Professional Documents
Culture Documents
Pain and Inflammation: Management by Conventional and Herbal Therapy
Uploaded by
Nahiyah IsnandaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pain and Inflammation: Management by Conventional and Herbal Therapy
Uploaded by
Nahiyah IsnandaCopyright:
Available Formats
[Downloaded free from http://www.indianjpain.org on Thursday, June 25, 2015, IP: 202.67.41.
51]
Review Article
Pain and inflammation: Management by
conventional and herbal therapy
David Arome, Akpabio Inimfon Sunday, Edith Ijeoma Onalike, Agbafor Amarachi1
Department of Science Laboratory Technology (Physiology and Pharmacology Technology), University of Jos, Plateau State, 1Biochemistry,
Covanent University, Ota, Ogun State, Nigeria
ABSTRACT
The sensation of pain is an indication that something is wrong somewhere in the body. Pain and inflammation may be linked by
cyclooxygenase (COX) enzymes most especially COX2, which help in the synthesis of prostaglandins (PGs) precisely PGE2 and PGF2a,
found in high concentration at the inflammatory site. The released PGs either stimulate pain receptor or sensitized pain receptors to the
action of other pain producing substances such as histamine, 5-hydroxytryptamine (5HT), bradykinin which initiate and cause the nerve
cells to send electrical pain impulse to the brain. In the present review, an attempt is made to unveil the treatment approach adopted in the
management of pain and inflammation as well as animal models used in evaluating herbal plants with analgesic and anti-inflammatory
properties. The choice of the use of herbal medicine have been encouraged due to it availability, affordability, accessibility, and little or no
side effect associated with it. However, the question remains can herbal therapy serves as an alternative to available conventional drugs.
Different treatment options in the management of pain and inflammation have been highlighted.
Key words: Conventional drugs, herbal medicine, inflammation, pain
body to react, for instance by withdrawing the hand from
a very hot object.[3]
Introduction
The sensation of pain is an indication that something
is wrong somewhere in the body. Pain in its real sense
has no precise definition, but in general term, occurs
whenever the body tissue is damaged.[1] The damage may
be superficial or deep right in the tissue of the body. The
function of pain is to draw attention to injury and through
the reflexes elicited to protect the injured part. Whenever
pain sets in, the individual reacts to remove the pain.
Pain receptors and aerent pain fibers are distributed
all round the body. The pain sensation is initiated by
peripheral receptors by stimuli: Such as mechanical,
thermal, electrical, chemical, etc., at a threshold sucient
to cause tissue damage.[2] The pain stimulus is processed
in the brain which then sends impulses down the spinal
cord and through appropriate nerve which commands the
Inflammation is a natural response of the body to a variety
of hostile agents; invading microbes, physical injury,
and toxic substances which lead to the accumulation
of blood and plasmatic body f luids.[4] Inf lammation is
a normal protective mechanism adopted by the body
to get rid of offending stimuli, but if not properly
treated may result to a more damage with exuberance
to create chronic inf lammation,[5] and other diseases.[6]
Inf lammation is characterized by five cardinal clinical
signs, namely redness, swelling, pain, heat, and loss
of function.[7] Inf lammation can be acute and chronic.
Inf lammation is the most frequent triggered of pain.
Pain is basically triggered in an inf lamed tissue by
arachidonic acid metabolism as well as other painproducing substances released from the damaged
Access this article online
Quick Response Code:
Website:
www.indianjpain.org
DOI:
10.4103/0970-5333.128879
Indian Journal of Pain | January-April 2014 | Vol 28 | Issue 1
Address for correspondence:
Mr. David Arome,
Department of Science Laboratory Technology,
(Physiology and Pharmacology Tech),
University of Jos - 23473, Nigeria.
E-mail: davearome@gmail.com
5
[Downloaded free from http://www.indianjpain.org on Thursday, June 25, 2015, IP: 202.67.41.51]
Arome, et al.: Conventional and herbal therapy for pain and inflammation
tissue. [8] Inf lammation and pain may be linked by
cyclooxygenase (COX) enzymes most especially COX2
which help in the synthesis of prostaglandins (PGs)
precisely PGE2 and PGF2a, found in high concentration
at the inf lammatory site. [9] The released PGs either
stimulate pain receptor or sensitized pain receptors
to the action of other pain producing substances
such as histamine, 5-hydroxytryptamine (5HT), and
bradykinin which initiate and cause the nerve cells to
send electrical pain impulse to the brain.
Previous reports have implicated herbal medicine as
an alternative therapy to conventional drugs. Herbal
preparations are used for wide range of diseases such
as pain and inflammation with little or no side eect
associated with their use. The uses of conventional
drugs in the treatment of pain and inflammation have
largely been greeted with side eects. These presenting
challenges have triggered scientific researchers all over the
world in search of alternative therapy. The present work
seek to review the treatment approach adopted in the
management of pain and inflammation as well as animal
models used in evaluating herbal plants with analgesic and
anti-inflammatory properties.
Types of Pain
Fast Pain
This is a localized pricking type of pain felt less than
a second after application of pain stimulus: Electrical,
thermal, and stimuli. This type of pain is superficial and
is not felt in most deep part of the body tissue. Fast pain
is transmitted in the peripheral nerves to the spinal cord
through a nerve called A delta fibers (Ad fibers) at a speed
of 5-30 m/s. The high conductive velocity of pain stimulus
allows the body to withdraw immediately from the painful
and harmful stimuli in order to avoid further damage. For
example, touching hot plate and pin pricking.[2]
Slow Pain
Slow pain is a throbbing, diused, slow burning pain felt
few seconds after pain stimulus is applied and may last
for minutes, weeks, and even resulting to chronic pain
if not properly processed by the body. Slow pain starts
immediately after fast pain subsides. It is felt mostly in
deep tissue of the body. Slow pain is transmitted by C-fibers
(with diameter 0.2 and one thousand of a millimeter) to
the brain at a velocity of 0.5-2 m/s. The response of the
body is to hold the aected body part immobile so that
healing can take place. Other types of pain are: Referred
pain, viscera pain, etc.[2]
6
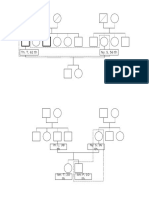
Differences between of fast pain and slow pain
Slow pain
Transmitted by very thin nerve
fibers
Poorly localized
All internal organs (except the
brain)
Body wants to be immobile to
allow healing (guarding, spam,
and rigidity)
Effective relief from opioid
Pain often radiates or is referred
For example, labor pain.
Fast pain
Transmitted by relatively thicker
faster conducting nerve fibers
Well localized
Mainly skin, mouth, and anus
Immediate withdrawal of
stimulation to avoid further
damage
Little relief from opioid
Pain does not radiate
For example, pain from a surgical
incision[10]
Pain transmission in the spinal cord and brain
Pain stimulus is transmitted through peripheral nerves to
the spinal cord and from there to the brain. This happens
via two dierent types of nerve fibers: Fast pain fibers and
slow pain fibers.
Fast pain is transmitted by A fibers to the spinal cord. Fast
pain fiber terminates at luminal one of the dorsal horns
of the spinal cord and excite the 2nd order neuron of the
neospinothalamic pathway which terminates at the reticular
area of the brainstem (ventrobasal complex). Fast pain
impulses are transmitted to specific and limited area of the
brain surface of cortex by neurotransmitter called glutamate
secreted by the fast pain nerve ending of the spinal cord
allowing for a relative precise localization of the pain.[3]
Slow Pain impulses are distributed diusely to dierent
parts of the brain. Each area of the brain elicit dierent
responds which explain the whole range of the symptoms
that pain can cause such as suering, sleeping diculties.[3]
Opioid analgesic system of the brain
The components of the opioid analgesic system of the
brain are:
1. The periaqueductal grey and periventricular area of the
mesencephalon in the upper pons
2. The raphe magnus nucleus located in the lower
pons and upper medulla and nucleus reticularis
paragigantocellaris.
3. Pain inhibitory complex located in the dorsal horn of
the spinal cord.
The nerve endings of the periaqueductal and periventricular
grey secrete mostly enkephalin, serotonin, when
stimulated. The endogenous mediator blocks signal at both
presynaptic and postsynaptic fibers of the Ad and C-fibers.
Met, leu enkephalin, dynorphin, and endorphin are the
major endogenous opioid substances found in the brain. The
Indian Journal of Pain | January-April 2014 | Vol 28 | Issue 1
[Downloaded free from http://www.indianjpain.org on Thursday, June 25, 2015, IP: 202.67.41.51]
Arome, et al.: Conventional and herbal therapy for pain and inflammation
arrival of pain impulses to the brain stimulate the release
of stored opioids causing them to bind to the receptors of
the terminal end of the ascending pain stimulating fibers
(APSF) to block the transmission and perception of pain.[2]
Inflammation
Previous reports have shown that inf lammation
manipulates two proteins namely: Calcium-activated
chloride channel and M-type potassium channel found
at the damage tissue of the pain sensing terminals of the
nerve cells. These proteins when targeted by bradykinin
cause the nerve cells to send electrical pain impulse to the
brain. The underlying mechanism to which this electrical
signal is generated still remains unclear.[10]
Walling o eect of inflammation
The very first eect of inflammation is to wall o the
injured area from other part of the tissue. This is made
possible by the fibrinogen clots which prevent fluid from
reaching the injured area. The important of walling o
process is to delay or slow down the spread of bacterial
and other toxic products.[2]
Types of inflammation
1. Acute inflammation: This is the initial response of the body
to harmful stimuli. The stimuli increased the movement
of plasma and white blood cells to the injured area.
2. Chronic inf lammation: This occurs as a result of
inflammation being prolonged for a period of time.
Some time it may result to autoimmune disease. Other
less common types are subacute inflammation and
granulomatous chronic inflammation.
Subacute inflammation has a chronic sign similar to acute
and chronic inflammation. It is an intermediate stage
between the two major types of inflammation.
Granulomatous chronic inflammation is a special type
of chronic inflammation associated with tuberculosis.[3]
Characteristics of Inflammation
Inflammation is characterized by
a. Vasodilation of the blood vessel and increase in blood
flow due to release of vasodilators.
b. Increase in permeability of capillaries leading to leakage
of fluid into the interstitial spaces.
c. Fluid clotting in the interstitial space due to the
leakage of excess fibrinogen and other proteins from
the capillaries.
d. Movement of large granulocyte monocyte to the injured
tissue.
e. Swelling of the tissue cells.[2]
Indian Journal of Pain | January-April 2014 | Vol 28 | Issue 1
Inflammatory reactions
Inflammatory reaction has two components
1. Innate response
The innate response is activated immediately after
infection or microbes invade the body. Innate responses
also prevent the adaptive response from targeting
and destroying the host cell. Innate response consists
of vascular and cellular element. Innate response is
mediated by antigen presenting cells (APC) which is
made up of dendritic cells and microphages. APC ingest
and process the antigen and present it on the surface of
the lymph nodes
2. Adaptive immune response
This is a complementary response that follows after
pathogen has been recognized by the innate system. It is
mediated by T and B lymphocyte.
Inflammatory reactions is controlled by the following
system: Cytokines complement, kinin, and fibrinolytic
pathways by lipid mediators (PG and leukotrienes)
released from a dierent cells and vasoactive mediator
release from mast cells, basophils, and platelet.[3]
Models of pain and inflammation
1. Animal models for pain
Models for Peripherally Acting Drugs
a. Acetic acid reduced abdominal writhing in mice
This is a widely used experimental model for screening
peripherally acting analgesic agents. Mice of either sex of
weight 20-25 g are used. The animals are pretreated with
the test sample. Thirty minutes after pretreatment, 0.2 ml
of 1% of the prepared acetic acid is injected into the animals
through intraperitoneal (IP) route, after which the mice
are transferred into a plastic bucket and observed. The
number of full abdominal writhes is counted for a total
duration of 5 min for each mouse.[11]
b. Pain in inflamed tissue (Randall-Selitto test)
The principle of this method is based on the fact
that inflammation increases the peripheral analgesic
sensitivity to pain. Animal with weight range of 130175 g fasted for 18-24 h is used. 0.1 ml of 20% suspension
of Brewers yeast is injected subcutaneously into the
left hind planter side of the paw. Three hours after
pretreatment with the test agent, pressure is applied
through tip of the plantar surface of the rat foot as
a constant rate using analgesiometer. Animal with a
control pain threshold greater than 80 g is eliminated
and replaced.[12]
7
[Downloaded free from http://www.indianjpain.org on Thursday, June 25, 2015, IP: 202.67.41.51]
Arome, et al.: Conventional and herbal therapy for pain and inflammation
Models for centrally acting drugs
a. Tail immersion test
Animals used for the test are placed in an individual
cage or restrainer, allowing for 30 min of acclimatization
leaving the tail hanging out freely. Five centimeter from
its tips of the animal tail is marked. The marked part is
immersed in cup of freshly filled water of temperature of
55C. Stopwatch is used in recording the reaction time,
both before and after administration of the test compound.
Withdrawal time more of than 6 s is regarded as a positive
response.[13]
b. Hot plate test
Hot plate test is used to assay narcotic drugs or agents. In
this method, hot plate surface is maintained at a constant
temperature of 55-56C. Animals are placed in a glass
bucket of 55 cm diameter or heated surface, and the
time between placement and shaking or leaking of the
paw or jumping is recorded as index of response latency.
Animals receive the test compound orally 1 h before they
are placed on the hot plates. Centrally acting analgesic
drug prolonged the response time.[14]
Other models for centrally analgesic drugs are:
1. Pleurisy test
2. Ultraviolent erythema test in guinea pigs
3. Oxazolone-induced ear edema in mice
4. Granuloma pouch techniques
Animal models for inflammation
Experimental models for acute and subacute inflammation
study
a. Carrageenan-induced paw edema in rat
This model is used to assay acute anti-inflammatory activity
of a test agent. One hour after pretreatment of animals with
test sample, 0.1 ml of 1% prepared carrageenan is injected
subcutaneously into plantar side of the left hind paw of
the animal. Paw volume is measured at 30 min interval
after the injection of 0.1 ml prepared carrageenan for
the total duration of 2-3 h, paw volume of the animal is
measured at 0 min with digital plethysmometer before the
administration of the test sample. The dierence between
the initial and subsequent paw volume values gives the
actual paw edema and which compared with the control.
Paw volume can also be measured with vernier caliper, pair
of divider, and cotton thread.[15]
b. Egg albumin induce paw edema in rat
Egg albumin is used to screen agent with acute antiinflammatory eects, especially if inflammation is not
intended to be sustained for long. The procedure used
is the same as that of the carrageenan, but with slight
8
modification in some cases. Here paw volume is measured
as 20 min interval after the injection of 0.1 ml of the egg
albumin for the total duration of 2 h. Paw volume is
measured at 0 min before the administration of the test
compound.[16]
Treatment of Pain and Inflammation
1.
2.
3.
4.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Narcotic drugs
Corticosteroids drugs
Immune selective anti-inf lammatory derivatives
(mSAIDs)
5. Herbal therapy
NSAIDs
NSAIDs are used for the treatment of mild to moderate
type of pain and inflammation. For example, ibuprofen,
indomethacin, and diclofenac. NSAIDs act through
inhibition of enzyme COX, most precisely COX 2
responsible for the biosynthesis of PGs which triggered
inflammation thereby preventing the amplification of the
pain stimuli.[17,18]
Side effects: Nausea, indigestion, bleeding from the
stomach, peptic ulcer, and bronchopasm.[19]
Narcotics Drugs
Basically used in the treatment of severe type of pain. These
are classified into three groups:
i. Natural opium alkaloid divided into
a. Phenanthrene group: For example, morphine
b. Benzylisoquinoline group: For example, papaverine
ii. Semisynthetic opioid: For example, oxycodone
iii. Synthetic derivatives with structures unrelated to
morphine
Mechanism of action
The pharmacological action of narcotic is mediated
by specific and multiple receptors. mainly: d, m,
and k receptors. Stimulation cause the release of the
endogenous opioids like enkaphalin, dynorphin from
the terminal ending of the descending pain inhibitory
fibers making to attached to receptors of the terminal of
the ascending pain carry fibers, and prevent the release
of substance P. All opioid analgesic receptors bind to
selective endogenous opioid receptors to elicit their
pharmacological action.[3]
Side effect of narcotics analgesic drugs: Euphoria,
tolerance, nausea, vomiting, and sedation.
Indian Journal of Pain | January-April 2014 | Vol 28 | Issue 1
[Downloaded free from http://www.indianjpain.org on Thursday, June 25, 2015, IP: 202.67.41.51]
Arome, et al.: Conventional and herbal therapy for pain and inflammation
Table 1: Herbal plants with analgesic and anti-inflammatory property
Plant (family)
Ficus ingens
(Moraceae)
Part used
Leaves
Zea may Husk
(Poacea)
Carica papaya
Seeds
Typhonium
Leaves
trilobatum
(Araceae)
Dracaena cinnabari Resin
Balf
Kaempferia galanga Rhizomes
Stachys
lavandulifolia
Aerial
parts
Jatropha curcas
Leaves
Tabernaemontana
divaricata
(Apocynaceae)
Flower
Tectona grandis
(Verbenaceae)
Guiera
senegalensis Gmel
(Combretaceae)
Leaves
Leaves
Litsea sebifera
(Lauraceae)
Different
part
Markhamia
tomentosa
(Bignoniaceae)
Leaves
Rosa damascene
(Rosaceae)
Chemical constituents
Alkaloids, glycosides, saponins,
flavonoids, carbohydrates,
tannins
Tannins, steroids, polyphenols
Uses
Fever, pain, inflammation,
pile, diarrhea, diuretics
Alkaloids, resins,
carbohydrates, fats, glycosides
Reducing sugar, alkaloids,
flavonoids, steroids tannins,
flavonoids gums, glycosides
Flavonoids, trepenoids, sterol
Antibacterial, malaria,
inflammation, deworming
Piles, rheumatism, asthma,
head ache, gastric ulcer
Pain, arthritis
Gastric sores, diarrhea,
dysentery, analgesic, skin
and mucosal diseases
Volatile oils: Eucalyptol,
Abdominal pain,
carvone
embrocation applied
on muscular swelling,
rheumatism
Flavonoids, saponins, and bitter Pain, inflammatory disorders
compounds
Animal models
References
Hot plate test, acetic acid-induced [11,14,23]
writhing test, carrageenaninduced paw edema
[24-28]
Hot plate test, formalin-induced
paw licking test, carrageenaninduced paw edema
[29-31]
Fresh egg albumin
Acetic acid-induced writhing,
xylene-induced ear edema
Acetic acid test, tail flick,
carrageenan-induced paw edema,
trauma-induced paw edema
Hot plate test, radiant heat tail
flick, carrageenan-induced paw
edema, cotton pellet-induced
granuloma model
Acetic acid-induced writhing,
formalin test, light tail flick,
carrageenan-induced paw edema
Alkaloids, saponins, trepenoids, Jaundice, pain, skin diseases, Acetic acid writhing test, egg
tannins, and steroids
cancer, snake bites
albumin-induced edema
Alkaloids, glycosides, steroids, Rejuvenation therapy, pain
Acetic acid-induced writhing, hot
saponins, flavonoids, terpenes, and inflammation, improved plate reaction test, carrageenanglycosides, proteins, amino
memory
induced paw edema
acids, fixed oil, tannins, and
volatile oil
Flavonoids, phenolic acids,
Analgesic, inflammation,
Eddys hot plate, carrageenanquinines, terpenes
wound healing
induced paw edema model
Alkaloids, glycosides, tannins, Diarrhea, rheumatism,
Acetic acid-induced writhing test,
and flavonoids
syphilis, leprosy, impotence, egg albumin induced edema,
dieresis, expurgation, fever,
malaria
Alkaloids, flavonoids,
Antiseptic, expectorant,
Acetic acid-induced writhing
glycosides, and saponins
tonics, fever, pain,
in mice, formalin induced hind
inflammation
paw licking test, carrageenaninduced paw edema, egg albumin
inflammation
Tannins, alkaloids, cardiac
Rheumatoid arthritis,
Writhing test, hot plate test,
glycosides, flavonoids, phenol, edema, gout, headache,
formalin test, immersion test,
an saponins
snake venom, scrotal
carrageenan
elephantiasis
Flavonoids, glycosides, tannins, Inflammatory diseases,
Writhing test, formalin test, tail
quercetin, caempterol, terpene, cough remedy, digestive
flick test, formalin-induced paw
myrcene, vitamin C, carboxylic, problems, laxative,
licking test, carrageenan-induced
essential oil: Geraniol,
antibacterial activity
paw edema
docosane, beta-citronellol, and
nonadacene
Corticosteroid Drugs
These are anti-inf lammatory agents that prevent
phospholipid release and undermines eosinophil action and
number of other mechanism involved in inflammation.[10]
Sets of corticosteroids drugs
a. Glucocorticoids are normally prescribed in the
treatment of inflammatory bowel diseases, hepatitis,
and allergic reactions.
Indian Journal of Pain | January-April 2014 | Vol 28 | Issue 1
[32-35]
[15,36-43]
[1,6,44-47]
[11,14,15,48]
[49,50]
[15,51,52]
[53-60]
[61-63]
[64-67]
[14,15,68-71]
[14,15,72-76]
b. Mineralocorticoid: Used with other medications in the
treatment of cerebral salt wasting.
mSAIDs
This new class of anti-inflammatory agent is found to alter
the activation and migration of immune cells involved
in amplification of inf lammatory response. mSAIDs
have been implicated as potential veterinary drugs for
controlling and reducing inflammation.[10]
9
[Downloaded free from http://www.indianjpain.org on Thursday, June 25, 2015, IP: 202.67.41.51]
Arome, et al.: Conventional and herbal therapy for pain and inflammation
Herbal Therapy
Herbal medicine is the oldest form of healthcare known
to mankind. Herbs have been used virtually by all culture
throughout history. People around the world in dierent
civilization have used plants to treat dierent diseases for
several years.[20] Herbal medicine is an alternate treatment
of disease which constitutes the use of dierent plants and
their extracts. Herbal medicine comes in dierent forms
that include extract, tablet, essential oil, or ointment.
Herbs are used to treat various disease conditions such
as asthma, eczema, premenstrual syndrome, etc., and
some cases may have fewer side eects than conventional
drugs.[21] About 28% of all modern drugs in use today are
derived directly from naturally occurring substances in
plants.[22] Substances derived from plants remain the basis
for large proportion of commercial medication Table 1.
5.
6.
7.
8.
9.
10.
11.
Conclusion
12.
Inflammation is a normal defensive mechanism adopted
by the body to get rid of invading microbes. However,
if left untreated may result to other chronic diseases.
Hence, there is need to arrest it before it gets out of
control. Dierent treatment options are available in the
treatment of pain and inflammation. Conventional and
herbal therapies are the widely used options employed.
The use of the former is greeted with numerous unwanted
side eects, which limit their application. The choice of
the use of herbal medicine have been encouraged due to it
availability, aordability, accessibility, and little or no side
eect associated with it.
13.
14.
15.
16.
17.
18.
The use of herbal medicine can serve as treatment options
or alternative therapy in the treatment of pain and
inflammation.
19.
Acknowledgment
20.
The authors would sincerely like to appreciate Mr Imadi David for
his encouragement and support toward the success of this paper.
21.
References
22.
1.
23.
2.
3.
4.
10
Michel YB, Dubois, Christopher G, Allen HL. Chronic pain
management. In: Healy TEJ, Knight PR, editors. Wylie and
Churchil-Davidsons A practice of Anaesthesia, 7th ed. London:
Hodder Arnold; 2003. p. 1235-9.
Guyton C, Hall JE. Medical Physiology, 11th ed. Churchill
Livingstone 2006;598-609.
Rang HP, Dale MM, Ritter JM, Flower RJ. Rang and Dales
Pharmacology, 7th ed, Churchill Livingstone; 2006;202-210.
Sobotar R, Szwed M, Kasza A, Bugno M, Kordula T.
Parthenolide inhibits activation of signa transducers and
24.
25.
activators of transcription (STATS) induced by cytokines of the
IL-6 family. Biochem Biophys Res Commun 2000;267:329-33.
Coulter A. The significance of pain and inflammation. Wholistic
Health Care. Capital Technologies 2013.
Sosa S, Balicet MJ, Arvigo R, Esposito RG, Pizza C, Altinier
G, et al. Screening of the topical antiinflammatory activity of
some central American plants. J Ethanopharmacol 2002;8:211-5.
Winyard PG. Key stages of acute anti-inflammatory response
and their relevance in therapeutic target. In: Winloughby
DA, Winyard PG, editors. Methods in molecular biology;
inflammation protocols. Human press inc 2003;225:3.
Shrma HL, Sharma KK, Dasal C. Principle of Pharmacology.
Medical Publishers, New Delhi, India 2007.
Derardt R, Jongney S, Delvalcee F, Falhout M. Release of
prostagladdins E and F in an algogenic reaction and its inhibition.
Eur J Pharmacol 1980;51:17-24.
Nordqvist C. Medical news today. Mediexicon international Ltd,
United Kingdom 2012.
Koster R, Anderson M, Debeer EJ. Acetic acid method of
analgesic screening. Curr Opin Immunol 1959;18:412.
Agrawal SS, Paridhavi M. Herbal drug technology. Universities
Press, India 2007:557-60.
Asongalem EA, Foyet HS, Ekobo S, Dimo T, Kamtchouing P.
Antiinflammatory lack of the central analgesia and antipyretic
properties of Acanthus montanus. J Ethnopharmacol 2004;95:63-8.
Turner RA. Analgesics: Screening Methods in Pharmacology.
New York: Academic Press; 1965. 100.
Winter CA, Risley EA, Nuss GV. Carrageenin induced oedema
in hindpaw of rats as an assay for anti-inflammatory drugs. Proc
Soc Exp Biol Med 1962;111:544-7.
Akah PA, Nwambie AI. Evaluation of Nigeria traditional
medicine: 1. Plants used for rheumatic (inflammation) disorders.
J Ethnopharmacol 2010;42:179-82.
Albert D, Zundorf I, Dingerman T, Muller WE, Stanhiber D,
Werz O. Hyperforin is a dual inhibitor of cyclooxygenase-1 and
5-lipoxygenase. Biochem Pharmacol 2002;64:1767-75.
Herdman JG, Limbird LE., eds. Goodman and Gulmans The
Pharmacological Basis of Therapeutics. ,New York: McGrawHill; 2001. 687-92.
Tapiero H, Ba GN, Couvreur P, Tew KD. Poyunsaturated fatty
acids (PUFA) and eicosanoids in human health pathologies.
Biomed Pharmacother 2002;56:215-22.
Calixto JB, Beirith A, Ferriera J, Satitos AR, Fiho VC, Yunes
RA. Naturally occurring antinociceptive substances from plants.
Phytother Res 2000;14:407-18.
Chin YW, Balunas MJ, Chai HB, Kiryhom AD. Drug discovery
from natural sources. AAPS J 2006;8:239-53.
Izzo AA, Einst E. Interaction between herbal medicine prescribed
drugs. An updated systematic review. Drug 2009;69:1777-98.
Niemeeger CJ, Verbiuggen FJ, Janssen PA. Effect of various
drugs on carrageenan induced oedema in rat hind paw. J Pharm
Pharmacol 1964;16:810-6.
Santos AR, Filho VC, Yunes RA, Calixto JB. Further studies
on the antinociceptive action of the hydroalcoholic extracts
from plants of the genus Phyllanthus. J Pharm Pharmacol
1995;47:66-71.
Hunskaar S, Hole K. The formalin test in mice dissociation
between inflammatory and non inflammatory pain. Pain
1987;30:103-14.
Indian Journal of Pain | January-April 2014 | Vol 28 | Issue 1
[Downloaded free from http://www.indianjpain.org on Thursday, June 25, 2015, IP: 202.67.41.51]
Arome, et al.: Conventional and herbal therapy for pain and inflammation
26. Olajide OA, Awe SO, Makinde JM, Ekhelar AI, Olusola A,
Morebise O, et al. Studies on the anti-inflammatory, antipyretic
and analgesic properties of Alstonia boonei stem bark. J
Ethnopharmacol 2000;71:179-86.
27. Owoyele VB, Wuraola CO, Soladoye AO, Olaleye SB. Studies
on the anti-inflammatory and analgesic properties of Tithonia
diversifolia leaf extract. J Ethnopharmacol 2004;90:317-21.
28. Mossa JS, Rafatullah S, Galal AM, Al-Yahya MA.
Pharmacological studies of Rhus retinorrhara L. Int J
Pharmacogn 1995;33:242-6.
29. Payne DN. Nitric oxide in allergic air way inflammation. Curr
Opin Allergy Clin Immunol 2003;3:133-7.
30. Marrow JD, Roberts LJ. 1.1 (2001): Lipid-derived autacoids,
eicosanoids and platelet-activating factor. Goodman & Gilmans:
The parmacological basis of therapeutics. New York: McGrawHill, Medical Publishing Division USA 2006;9-680.
31. Akah PA, Akunyili DN, Egwuatu CN. Investigations on the
analgesic and antipyrectic activities of aqueous extract of
Caricapapaya leaves. Nig J Neurosci 2002;5:29-34.
32. Das HB, Mojumder K, Datta BK, Ray D. Ethnobotanical uses
of some plants by Tripuri and Reang tribes of Tripura. Nat Prod
Rad 2009;8:172-80.
33. Rahmatullah M, Rahman L, Rehana F, Kalpana MA, Khatun
MA, Jahan R, et al. A scientific evaluation of medicinal plants
used in the folk medicinal system of five villages in Narsinghdi
District, Bangladesh. Am Eurasian J Sustain Agric 2010;4:5.
34. Ahmed F, Selim MS, Das AK, Choudhuri MS. Anti-inflammatory
and anti-nociceptive activities of Lippia nodiaflora Linn.
Pharmazie 2004;59:329-30.
35. Yaro AH, Magaji MG, Danjuma NM, Malami S, Isah A. Studies
on analgesic and anti-inflammatory activities of Cissampelos
mucronata Linn in laboratory animals. Int J Pure App Sci
2008;2:111-7.
36. Miller AG, Morris M, plants of Dhofar-the southern region of
Oman, traditional, economic and medicinal uses. Office of the
adviser on the Environment, Diwan of Royal Court, Sultanat
of Oman 1988.
37. Dongmo AB, Nguelefack T, Lacaille- Dubois MA. Anti
nociceptive and anti-inflammatory activities of acacia pennata
wild (Mimmo Saceae). J Ethnopharmacol 2005;98:201-6.
38. Nguemfo EL, Dimo T, Azebaze AG, Asongalem EA, Alaoui K,
Dongmo AB, et al. Anti inflammatory and anti nociceptive
activities of the stem barkextracts from Allanblackia monticola.
J Ethnopharmacol 2007;114:417-24.
39. Dykstra LA, Woods JH. A tail withdrawal procedure for
assessing analgesic activity in rhesus monkeys. J Pharmacol
Methods 1986;15:263-9.
40. Toma W, Graciosa JS, Hiruma-Lima CA, Andrade FD,
Vilegas W, Souza Brito AR. Evaluation of the analgesic and
antiedematogenic activities of Quassia amara bark extract. J
Ethnopharmacol 2003;85:19-23.
41. Riesterer L, Jacques R. The influence of anti-inflammatory drugs
on the development of an experimental traumatic paw oedema
in the rat. Pharmacology 1970;3:243-51.
42. Feirreira SH, Moncada S, Vane JR. Indomethacin and aspirin
abolish prostaglandin release from the spleen. Nature New Biol
1971;231:237-239.
43. Al-sobarry M, Alwashli A, Cherrah Y, Alaoui K. Antiinflammatory activities of methanolic extract of Jatropha
unicostata balf (Sibru) and ethanolic extract of Aloe perryi
Indian Journal of Pain | January-April 2014 | Vol 28 | Issue 1
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
baker (taife), as endemic plants in Yemen. Int J Nat Prod Pharm
Sci 2011;2:40-55.
Eddy NB, Liembach D. Synthetic analgesics II. Dithienylbuttenyl
and dithiennylbulyl-amines. J Pharmacol Exp Ther 1957;107:385-93.
Prempeh AB, Mensah Attipoe J. Analgesic activity of crude
aqueous extract of the root bark of zanthoxylum xanthoxyloides.
Ghana Med J 2008;42:79-84.
DAmour FE, Smith DL. A method for determining loss of pain
sensation. J Pharmacol Exp Ther 1941;72:74-9.
Othman R, Ibrahim H, Mohd MA, Mustafa MR, Awang K.
Bioassay-guided isolation of a vasorelaxant active compound
from Kaempferia galanga L. Phytomedicine 2006;13:61-6.
Hajhashemi V, Ghannadi A, Sedighifer S. Analgesic and antiinflammatory properties of hydroalcoholic polyphenolic and boiled
extracts of Stachys lavandulifolia. Res Pharm Sci 2007;2:92-8.
Okujagu TF, Etatuvie SO, Eze I, Jimoh B, Nweke C, Mbaoji
C. Medicinal Plants of Nigeria; South-west Nigeria. In:
Collaboration with Lagos state Traditional Medicine Board
and Botany Department, University of Lagos. 1st ed, 2006;1:20.
Arul V, Miyazaki S, Dhananjayan R. Studies on the antiinflammatory, antipyretic and analgesic properties of the leaves
of Aegle marmelos Corr. J Ethnopharmacol 2005;96:159-63.
Ingkaninan K, Temkitthawon P, Chuenchom K, Yuyaem T,
Thongnoi W. Screening for acetylcholinesterase inhibitory
activity in plants used in Thai traditional rejuvenating and
neurotonic remedies. J Ethnopharmacol 2003;89:261-4.
Taesotikul T, Panthong A, Kanjanapothi D, Verpoorte R, Scheffer
JJ. Neuropharmacological activities of the crude alkaloidal
fraction from stems of Tabernaemontana pandacaqui Poir. J
Ethnopharmacol 1998;62:229-34.
Nayeem N, Karverkar MD. Wound healing ; A review. Res J
Pharma Bio Chem Sci 2010;8:221.
Aguinaldo AM, Ocampo OM, Bowden BF, Gray AI, Waterman
PG. Phytochemistry. In: Guevara BQ (ed). A guide book to plant
screening and biological. University of Santo Tomas, Manila
Phillipines 1993;33:933.
Macas FA, Lacret R, Venela RM, Nogueiras C, Molinillo JM.
Isolation and phytotoxicity of terpenes from Tectona grandis.
J. Chem. Ecol 2010;36:396-404.
Nayeem N, Karvekar MD. Analgesic and anti-inflammatory
activity of methanolic extract of the frontal leaves of Tectona
grandis. Inter J Pharma Bio Sci 2010813:1.
Jain PK, Soni P, Upmanyu N, Shivhare Y. Evaluation of analgesic
activity of Manilkara zapora leaves.Eur J Exp Bio 2011;1:14-17.
Lakheda S, Devalia R, Jain UK, Gupta N, Raghuwansi
AS, Patidar N. Anti inflammatory activity of Artocarpus
heterophyllus bark Der Pharmacia Sinica 2011;2:127-30.
Khadse CD, Kakde RB. Inflammatory activity of aqueous
extract fractions of Barieria prionitis L. roots. Asian Plant Sci
Res 2011;1:63-8.
Mathur A, Purohit R, Deepika M, Prasad KS, Dua VK. Der.
Pharmacological investigation of methanolic extract of Mentha
piperita L. root on the basis of antimicrobial, anti-oxidant and
anti-inflammatory. Der Pharmacia Sinica 2011;2:208-21.
Abbiw DK. Useful Plants of Ghana. Vol. 1, Kew, In: Stermediate
Technology Publication ltd and Royal Botanic Gardens. 1990. 28-34.
Hutchinson J, Dalziel JM. Flora of West Tropical Part 1, Crown
agents for oversea governments and administrations, London
1965;1:275.
11
[Downloaded free from http://www.indianjpain.org on Thursday, June 25, 2015, IP: 202.67.41.51]
Arome, et al.: Conventional and herbal therapy for pain and inflammation
63. Zeljan M, Marica M, Franz B. Flavonoida of G. Senegalensis
thin layer chromatography and numerical methods. Croatica
Chemica Acta 1998;71:69-79.
64. Okokon JE, Anita BS, Emem U. Analgesic and anti-inflammatory
effects of etha nolic extractsof Hippcratea Africana. Int J
Pharmacol 2008;4:51-5.
65. Kumar V, Abbas AK, Fauso N. Robbins and cotran pathologic
basis of disease, 7th ed. Philadelphia: Elsevier Saunders; 2004.
47-86.
66. Saddi G, Abbott FV. The formalin test in the mouse: A parametric
analysis of scoring properties. Pain 2000;89:53-63.
67. Hunskaar S, Fasmer OB, Hole K. Formalin test in mice: A useful
technique for evalu-atingmild analgesics. J Neurosci Methods
1987;4:69-76.
68. Buttgereit F, Burmester GR, Simon LS. Gastrointestinal toxic
side effect of nonsteroidal ant-inflammatory drugs and cyclooxygenase-2- specific inhibitor. Am J Med 2001;110:13-9.
69. Aladesanmi AJ, Iwalewa EO, Adebajo AC, Akinkunmi EO,
Taiwo BJ, Olorunmola FO, et al. Antimicrobial and antioxidant
activities of some Nigerian medicinal plants. Afr J Tradit
Complement Altern Med 2006;4:173-84.
70. Nguemfo EL, Dimo T, Azebaze AG, Asongalem EA, Alaui
K, Dongmo AB, et al. Anti-inflammatory and antinociceptive
activities of stem bark extracts from Aanblackia monticola. J
Ethnopharmacol 2007;114:417-24.
12
71. Nkeh-Chungag BN, Temdore JR, Sewani-Rusike C, Fodjo
VM, Mbafor JT. Analgesic, anti-inflammatory antiulcer
properties of the extract of Vapaca guineensis. J Med Plants
Res 2009;3:635-40.
72. Lister M. Delmars Intergrative Herbal Guide for Nurse.
Thompson Learning Alby, Delmar 2002;360-70.
73. Basim E, Basim H. Antibacterial activity of Rosa demascena
essential oil. Fitoterapia 2003;74:394-6.
74. Yassa N, Masoomi F, Ronkouhi SE, Hadjlahoondi A. Chemical
composition and anti-oxidant activity of the extract and essential
oil of Rosa damascene from Iran, population of Gallani. Daru
2009;17:175-80.
75. Ferreira J, Floriani AE, Filho VC, Delle-Monache F, Yunes RA,
Calixto JB, et al. Antinoceptive properties of the methanolic
extract of two triterpenes isolated from Epidendrum mosenji
stem. Life Sci 2000;60:791-802.
76. de Miranda FG, Vilar JC, Alves IA, Cavalcanti SC, Antoniolli
AR. Atinociceptive and antiedematogenic properties and acute
toxicity of Tabebula avellendae lor, inner back aqueous extract.
BMG Pharmacol 2001;1:6.
How to cite this article: Arome D, Sunday AI, Onalike EI, Amarachi
A. Pain and inflammation: Management by conventional and herbal
therapy. Indian J Pain 2014;28:5-12.
Source of Support: Nil. Conflict of Interest: None declared.
Indian Journal of Pain | January-April 2014 | Vol 28 | Issue 1
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Regional Anesthesia in Cattle PDFDocument33 pagesRegional Anesthesia in Cattle PDFNiaz AsgharNo ratings yet
- Roh 4Document52 pagesRoh 4gajucoolkarni50% (6)
- TSU Nursing Performance Evaluation ChecklistDocument7 pagesTSU Nursing Performance Evaluation ChecklistKatKat Bognot100% (2)
- AMORCDocument14 pagesAMORCJupiter16100% (6)
- DalaDocument1 pageDalaNahiyah IsnandaNo ratings yet
- DalaDocument1 pageDalaNahiyah IsnandaNo ratings yet
- Garbage 7Document1 pageGarbage 7Nahiyah IsnandaNo ratings yet
- MaftukhahDocument4 pagesMaftukhahNahiyah IsnandaNo ratings yet
- BeautifulDocument2 pagesBeautifulNahiyah IsnandaNo ratings yet
- GarbageDocument1 pageGarbageNahiyah IsnandaNo ratings yet
- Love Scenario IKONDocument2 pagesLove Scenario IKONTyakaNo ratings yet
- Solo 2Document1 pageSolo 2Nahiyah IsnandaNo ratings yet
- Black PinkDocument2 pagesBlack PinkNahiyah IsnandaNo ratings yet
- Garbage 6Document1 pageGarbage 6Nahiyah IsnandaNo ratings yet
- Shared by On Aug 29, 2013 in - See More At: Source:: Cancercouncilnsw Health Tobacco#Sthash.4Xoc8Qkp - DpufDocument1 pageShared by On Aug 29, 2013 in - See More At: Source:: Cancercouncilnsw Health Tobacco#Sthash.4Xoc8Qkp - DpufNahiyah IsnandaNo ratings yet
- Breast Cancer GuidelineDocument127 pagesBreast Cancer GuidelinetambahanNo ratings yet
- Intra OcularTumoursDocument35 pagesIntra OcularTumoursdrvishalkulkarni2007100% (1)
- Geno GenoDocument2 pagesGeno GenoNahiyah IsnandaNo ratings yet
- IndianJPain2815-3667104 101111Document8 pagesIndianJPain2815-3667104 101111Nahiyah IsnandaNo ratings yet
- IndianJPain28261-3648707 100807Document10 pagesIndianJPain28261-3648707 100807Nahiyah IsnandaNo ratings yet
- IndianJPain273114-3926598 105425Document7 pagesIndianJPain273114-3926598 105425Nahiyah IsnandaNo ratings yet
- PDFDocument36 pagesPDFnetifarhatiiNo ratings yet
- IndianJPain283184-3773691 102856Document5 pagesIndianJPain283184-3773691 102856Nahiyah IsnandaNo ratings yet
- MONREP Surgery PatientsDocument16 pagesMONREP Surgery PatientsNahiyah IsnandaNo ratings yet
- Lyrics: Dream High (Taecyeon, Suzy, Joo & Kim Soo Hyun)Document3 pagesLyrics: Dream High (Taecyeon, Suzy, Joo & Kim Soo Hyun)ridz_1205No ratings yet
- Comparing Pethidine and Ondansetron for Preventing ShiveringDocument12 pagesComparing Pethidine and Ondansetron for Preventing ShiveringKikiNurAqidahNo ratings yet
- Nanda ScabiesDocument1 pageNanda ScabiesNahiyah IsnandaNo ratings yet
- Breast FeedingDocument6 pagesBreast FeedingNahiyah IsnandaNo ratings yet
- Statistik Karakteristik RespondenDocument14 pagesStatistik Karakteristik RespondenNahiyah IsnandaNo ratings yet
- Lap PBL 1-BHL VIDocument13 pagesLap PBL 1-BHL VINahiyah IsnandaNo ratings yet
- MPS Therapy Flyer April 10 2018Document8 pagesMPS Therapy Flyer April 10 2018Neptune ShellNo ratings yet
- Lecture 2A The Chief Complaint Its HistoryDocument20 pagesLecture 2A The Chief Complaint Its HistoryAhmed HegazyNo ratings yet
- Enactive Approach To PainDocument29 pagesEnactive Approach To PainAlejandroNo ratings yet
- POS Questionnaire v1 Patient EN-22-08-2011Document2 pagesPOS Questionnaire v1 Patient EN-22-08-2011StefiSundaranNo ratings yet
- Music Therapy in Acute and Chronic Pain Management: A Literature ReviewDocument2 pagesMusic Therapy in Acute and Chronic Pain Management: A Literature ReviewSean EurekaNo ratings yet
- The Kadoka Press, May 3, 2012Document10 pagesThe Kadoka Press, May 3, 2012surfnewmediaNo ratings yet
- Clinical Rehabilitation: Goal Attainment Scaling (GAS) in Rehabilitation: A Practical GuideDocument12 pagesClinical Rehabilitation: Goal Attainment Scaling (GAS) in Rehabilitation: A Practical GuideMarla Constanza Martinez RoseroNo ratings yet
- ... My Reflection On Action (Leadershinp and Management)Document15 pages... My Reflection On Action (Leadershinp and Management)Yasmeen zulfiqarNo ratings yet
- Corporal PunishmentDocument4 pagesCorporal Punishmentabdulhadi masoodNo ratings yet
- Morbid Anxiety As A Risk Factor in Patients With Somatic Diseases A Review of Recent FindingsDocument9 pagesMorbid Anxiety As A Risk Factor in Patients With Somatic Diseases A Review of Recent FindingsAdelina AndritoiNo ratings yet
- Healy Professional DeviceDocument1 pageHealy Professional DeviceBramarish KadakuntlaNo ratings yet
- VHA Pain DirectiveDocument12 pagesVHA Pain DirectiveJimNo ratings yet
- Prioritization and delegation rules for nursesDocument20 pagesPrioritization and delegation rules for nursesPascal St Peter Nwaorgu100% (1)
- 600 Confusing English Words ExplainedDocument209 pages600 Confusing English Words Explainedata nazariNo ratings yet
- Shawa - Patients Perceptions Regarding Nursing Care in The General Surgical Wards at Kenyatta National Hospital - NinisannnDocument103 pagesShawa - Patients Perceptions Regarding Nursing Care in The General Surgical Wards at Kenyatta National Hospital - Ninisannnnoronisa talusobNo ratings yet
- Focus On Diagnosis of Acute Compartment Syndrome PDFDocument8 pagesFocus On Diagnosis of Acute Compartment Syndrome PDFMuthia DewiNo ratings yet
- Translate Morgan SecsioDocument4 pagesTranslate Morgan SecsioYolanda KasiNo ratings yet
- About Jure and The AEQ MethodDocument3 pagesAbout Jure and The AEQ MethodJure KoščakNo ratings yet
- Dutton Chapter 11 Manual TherapiesDocument24 pagesDutton Chapter 11 Manual Therapiesmaria_dani100% (1)
- Contract CodexDocument18 pagesContract CodexGnomeMadeIon100% (4)
- Exploratory Study On Bach Flower RemediesDocument39 pagesExploratory Study On Bach Flower RemediesNarayananSrinivasan100% (1)
- Assessment of Hypnosis Knowledge Among Dentists: A Cross Sectional StudDocument9 pagesAssessment of Hypnosis Knowledge Among Dentists: A Cross Sectional StudSri Mulyani DjunaidiNo ratings yet
- Case History FibromyalgiaDocument23 pagesCase History FibromyalgiaRAGUPATHYNo ratings yet
- Penn Shoulder Score 3Document2 pagesPenn Shoulder Score 3Izemari SwartNo ratings yet
- Epidural Steroid InjectionDocument3 pagesEpidural Steroid Injectionhi_landsNo ratings yet
- Homeo 2Document10 pagesHomeo 2RENJULALNo ratings yet