- Metabolic Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandMetabolic Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
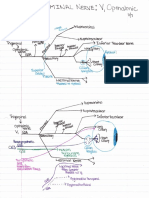
- CN 5 V1 Opthalmic NerveDocument1 pageCN 5 V1 Opthalmic NerveBeck33ers5826No ratings yet
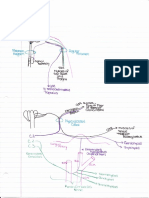
- Pharyngeal Arches 1Document1 pagePharyngeal Arches 1Beck33ers5826No ratings yet
- Neck Sympathetic ChainDocument1 pageNeck Sympathetic ChainBeck33ers5826No ratings yet
- Subclavian Artery BranchesDocument1 pageSubclavian Artery BranchesBeck33ers5826No ratings yet
- CN 11 and CN 12Document1 pageCN 11 and CN 12Beck33ers5826No ratings yet
- Block 11 Resident Education 2020Document1 pageBlock 11 Resident Education 2020Beck33ers5826No ratings yet
- CN 5 V2 Maxillary NerveDocument1 pageCN 5 V2 Maxillary NerveBeck33ers5826No ratings yet
- CN 10 VagusDocument1 pageCN 10 VagusBeck33ers5826No ratings yet
- Abdominal Arteries ChartDocument1 pageAbdominal Arteries ChartBeck33ers5826No ratings yet
- First Floor Options for Bucknell at Mews at Laurel CreekDocument1 pageFirst Floor Options for Bucknell at Mews at Laurel CreekBeck33ers5826No ratings yet
- Pulmonary Journal ClubDocument19 pagesPulmonary Journal ClubBeck33ers5826No ratings yet
- Renal Drug EffectsDocument1 pageRenal Drug EffectsBeck33ers5826No ratings yet
- Emc Campus Mapp 2012 VerticalDocument1 pageEmc Campus Mapp 2012 VerticalBeck33ers5826No ratings yet
- EKG EtcDocument1 pageEKG EtcBeck33ers5826No ratings yet
- EKG TemplateDocument3 pagesEKG TemplateBeck33ers5826No ratings yet
- EKG Page 1Document1 pageEKG Page 1Beck33ers5826No ratings yet
- Emma Holliday LecturesDocument1 pageEmma Holliday LecturesBeck33ers5826No ratings yet
- Upload 1Document1 pageUpload 1Beck33ers5826No ratings yet
- EkgsDocument3 pagesEkgsBeck33ers5826No ratings yet
- Diabetic Foot Ulcer Classification System ExplainedDocument2 pagesDiabetic Foot Ulcer Classification System ExplainedBeck33ers5826No ratings yet
- Post Op ComplicationsDocument1 pagePost Op ComplicationsBeck33ers5826No ratings yet
- Diabetic Foot Ulcer Classification System ExplainedDocument2 pagesDiabetic Foot Ulcer Classification System ExplainedBeck33ers5826No ratings yet
- Asthma ClassificationDocument1 pageAsthma ClassificationYak NafarNo ratings yet
- Try AgainDocument1 pageTry AgainBeck33ers5826No ratings yet
- Document 1Document1 pageDocument 1Beck33ers5826No ratings yet
- Renal Drug Ion Actions Cells Response 1Document1 pageRenal Drug Ion Actions Cells Response 1Beck33ers5826No ratings yet