Professional Documents
Culture Documents
Vertically Transmitted Infection
Uploaded by
dger11Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vertically Transmitted Infection
Uploaded by
dger11Copyright:
Available Formats
Vertically transmitted infection
Vertically transmitted infection
Perinatal infection
Classification and external resources
Micrograph of cytomegalovirus (CMV) infection of the placenta (CMV placentitis), a vertically transmitted infection. The characteristic large
nucleus of a CMV infected cell is seen off-centre at the bottom-right of the image. H&E stain.
ICD-10
P35
ICD-9
771
[1]
-P39
[2]
[3]
A vertically transmitted infection is an infection caused by bacteria, viruses or, in rare cases, parasites transmitted
directly from the mother to an embryo, fetus or baby during pregnancy or childbirth. It can occur when the mother
gets an infection as an intercurrent disease in pregnancy.
Nutritional deficiencies may exacerbate the risks of perinatal infection.
Classification
The transmission can also be called mother-to-child transmission.
A vertically transmitted infection can be called a perinatal infection if it is transmitted in the perinatal period, which
is the period starting at a gestational age of 22[4] to 28[5] weeks (with regional variations in the definition) and ending
7 completed days after birth.
The term congenital infection can be used if the vertically transmitted infection persists after childbirth.
Examples
Several vertically transmitted infections are included in the TORCH complex, which stands for:
1.
2.
3.
4.
5.
T Toxoplasmosis / Toxoplasma gondii
O Other infections (see below)
R Rubella
C Cytomegalovirus
H Herpes simplex virus-2 or neonatal herpes simplex
The "other agents" under O include:
Coxsackievirus
Chickenpox (caused by varicella zoster virus)
Parvovirus B19
Chlamydia
Vertically transmitted infection
HIV
Human T-lymphotropic virus
Syphilis
Hepatitis B may also be classified as a vertically transmitted infection, but the hepatitis B virus is a large virus and
does not cross the placenta, hence it cannot infect the fetus unless there have been breaks in the maternal-fetal
barrier, such as can occur in bleeding during childbirth or amniocentesis.[6]
The TORCH complex was originally considered to consist of the four conditions mentioned above, with the "TO"
referring to "Toxoplasma". The four-term form is still used in many modern references, and the capitalization
"ToRCH" is sometimes used in these contexts. The acronym has also been listed as TORCHES, for
TOxoplasmosis, Rubella, Cytomegalovirus, HErpes simplex, Syphilis.
A further expansion of this acronym, CHEAPTORCHES, was proposed by Ford-Jones and Kellner in 1995:
C Chickenpox and shingles
H Hepatitis B, C, (D), E
E Enteroviruses
A AIDS (HIV infection)
P Parvovirus B19
T Toxoplasmosis / Toxoplasma gondii
O Other (Group B Streptococcus, Listeria, Candida, Lyme disease)
R Rubella
C Cytomegalovirus
H Herpes simplex
E Everything else sexually transmitted (Gonorrhea, Chlamydia, Ureaplasma urealyticum, Human
papillomavirus)
S Syphilis
Signs and symptoms
The signs and symptoms of a vertically transmitted infection depend on the individual pathogen. It may cause subtle
signs such as a influenza-like illness and may not even be noticed by the mother during the pregnancy. In such cases,
the effects may be seen first at birth.
Symptoms of a vertically transmitted infection may include fever and poor feeding. The newborn is often small for
gestational age. A petechial rash on the skin may be present, with small reddish or purplish spots due to bleeding
from capillaries under the skin. An enlarged liver and spleen (hepatosplenomegaly) is common, as is jaundice.
However, jaundice is less common in Hepatitis B because a newborn's immune system is not developed well enough
to mount a response against liver cells, as would normally be the cause of jaundice in an older child or adult. Hearing
impairment, eye problems, mental retardation, autism, and death can be caused by vertically transmitted infections.
The mother often has a mild infection with few or no symptoms.
It is possible for genetic conditions (Aicardi-Goutieres syndrome) to present in a similar manner.
Vertically transmitted infection
Causes
The main routes of transmission of vertically transmitted infections are across the placenta (transplacental) and
across the female reproductive tract during childbirth:
Transplacental
The embryo and fetus have little or no immune function. They depend on the immune function of their mother.
Several pathogens can cross the placenta and cause (perinatal) infection. Often microorganisms that produce minor
illness in the mother are very dangerous for the developing embryo or fetus. This can result in spontaneous abortion
or major developmental disorders. For many infections, the baby is more at risk at particular stages of pregnancy.
Problems related to perinatal infection are not always directly noticeable.
During childbirth
Babies can also become infected by their mother during birth. Some infectious agents may be transmitted to the
embryo or fetus in the uterus, while passing through the birth canal or even shortly after birth. The distinction is
important because when transmission is primarily during or after birth, medical intervention can help prevent
infections in the infant.
During birth, babies are exposed to maternal blood and body fluids without the placental barrier intervening and to
the maternal genital tract. Because of this, blood-borne microorganisms (Hepatitis B, HIV), organisms associated
with sexually transmitted disease (e.g., Gonorrhoea and Chlamydia), and normal fauna of the genito-urinary tract
(e.g., Candida) are among those commonly seen in infection of newborns.
Pathophysiology
Virulence versus symbiosis
In the spectrum of optimal virulence, vertical transmission tends to evolve benign symbiosis. It is therefore a critical
concept for evolutionary medicine. Because a pathogen's ability to pass from parent to child depends significantly on
the hosts' ability to reproduce, pathogens' transmissibility tends to be inversely related with their virulence. In other
words, as pathogens become more harmful to and thus decrease the reproduction rate of their host organism, they are
less likely to be passed on to the hosts' offspring, since there will be fewer offspring.
Although AIDS is sometimes transmitted through perinatal transmission, its virulence can be accounted for by the
fact that its primary mode of transmission is not vertical. Moreover, medicine has further decreased the frequency of
vertical transmission of AIDS. The incidence of perinatal AIDS cases in the United States has declined as a result of
the implementation of recommendations on HIV counselling and voluntary testing practices and the use of
zidovudine therapy by providers to reduce perinatal HIV transmission.
The price paid in the evolution of symbiosis is, however, great: for many generations, almost all cases of vertical
transmission will continue to be pathologicalin particular if there are any other routes of transmission. It takes
many generations of random mutation and selection to evolve symbiosis. During this time, the vast majority of
vertical transmission cases will exhibit the initial virulence.[citation needed]
In Dual Inheritance Theory, vertical transmission refers to the passing of cultural traits from parents to children.
Vertically transmitted infection
Diagnosis
When physical examination of the newborn shows signs of a vertically transmitted infection, the examiner may test
blood, urine, and spinal fluid for evidence of the infections listed above. Diagnosis can be confirmed by culture of
one of the specific pathogens or by increased levels of IgM against the pathogen.
Treatment and prevention
Some of the vertically transmitted infections, such as toxoplasmosis
and syphilis, can be effectively treated with antibiotics if the mother is
diagnosed early in her pregnancy. Many of the viral vertically
transmitted infections have no effective treatment, but some, notably
rubella and varicella-zoster, can be prevented by vaccinating the
mother prior to pregnancy.
If the mother has active herpes simplex (as may be suggested by a pap
test), delivery by Caesarean section can prevent the newborn from
contact, and consequent infection, with this virus.
It has been suggested that IgG2 antibody can play crucial role in
prevention of intrauterine infections and currently extensive research is
going on for developing IgG2 based therapies for treatment and
vaccination.[7]
Micrograph of a pap test showing changes
(upper-right of image) associated with herpes
simplex virus, a vertically transmitted infection.
Prognosis
Each type of vertically transmitted infection has a different prognosis. The stage of the pregnancy at the time of
infection also can change the effect on the newborn.
Additional images
CMV placentitis.
CMV placentitis.
Vertically transmitted infection
References
[1]
[2]
[3]
[4]
http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ P35
http:/ / apps. who. int/ classifications/ icd10/ browse/ 2010/ en#/ P39
http:/ / www. icd9data. com/ getICD9Code. ashx?icd9=771
Definitions and Indicators in Family Planning. Maternal & Child Health and Reproductive Health. (http:/ / test. cp. euro. who. int/ document/
e68459. pdf) By European Regional Office, World Health Organization. Revised March 1999 & January 2001. In turn citing: WHO Geneva,
WHA20.19, WHA43.27, Article 23
[5] Singh, Meharban (2010). Care of the Newborn. p. 7. Edition 7. ISBN 9788170820536
[6] Hepatitis B (http:/ / www. who. int/ csr/ disease/ hepatitis/ whocdscsrlyo20022/ en/ index1. html) by World Health Organization (WHO),
retrieved November, 2011
[7] Syal K* and Karande AA. IgG2 Subclass Isotype Antibody and Intrauterine Infections. Current Science Vol. 102, No. 11, 10 June 2012.
Article Sources and Contributors
Article Sources and Contributors
Vertically transmitted infection Source: http://en.wikipedia.org/w/index.php?oldid=597568411 Contributors: Arcadian, Arthena, DadaNeem, Emble64, Facts707, Herbee, KillerChihuahua,
Kirtimaansyal, LT910001, Lucien504, Mikael Hggstrm, Qetuth, SingleIntegral, TenPoundHammer, Una Smith, Wouterstomp, 3 anonymous edits
Image Sources, Licenses and Contributors
File:CMV placentitis1_mini.jpg Source: http://en.wikipedia.org/w/index.php?title=File:CMV_placentitis1_mini.jpg License: Creative Commons Attribution-Sharealike 3.0 Contributors:
Nephron
Image:Herpes simplex virus pap test.jpg Source: http://en.wikipedia.org/w/index.php?title=File:Herpes_simplex_virus_pap_test.jpg License: Creative Commons Attribution-Sharealike 3.0
Contributors: Nephron
Image:CMV_placentitis1.jpg Source: http://en.wikipedia.org/w/index.php?title=File:CMV_placentitis1.jpg License: Creative Commons Attribution-Sharealike 3.0 Contributors: Nephron
Image:CMV_placentitis2.jpg Source: http://en.wikipedia.org/w/index.php?title=File:CMV_placentitis2.jpg License: Creative Commons Attribution-Sharealike 3.0 Contributors: Nephron
License
Creative Commons Attribution-Share Alike 3.0
//creativecommons.org/licenses/by-sa/3.0/
You might also like
- Feline Immunodeficiency Virus: From Diagnosis to Well-being for Cats with FIVFrom EverandFeline Immunodeficiency Virus: From Diagnosis to Well-being for Cats with FIVNo ratings yet
- TORCH MedscapeDocument17 pagesTORCH MedscapeAndrea RivaNo ratings yet
- Management of Viral Infection During Pregnancy: VaccinationDocument6 pagesManagement of Viral Infection During Pregnancy: VaccinationPOPA EMILIANNo ratings yet
- Microorganisms 09 01749Document23 pagesMicroorganisms 09 01749Ga HernandezNo ratings yet
- Cytomegalovirus Infection in Pregnancy - An UpdateDocument18 pagesCytomegalovirus Infection in Pregnancy - An UpdateBen HonorseekerNo ratings yet
- Background: Viral Infections and PregnancyDocument23 pagesBackground: Viral Infections and PregnancyStefania MarlinaNo ratings yet
- TORCH Infection in Pregnant Women Ver September 2017 PDFDocument9 pagesTORCH Infection in Pregnant Women Ver September 2017 PDFRevina AmaliaNo ratings yet
- TORCH Infections. UpToDate. Aproximacion Al DXDocument15 pagesTORCH Infections. UpToDate. Aproximacion Al DXgloriaNo ratings yet
- Correlation Between TORCH Infection On Pregnant WomenDocument32 pagesCorrelation Between TORCH Infection On Pregnant Womenmila widyastuti0% (1)
- Epidemiology of TORCH Infections and Understanding The Serology in Their DiagnosisDocument5 pagesEpidemiology of TORCH Infections and Understanding The Serology in Their DiagnosisEllya Syahfitri 2108125983No ratings yet
- Neonatal InfectionDocument18 pagesNeonatal InfectionchinchuNo ratings yet
- CMV, TOXO, Parvo, VZV in PregnancyDocument16 pagesCMV, TOXO, Parvo, VZV in Pregnancyw yNo ratings yet
- Practice Bullet In: Cytomegalovirus, Parvovirus B19, Varicella Zoster, and Toxoplasmosis in PregnancyDocument16 pagesPractice Bullet In: Cytomegalovirus, Parvovirus B19, Varicella Zoster, and Toxoplasmosis in PregnancyAyline Araceli AlavaNo ratings yet
- Tuberculosis in HIV-Infected ChildrenDocument6 pagesTuberculosis in HIV-Infected ChildrenSyaiful RizalNo ratings yet
- Infecciones Neonatale IDocument13 pagesInfecciones Neonatale IFidel RamonNo ratings yet
- CMV VirusDocument8 pagesCMV VirusKalpavriksha1974No ratings yet
- Hiv in PregnancyDocument23 pagesHiv in PregnancypuspoNo ratings yet
- Intrauterine Infection. Sepsis. Local Pyo-Inflammatory DiseaseDocument12 pagesIntrauterine Infection. Sepsis. Local Pyo-Inflammatory DiseaseIsak ShatikaNo ratings yet
- "Neonatal Infections" Lecture 1: Pediatrics Dr. Sawsan AliDocument5 pages"Neonatal Infections" Lecture 1: Pediatrics Dr. Sawsan AliAmmarNo ratings yet
- Cytomegalovirus Infection in Pregnancy: Infecção Pelo Citomegalovírus Na GestaçãoDocument5 pagesCytomegalovirus Infection in Pregnancy: Infecção Pelo Citomegalovírus Na GestaçãoDewina Dyani Rosari IINo ratings yet
- 15 Virusne Infekcije U Trudnoci - PrevedenoDocument7 pages15 Virusne Infekcije U Trudnoci - PrevedenoVelibor StankovićNo ratings yet
- Torch InfectionsDocument13 pagesTorch InfectionsOmeNo ratings yet
- RB - Aronson. I Mononucleosis. UpToDate, 2019Document36 pagesRB - Aronson. I Mononucleosis. UpToDate, 2019GuilhermeNo ratings yet
- Pelvic Inflammatory Disease - 1Document8 pagesPelvic Inflammatory Disease - 1fatqur28No ratings yet
- Congenital Cytomegalovirus Infection Clinical Features and DiagnosisDocument21 pagesCongenital Cytomegalovirus Infection Clinical Features and Diagnosisgomitas21No ratings yet
- Congenital and Perinatal Cytomegalovirus Infection: Chun Soo Kim, M.D., PH.DDocument7 pagesCongenital and Perinatal Cytomegalovirus Infection: Chun Soo Kim, M.D., PH.Dasri khazaliNo ratings yet
- Gonorrhea: SymptomsDocument9 pagesGonorrhea: Symptomspragna novaNo ratings yet
- 1995 Congenital Cytomegalovirus InfectionDocument10 pages1995 Congenital Cytomegalovirus InfectionIndra T BudiantoNo ratings yet
- 24.11.09 PPT On Intrauterine InfectionDocument57 pages24.11.09 PPT On Intrauterine InfectionDhara Meena90% (10)
- Cytomegalovirus in Pregnancy - GLOWMDocument24 pagesCytomegalovirus in Pregnancy - GLOWMLearta Asani VeliuNo ratings yet
- Communicable Diseases GIT InfectionDocument63 pagesCommunicable Diseases GIT InfectionReyadh JassemNo ratings yet
- Congenital Cytomegalovirus Infection: Current Strategies and Future PerspectivesDocument17 pagesCongenital Cytomegalovirus Infection: Current Strategies and Future PerspectivesAfif AriyanwarNo ratings yet
- Meningitis Pada AnakDocument14 pagesMeningitis Pada AnakRayhanun MardhatillahNo ratings yet
- 2 5224454212343056346-MergedDocument15 pages2 5224454212343056346-Mergedsalamalmaliki489No ratings yet
- Paediatric AIDSDocument52 pagesPaediatric AIDSvijayasree bavireddyNo ratings yet
- AIDS (Acquired Immune Deficiency Syndrome) : Biology Research WorkDocument8 pagesAIDS (Acquired Immune Deficiency Syndrome) : Biology Research WorkSarah IftikharNo ratings yet
- Anesthesia For The Pregnant HIV PatientDocument17 pagesAnesthesia For The Pregnant HIV PatientrolandoanestesiaNo ratings yet
- Acute Infections During PregnancyDocument63 pagesAcute Infections During PregnancyHussein AliNo ratings yet
- TB in Children: EpidemiologyDocument13 pagesTB in Children: EpidemiologyAdel HamadaNo ratings yet
- Home Visual Library Resources News Resources Mobile Subscribe Contact Skip To Main Page ContentDocument50 pagesHome Visual Library Resources News Resources Mobile Subscribe Contact Skip To Main Page ContentAnastasia Lilian SuryajayaNo ratings yet
- Fetal Infections and Brain DevelopmentDocument15 pagesFetal Infections and Brain DevelopmentadriricaldeNo ratings yet
- Gen Patho AIDSDocument22 pagesGen Patho AIDSJireh MejinoNo ratings yet
- Prenatal InfectionDocument7 pagesPrenatal InfectionemeyyNo ratings yet
- Infectious Mononucleosis in Adults and Adolescents - UpToDateDocument26 pagesInfectious Mononucleosis in Adults and Adolescents - UpToDateEduardo Romero StéfaniNo ratings yet
- Pelvic Inflammatory DiseaseDocument8 pagesPelvic Inflammatory DiseaseAndyan Adlu Prasetyaji0% (1)
- Acute Bacterial Meningitis During and After Pregnancy: CommentaryDocument3 pagesAcute Bacterial Meningitis During and After Pregnancy: CommentaryAyu Wedhani SpcNo ratings yet
- Toxoplasma and RubellaDocument37 pagesToxoplasma and RubellaHervi LaksariNo ratings yet
- Acquired Immune Deficiency SyndromeDocument7 pagesAcquired Immune Deficiency SyndromeHani ApiagNo ratings yet
- Bishaw Assignment NN1of TORCHDocument67 pagesBishaw Assignment NN1of TORCHRas Siko SafoNo ratings yet
- 1 - Overview of TORCH Infections - UpToDateDocument38 pages1 - Overview of TORCH Infections - UpToDateRaquel GallegoNo ratings yet
- Inrauterine InfectionsDocument83 pagesInrauterine Infectionsahmad aminNo ratings yet
- Neonatal Sepsis in The Very Low Birth Weight Preterm Infants: Part 1: Review of Patho-PhysiologyDocument10 pagesNeonatal Sepsis in The Very Low Birth Weight Preterm Infants: Part 1: Review of Patho-PhysiologyjukunkNo ratings yet
- Gonococcal Infection in The Newborn - UpToDateDocument13 pagesGonococcal Infection in The Newborn - UpToDateCarina ColtuneacNo ratings yet
- Intrauterine InfectionDocument64 pagesIntrauterine Infectionthapan87100% (1)
- 2024.sifilis CongenitaDocument12 pages2024.sifilis CongenitaWILLIAM ROSALES CLAUDIONo ratings yet
- Herpes Simplex Congenital Infections, Part I: Cytomegalovirus, Toxoplasma, Rubella, andDocument13 pagesHerpes Simplex Congenital Infections, Part I: Cytomegalovirus, Toxoplasma, Rubella, andSyahrialNo ratings yet
- MeningococcemiaDocument14 pagesMeningococcemiaMonica Marie MoralesNo ratings yet
- Pregnancy and Viral Infections Mechanisms of Fetal Damage, Diagnosis and Prevention of Neonatal Adverse Outcomes From Cytomegalovirus To SARS-CoV-2 and Zika VirusDocument18 pagesPregnancy and Viral Infections Mechanisms of Fetal Damage, Diagnosis and Prevention of Neonatal Adverse Outcomes From Cytomegalovirus To SARS-CoV-2 and Zika VirusBen HonorseekerNo ratings yet
- Luntz Wexner AnalysisDocument17 pagesLuntz Wexner Analysisdger11No ratings yet
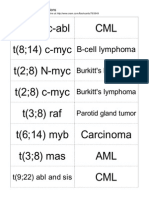
- Translocations Small00center10 765849Document5 pagesTranslocations Small00center10 765849dger11No ratings yet
- Atrophic VaginitisDocument3 pagesAtrophic Vaginitisdger11No ratings yet
- Nodular Fasciitis: Etiology and Clinical CourseDocument3 pagesNodular Fasciitis: Etiology and Clinical Coursedger11No ratings yet
- Roger Collins Early Medieval Europe 300 1000Document241 pagesRoger Collins Early Medieval Europe 300 1000dger11100% (2)
- Pneumocystis PneumoniaDocument5 pagesPneumocystis Pneumoniadger11No ratings yet
- Outlines in PathologyDocument200 pagesOutlines in PathologyLisztomaniaNo ratings yet
- Renal Cell CarcinomaDocument15 pagesRenal Cell Carcinomadger11No ratings yet
- The Psychosis-Risk SyndromeDocument256 pagesThe Psychosis-Risk Syndromedger11No ratings yet
- Royal Yucatan Villa InformationDocument3 pagesRoyal Yucatan Villa Informationdger11No ratings yet
- HHHHDocument36 pagesHHHHdger11No ratings yet
- Review Article: The Spleen Revisited: An Overview On Magnetic Resonance ImagingDocument16 pagesReview Article: The Spleen Revisited: An Overview On Magnetic Resonance ImagingrusselioNo ratings yet
- Speech DisordersDocument5 pagesSpeech DisordersRaymond LiuNo ratings yet
- Vital Signs ScriptDocument2 pagesVital Signs ScriptRed Angela Dinson100% (1)
- Factors Affecting Tendency For Drug Abuse in People Attending Addiction Treatment CentresDocument3 pagesFactors Affecting Tendency For Drug Abuse in People Attending Addiction Treatment CentresDessa Patiga IINo ratings yet
- Fetal Cystic Hygroma The Importance of Natural HistoryDocument7 pagesFetal Cystic Hygroma The Importance of Natural HistoryNGUYỄN XUÂN SangNo ratings yet
- Chapter 2 Radionuclide ImagingDocument5 pagesChapter 2 Radionuclide ImagingSri HariNo ratings yet
- Gene Therapy InfoDocument3 pagesGene Therapy InfoShailendra Singh KhichiNo ratings yet
- Pe 9 q1 w1 Answer KeyDocument8 pagesPe 9 q1 w1 Answer KeyRAYMOND ADLAONNo ratings yet
- Removal of Stuck Femur Interlocking Nail by Longitudinal Osteotomy of Femur - A Case ReportDocument4 pagesRemoval of Stuck Femur Interlocking Nail by Longitudinal Osteotomy of Femur - A Case ReportIJAR JOURNALNo ratings yet
- The Cornea PPT EditDocument38 pagesThe Cornea PPT EditRahman Setiawan100% (1)
- DeathDocument42 pagesDeathEunice ChavezNo ratings yet
- Aneurysmal Subarachnoid Hemorrhage Nursing Self-Paced Case StudyDocument100 pagesAneurysmal Subarachnoid Hemorrhage Nursing Self-Paced Case StudyAndi rahma AnugrahNo ratings yet
- Health Certificate For COVID-19: Roshan Kumar Shah Male 29 04/04/1992 Nepal 11247987Document1 pageHealth Certificate For COVID-19: Roshan Kumar Shah Male 29 04/04/1992 Nepal 11247987Roshan ShahNo ratings yet
- ADHD Psychoeducation Information For Parents Schools and CliniciansDocument2 pagesADHD Psychoeducation Information For Parents Schools and CliniciansJudit BerkiNo ratings yet
- Proton Therapy Coverage LawsuitDocument47 pagesProton Therapy Coverage LawsuitAlex KacikNo ratings yet
- Going To The DoctorDocument4 pagesGoing To The DoctorJarod TempleNo ratings yet
- Sexually Transmitted Diseases: PresentationDocument17 pagesSexually Transmitted Diseases: PresentationBonface NdunguNo ratings yet
- List of HCOsDocument115 pagesList of HCOsamit.panghaal89No ratings yet
- Color Atlas & Synopsis of Clinical Ophthalmology - Wills Eye Institute CorneaDocument384 pagesColor Atlas & Synopsis of Clinical Ophthalmology - Wills Eye Institute Corneam.No ratings yet
- ALS FA Poster Aed Untrained v3Document1 pageALS FA Poster Aed Untrained v3seeNo ratings yet
- DC2020-0067 ICD-10 Code For COVID-19 (Previously Known As 2019-nCoV) (02-12-20)Document1 pageDC2020-0067 ICD-10 Code For COVID-19 (Previously Known As 2019-nCoV) (02-12-20)Leah Rose Figueroa ParasNo ratings yet
- Auerbach's Wilderness Medicine PDFDocument1,672 pagesAuerbach's Wilderness Medicine PDFKieran D90% (10)
- Radiology CWRU Medical Student Elective Week 1Document112 pagesRadiology CWRU Medical Student Elective Week 1Yopi SimargiNo ratings yet
- Otto Warburg Metabolism of TumorsDocument12 pagesOtto Warburg Metabolism of Tumorsdanielbi2012No ratings yet
- Identification of Hemoglobin Varients Through HPLCDocument42 pagesIdentification of Hemoglobin Varients Through HPLCJohnNo ratings yet
- Hypodermoclysis: A Literature Review To Assist in Clinical PracticeDocument7 pagesHypodermoclysis: A Literature Review To Assist in Clinical PracticeRaabe AndradeNo ratings yet
- ResumeDocument4 pagesResumeAizack Gavrielle AbenganaNo ratings yet
- 610PHSPDF HSIBonusReportsDocument90 pages610PHSPDF HSIBonusReportsMichael ReyesNo ratings yet
- Chain of Survival: Adult and Pediatric Out of Hospital Cardiac ArrestDocument10 pagesChain of Survival: Adult and Pediatric Out of Hospital Cardiac ArrestJapeth John M. FloresNo ratings yet
- Forbidden Cures PDFDocument380 pagesForbidden Cures PDFJacek Jurkowski100% (2)