Professional Documents
Culture Documents
HIV in Pregnancy
HIV in Pregnancy
Uploaded by
Tio Prima SCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
HIV in Pregnancy
HIV in Pregnancy
Uploaded by
Tio Prima SCopyright:
Available Formats
6/8/2015
HIVinPregnancy
HIVinPregnancy
Author:TeresaMarino,MDChiefEditor:ThomasChihChengPeng,MDmore...
Updated:Jan15,2015
Overview
Thereductioninmothertochildtransmissionofhumanimmunodeficiencyvirus(HIV)isregardedasoneofthe
mosteffectivepublichealthinitiativesintheUnitedStates.Intheabsenceoftreatment,theriskofvertical
transmissionofHIVisashighas2530%.WiththeimplementationofHIVtesting,counseling,antiretroviral
medication,deliverybycesareansectionpriortoonsetoflabor,anddiscouragingbreastfeeding,themotherto
infanttransmissionhasdecreasedtolessthan2%intheUnitedStates.
Beforethecurrenttreatmentera,approximately2000babieswereinfectedwithHIVeachyearintheUnitedStates
alone.DespiteincreasingHIVprevalence,thatfigurenowstandsatapproximately300infantsperyear. [1]
Therapidclinicalimplementationofresearchfindingsdirectedtowarddecreasingperinataltransmissioniscredited
asthekeytothisaccomplishment.In1994,thePediatricAIDSClinicalTrialsGroup(PACTG)protocol076
demonstratedthattheadministrationofzidovudineduringpregnancyandlaborandthentothenewborndecreased
theriskofperinataltransmissionofHIVby68%,from25.5%to8.3%. [2]Inthelate1990s,thecombineduseof3or
moreantiretroviralmedicationswasfoundtobehighlysuccessfulatsuppressingviralreplication.
TheexactmechanismofmothertochildtransmissionofHIVremainsunknown.Transmissionmayoccurduring
intrauterinelife,delivery,orbreastfeeding.Thegreatestriskfactorforverticaltransmissionisthoughttobe
advancedmaternaldisease,likelyduetoahighmaternalHIVviralload. [3]Unfortunately,about30%ofpregnant
womenarenottestedforHIVduringpregnancy,andanother1520%receivenoorminimalprenatalcare,thereby
allowingforpotentialnewborntransmission. [4]
Epidemiology
UnitedStatesstatistics
Earlyintheacquiredimmunodeficiencysyndrome(AIDS)epidemic,womenwererarelydiagnosedwithHIVor
AIDS,butby2005,womenrepresented27%oftheestimated45,669newdiagnosisofHIV/AIDS,withthegreatest
riseamongyoungwomen. [5]About80%ofnewcasesinwomenintheUnitedStatesarecontractedthrough
heterosexualintercourse,20%bycontaminatedneedles,andmostoftheremainingcasesbymaternalchild
transmission.Testingofdonatedbloodhasessentiallyeliminatedbloodtransfusionsasasourceofinfection.
OfwomenwithAIDS,71%werediagnosedbetweentheagesof25and44,implyingthatmanyofthemmayhave
beeninfectedasadolescents.IntheUnitedStates,AfricanAmericanandHispanicwomenrepresent25%ofthe
femalepopulationbutaccountfor82%ofthetotalnumberofwomenwithAIDS.Furthermore,womenofcolor
accountfor80%ofnewlydiagnosedHIV/AIDScases. [6]
Internationalstatistics
TheJointUnitedNationsProgrammeonHIV/AIDS(UNAIDS)hasestimatedthat,in2008,approximately33.4
millionpeopleworldwide(1%oftheglobaladultpopulationaged1549y)wereinfectedwithHIV,adeclinefrom
2006(39.5millionreportedatthattime)67%ofallpeoplelivingwithHIVworldwideliveinsubSaharanAfrica,and
91%ofallnewinfectionsamongchildrenoccurthere. [7]
Morethan500,000babiesworldwidecontractHIVfromtheirmothers90%ofthesecasesoccurindeveloping
countries.In2005,AIDSclaimedanestimated2.43.3millionlivesmorethan500,000ofwhichwerechildren.One
thirdofthesedeathswereinsubSaharanAfrica. [5]
ProphylaxisandPregnancyOutcome
TheAntiretroviralPregnancyRegistry,wherecliniciansshouldreportcasesofexposuretoantiviraltherapyin
pregnancy,containsapproximately5,000reportedexposuresandnotesnoincreaseinthecongenitalmalformation
ratewithexposuretoantiretroviralmedications,eveninthefirsttrimester,withtheexceptionofefavirenz.Early
exposuretoefavirenzhasbeenassociatedwithneuraltubedefects.
Concernwasraisedthatantiretroviraltherapymayincreasetheincidenceofadversepregnancyoutcomes.Several
studieshaveshownthatzidovudinemonotherapyhadnonegativeeffectonpregnancy.
AlthoughdatafromcohortsintheUnitedStateshavenotshownanincreasedriskofpretermbirthwithcombination
therapy,aEuropeancollaborativestudyshowedanincreasedriskofpretermlaborinwomeninfectedwithHIVwho
weretakingcombinationantiretroviraltherapy,withanoddsratioforpretermbirthof1.8forcombinationtherapy
withoutaproteaseinhibitorand2.6forcombinationtherapythatincludedaproteaseinhibitor. [8]
InaUSstudyofpregnantwomeninfectedwithHIV,theoverallrateofadversepregnancyoutcome,including
prematurity,lowbirthweight,stillbirth,andabnormalApgarscores,wassimilarinwomenwhoreceivedantiretroviral
therapyduringpregnancyandthosewhodidnot. [9]Ofthe2123womeninthestudy,1590receivedmonotherapy,
396receivedcombinationtherapywithoutaproteaseinhibitor,and137receivedcombinationtherapywitha
proteaseinhibitor1143didnotreceiveantiretroviraltherapy.
Ratesofprematurityandextremeprematuritydidnotdiffersignificantlyaccordingtoantiretroviralregimen.
Althoughtheriskoflowandverylowbirthweightwasgreaterinthegroupreceivingaproteaseinhibitor,theresults
http://emedicine.medscape.com/article/1385488overview
1/10
6/8/2015
HIVinPregnancy
didnotreachstatisticalsignificance.Furthermore,thismaybeareflectionofhigherviralloadoradvancedstageof
diseaseratherthanexposuretoproteaseinhibitors. [9]
Inamorerecentretrospectivestudy(20042012)thatevaluatedUSinfantgrowthpatternsduringtheirfirstyearof
lifeamongthoseborntoperinatallyHIVinfected(PHIV)(32infants,25mothers)andnonperinatallyHIVinfected
(NPHIV)mothers(120infants,99mothers)whoreceivedcare,infantsofPHIVmothershadlowermeanlengthfor
agezscores(LAZ)thatwereassociatedwithbirthlength.Othersmallforgestationalageanthropometricparameter
associationsincludedthoseofbirthweightandweightforagezscores(WAZ)andthoseofbothbirthlengthand
weightwithweightforlengthzscores(WLZ).TheinvestigatorsalsoreportedanassociationbetweendeliveryHIV
RNAlevelbelow400copies/mLwithincreasedWAZandWLZ. [10]
Alargemetaanalysisthatincludedarticlesfromseveralcountriesbetween1998and2006showedthatoverall,
highlyactiveantiretroviraltherapy(HAART)didnotincreasetheriskofprematurityhowever,theuseofregimens
withproteaseinhibitorsseemedtoincreaseprematurityslightly. [11]
ApossibleassociationexistsbetweenHAARTandpreeclampsia. [12]
ThedevelopmentofglucoseintolerancemaybemorecommoninpregnantwomenwithHIV.Originallythoughtto
beassociatedwithproteaseinhibitors,gestationaldiabetesappearstobesomewhatincreasedregardlessofthe
medicationregimen.Assuch,duringpregnancy,womenshouldbescreenedandmonitoredforglucoseintolerance.
[13]
HIVandPregnancyPlanning
PreliminarydatasuggestthatwomenwithHIVmaysufferfromsubfertility.Conceptionincoupleswhohavenever
conceivedmayoccurinamedianof6monthswith2actsofintercourseduringtheovulatoryperiodofthecycle.
Witheachact,theriskofsexualtransmissionmustbeconsideredeveninthepresenceofanundetectableviral
load.ConductingtestingandconsideringreproductivetechniquesinwomeninfectedwithHIVmaybeworthwhilein
anefforttoreducetheriskofinfectiontoahealthypartner.
Incouplesplanningapregnancywhereonlythemalepartnerisinfected,naturalconceptioncarriesariskofsexual
transmissiontotheuninfectedfemale.Counselingprovidedtosuchcouplesshouldincludestrategiestominimize
HIVtransmission.Optionsincludeadoption,spermdonation,andassistedreproductiontechniques.While
antiretroviraltherapycanreduceviralloadinthebloodtoundetectablelevels,somereportshaveshownthatmen
canstillhaveasubstantialviralconcentrationinsemeninthepresenceofanundetectableplasmaviralload.
Whenpossible,confirmationofundetectableseminalplasmaviralloadmaybeconsidered.IfHIVviralloadcannot
besuppressed,semenwashinghasbeenproposedandmaydecreasetheHIVRNAandDNAtoundetectable
levels.Afterprocessingandrecheckingforresidualcontamination,thespermatozoacanbeusedforintrauterine
inseminationorinvitrofertilization.
PregnancydoesnotappeartoinfluencetheprogressionofHIVdisease. [14,15]AlargecohortofFrenchwomenwith
knownseroconversiondatesnotedapregnancyadjustedrelativeriskofprogressionfromHIVtoAIDSof0.7. [16]
Furthermore,pregnancydoesnotseemtoaffectsurvivalofwomeninfectedwithHIV. [17]
Forserodiscordantcoupleswhowanttoconceive,theuseofantiretroviraltherapy(ART)isrecommendedforthe
HIVinfectedpartner,withthestrengthoftherecommendationdifferingbasedontheCD4cellcountoftheinfected
partner.Additionally,NIHguidelinesincludediscussionregardingpreexposureprophylaxis(PrEP)studiesin
heterosexualcouples.NewrecommendationsregardingpericonceptionadministrationofantiretroviralPrEPforHIV
uninfectedpartnersmayofferanadditionaltooltoreducetheriskofsexualtransmission.Theguidelinesinclude
informationoncounseling,laboratorytesting,andmonitoringofindividualsonPrEPandtheimportanceofreporting
uninfectedwomenwhobecomepregnantonPrEPtotheAntiretroviralPregnancyRegistry. [18,19,20]
HIVinfectionriskreductionstrategiesinconjunctionwithrelativelyinexpensivefertilityawarenessmethods(FAMs)
maybeusefulforcounselingHIVserodiscordantcoupleswhowanttoconceive. [21]Suchmethodsincludeuseof
accessibleandhighlysensitive,butpoorlyspecific,strategieslikethecalendarmethod,basalbodytemperature
measurements,andcervicovaginalmucussecretionfeatures.Urinaryluteinizinghormonetestinghashighspecificity
andcostwithlesssensensitivity.Timedcondomlesssexhaslowcostbutnecessitatesunderstandinghowto
preciselypredictthefertileperiodinamenstrualcycle. [21]
PatientEducation
Approximately30%ofwomenintheUnitedStatesarenottestedforHIVduringpregnancy.Reasonsfordeclining
shouldbeexploredandpatientscounseledappropriately.Testingstrategiesalsoincludereofferingscreeninginthe
thirdtrimestertowomenwhodeclinedfirsttrimesterscreeningorwhoareinhighriskgroups.TheCentersfor
DiseaseControlandPrevention(CDC)recommendsroutinethirdtrimesterscreeninginwomenwithhighrisk
behaviorsorwhoexhibitsignsorsymptomsofthedisease. [4]
ClinicianswhocareforwomenwithHIVneedtoprovidefamilyplanningservicesandcounselingregarding
optimizinghealthstatus.Thisincludesencouragingcompliancetomedicationregimens,cessationofsmoking,and
updatingimmunizations.
Stressingtheimportanceoftakingtheirmedicationregularlytodecreasethepossibilityofthedevelopmentof
antiretroviraldrugresistancemayencouragewomentocomplywiththerapy.Cigarettesmoking,concurrentuseof
drugs(cocaine,heroin),andunprotectedintercoursehavebeenassociatedwithincreasedriskofperinatal
transmission.
Itisencouragingtonotetherehasbeenasubstantialreductioninsubstanceuseinthepast2decades. [22]Ina
retrospectivestudyovera23yearperiod(19902012)thatevaluateddatafromtwoprospectivecohortstudies
(WomenandInfantsTransmissionStudy,SurveillanceMonitoringforAntiretroviralTherapyToxicitiesStudy),
investigatorsnotedadramaticdecreaseinsubstanceuseamong5451HIVinfectedpregnantwomen(1990:82%
2012:23%).Therewasasignificantdeclineinuseofeachsubstancebetween1990and2006,whenitreacheda
plateau,whichtheinvestigatorssuggestedmayhavebeencausedbyanepidemiologictransitionoftheHIV
epidemicamongUSwomen. [22]Substanceusewasinverselyassociatedwithreceivingantiretroviraltherapy.
Womenwithmultiplepregnancieswithsubstanceuseintheirpreviouspregnancywereathigherriskofsubstance
http://emedicine.medscape.com/article/1385488overview
2/10
6/8/2015
HIVinPregnancy
useintheirnextpregnancy. [22]
Unfortunately,15%ofwomeninfectedwithHIVreceivenoorminimalprenatalcare,and20%donotinitiate
prenatalcareuntillateinthethirdtrimester.Womenwhoarenottreatedduringpregnancyshouldbetreatedwith
oneoftheappropriateintrapartumantiretroviraldrugregimens.
Evenintheabsenceofantepartumtreatment,intrapartumandearlyneonatalprophylaxiscanreducethemotherto
childtransmissionrisk.Womenshouldbeextensivelycounseledregardingtheabilitytodecreasetheriskof
perinataltransmissionwithhighlyactiveantiretroviraltherapy(HAART)prophylaxisortreatment.Inwomenwhoare
beingtreatedwithHAARTandplanningapregnancy,theteratogenicpotentialofcertainantiretroviralmedications
mustbereviewedandeffectivecontraceptiondiscussed.Thesemedicationsshouldbestoppedpriortoplanninga
pregnancy.
HistoryandPhysicalExamination
History
Inpregnancy,theinitialhistoryshouldassessthestatusofthepatientsHIVdisease(eg,CD4+Tcellcount,viral
load),theneedforbeginningoralteringantiretroviralmedication,andwaystoreduceperinataltransmission.A
carefulreviewofthemedicalandsurgicalhistory,gynecologichistory,highriskhabits,andpreviousobstetrichistory
shouldbedoneatthefirstprenatalvisit.
Physicalexamination
Duringpregnancy,acompletephysicalexaminationmustbeperformed.Knowledgeofthenormalphysiologic
changesofpregnancy,suchasanenlargedthyroidglandandasystolicmurmur,isimportanttodifferentiatefrom
diseaseprocess.HIVinfectioncanaffectessentiallyallbodysystems.
Screening
TheAmericanCongressofObstetricsandGynecology(ACOG)recommendsroutineHIVscreeningforwomenaged
1964yearsandtargetedscreeningforatriskwomenoutsideofthisagereference.Allpregnantwomenshould
havetheirHIVserostatusevaluatedwhentheyfirstpresentforprenatalcare.
WomenshouldhavetherighttorefusetestingafterbeinginformedthatHIVtestingwillbedrawnaspartoftheir
routineprenatalpanel.Thisoptoutapproachtoprenatalscreening,asadvocatedbytheInstituteofMedicine,is
associatedwithhighertestingratesamongpregnantwomen.However,severalstateshavelawsthatprohibitthis
approachandmandatethatpatientssignconsentformsfortesting,knownastheoptinapproach. [23]
ELISA
Themostcommonscreeningtestisanenzymelinkedimmunosorbentassay(ELISA),whichlooksforthepresence
ofantibodies.Ifthistestresultispositive,theELISAisrepeatedtoeliminatelaboratoryerrorpriortoproceedingto
aconfirmatorytestbyWesternblot.TheELISAhas98%sensitivity.Falsenegativeresultsmayoccurearlyinthe
disease,andfalsepositiveresultshavebeenreportedaftercertainvaccines.Repeattestingseveralmonthslater
usuallyconfirmsseronegativityinsuchcases.ApositivetestissentforWesternblot.
Westernblot
FortheWesternblot,specificviralproteinsareseparatedbyelectrophoresis,andreactionofantibodyto3proteins
mustoccurforthetesttobeconsideredpositive.Indeterminateresultsoccurwhen1or2oftheproteinsare
present.Inlowriskpopulations,indeterminateresultsusuallyreverttonegativeoverseveralmonths.Westernblot
hasafalsepositiverateof1in20,000.
Bloodcountsandviralload
ForpregnantwomeninfectedwithHIV,inadditiontothestandardprenatalassessment,continuedassessmentof
HIVstatusisimportant.Acompletebloodcounttoassessanemiaandwhitebloodcellcountaswellasrenaland
liverfunctiontestsshouldbeincluded.InitialevaluationincludesCD4+counts,whichhelpdeterminethedegreeof
immunodeficiency.
Viralload,determinedbyplasmaHIVRNAcopynumber(copies/mL)assessestheriskofdiseaseprogression.The
viralloadisimportantindecisionsregardingmaternaltreatmentanddeliverymanagementhowever,because
perinatalHIVtransmissioncanoccurevenatloworundetectableHIVRNAcopynumbers,theviralloadisnotused
inpregnancytodecidewhethertostartantiretroviralmedications.
Ifaviralloadisdetected,antiretroviraldrugresistancestudies(HIVgenotype)shouldbeperformedbeforestarting
therapyunlessthediagnosisismadelateinthepregnancy,inwhichcasestartingmedicationswhileawaitingresults
isrecommended.Ingeneral,pregnancyhasnotbeenassociatedwithariskofrapidprogressionofHIV. [17]
Withappropriatetherapy,theviralloadshoulddropby1logwithinthefirstmonthandbecomenondetectablewithin
6monthsafterinitiatingtreatment.Thehighertheviralload,thelongerthedecreasemaytakehowever,iftheviral
loadpersistsorincreasesat6months,treatmentfailuremustbeconsidered.
Lipidprofileandultrasound
Otherlaboratorystudiesshouldincludealipidprofile,whichisnotusuallyobtainedinpregnancy.Although
cholesterolnormallyincreasesinpregnancy,baselinevaluesarerequired,ascertainmedicationshavebeen
associatedwithincreasedtriglycerideandcholesterollevels.Evaluationofotherinfectiousdiseasestatesand
possibleopportunisticinfections,suchassyphilis,cytomegalovirus,andtoxoplasmosis,alsoneedstobedone.
Initialobstetricultrasonographyforviabilityanddatingisimportantfordeterminingtreatmentandplanningdelivery.
Potentialteratogenicityishighestduringthefirsttrimester,andsomepatientsmayconsiderdelayingtreatmentuntil
afterthefirst12weeksofpregnancy.Inwomenwhoareseverelyill,therisksandbenefitsofthisdelaymustbe
weighed.Atargetedultrasonographymaybewarranteddependingonmedicationexposure.
http://emedicine.medscape.com/article/1385488overview
3/10
6/8/2015
HIVinPregnancy
Hepatitistesting
HepatitisBsurfaceantigenstatusisrecommendedforallpregnantwomen.InthecaseofacutehepatitisB
infection(HBV),theriskofverticaltransmissionalsovarieswithgestationalage,withan8090%riskof
transmissiontotheoffspringiftheinfectionoccursinthethirdtrimester. [23]WomenwhoarecoinfectedwithHIV
andchronichepatitisBmayrequiredifferentmanagementinpregnancy.
CoinfectionwithHIVandhepatitisCvirus(HCV)iscommonandmayrangefrom1754%. [24]Thediagnosisof
hepatitisCisconfirmedbyidentificationofthehepatitisCantibodyviaanELISAtest.FalsenegativeHCVtest
resultsmayoccuriftheCD4countisverylow.Morespecifictests,(eg,hepatitisCviralRNAdetectionby
polymerasechainreaction)areavailable.Highmaternalviraltitershavebeenassociatedwithanincreasedriskof
verticaltransmission.
AllwomenwhoarechroniccarriersofHBVorHCVshouldinformsexualpartners,householdcontacts,andneedle
sharingcontactsandreviewprecautionstodecreasetransmission.
Opportunisticinfectionassessment
AssessmentoftheneedforprophylaxisagainstPneumocystisjirovecipneumonia(PCP)orMycobacteriumavium
complex(MAC)infectionisnecessary.ForwomenwithlowCD4counts,prophylaxisforPCPiswithtrimethoprim
sulfamethoxazole(TMPSMX).Duetopotentialteratogenicity,aerosolizedpentamidinemaybesubstitutedinthe
firsttrimester,asitisnotabsorbedsystemically.ForprophylaxisofMAC,azithromycinisusedinplaceof
clarithromycinbecauseofpotentialteratogenicity. [14]
Othersexuallytransmitteddiseasetesting
Screeningforothermaternalsexuallytransmitteddiseasesisrecommendedinpregnancy.Forexample,screening
formaternalsyphilisisimportantnotonlyforthepreventionofcongenitalsyphilisbutalsobecausematernalsyphilis
hasbeenassociatedwithanincreasedriskofmothertochildtransmissionofHIV. [25]
Vaginalspeculumexaminationshouldbeperformedtoobtaincervicalcytologysmearandassaysforgonorrheaand
chlamydia.Allsexuallytransmitteddiseasesshouldbetreatedpromptly.Genitalwartsandvulvarintraepithelial
neoplasiaaremorecommonamongHIVseropositivethanHIVseronegativewomen,butwartregressionisas
commoninwomenwithHIVasthosewithoutandcancerisinfrequent. [26]WomeninfectedwithHIVhaveahigher
incidenceofcervicaldysplasia.
Vaccination
Vaccinationsshouldbekeptupdated.Duringpregnancy,liveattenuatedvaccines(eg,measlesmumpsrubella
[MMR],varicellavaccines)shouldbeavoided.Annualinfluenzavaccineandpneumococcalvaccineshouldbe
administeredtoallpregnantwomenwhoareHIVpositive.TheH1N1influenzavaccineshouldbeadministeredto
allpregnantwomenandissafeinwomenwithHIV.
Tuberculosistesting
CoinfectionwithHIVandtuberculosisisverycommonindevelopingnations.ImmunosuppressionfromHIV
infectioncontributesnotonlytoahigherrateoftuberculosisreactivationbutalsotoanincreaseddiseaseseverity.
Tuberculosisskintestingshouldbeperformedanda5mmpurifiedproteinderivative(PPD)resultinterpretedas
positive.Ifpositive,chestradiographycanbeperformedduringpregnancybecauseradiationriskisexceedinglylow.
Presentationduringlabor
Forwomenwhopresentinlaborandhavenothadprenataltesting,rapidtestingshouldbeoffered.Unlikethe
ELISA,therapidHIVtestisabloodorsalivaantibodytestandresultsareusuallyavailablewithinanhour.The
rapidtestisreportedtohaveahighnegativepredictivevalue(100%)andtobehighlysensitiveandspecific
(approaching100%)however,thepositivepredictivevalueinpregnancyvariesfrom44100%. [4]Patientswhotest
positiveinlaborbyELISAshouldbetreatedasHIVpositiveuntilconfirmatoryresultsareavailable.
AntiretroviralTherapy
Overview
Mothertochildtransmissionislinkedtoviralload.Assuch,antiretroviraltherapyshouldbeofferedtoallpregnant
womeninfectedwithHIVtoreducetheriskofperinataltransmissiontobelow2%. [27]Combinationantiretroviral
therapyshouldbeofferedinallcases.Aszidovudine(ZDV)istheonlyagentspecificallyshowntoreduceperinatal
transmission,itshouldbeusedwheneverpossibleaspartofthehighlyactiveantiretroviraltherapy(HAART)
regimen. [2]
Ifapregnantwomanhasreceivedantiretroviralmedicationinthepastbutisnotcurrentlyonanymedication,the
choiceofregimenmayvaryaccordingtothehistoryofprioruse,theindicationforstoppingtreatmentinthepast,
gestationalage,andresistancetesting.Inthissetting,ifthereisnoresistancetothedrugsandtheregimen
suppressedviralload,antiretroviralmedicationcanbeusedagain,butavoiddrugswithteratogenicpotentialor
adversematernaleffects.
IfapatientwhoisonaHAARTregimenpresentsforprenatalcare,continuinghertreatmentduringthefirst
trimesterisreasonable,providedthatcareistakentoavoidmedicationsthatarecontraindicatedinearlypregnancy.
HIVantiretroviraldrugresistancetestingisrecommendedifaviralloadisdetectable.Considerationsofdrugsnot
usuallyusedearlyinpregnancymaybenecessaryifdrugresistanceisconfirmedandthepatientreceivesextensive
counselingregardingriskandbenefits.
InanHIVinfectedpregnantwomanwhohasneverbeenexposedtoantiretroviralmedication,HAARTshouldbe
startedassoonaspossible,includingduringthefirsttrimester.Again,recommendationsarefordrugresistance
testingandcaretoavoidmedicationsthatmaypotentiallycauseadversematernalandfetaleffects.
http://emedicine.medscape.com/article/1385488overview
4/10
6/8/2015
HIVinPregnancy
IfprenatalHIVtestingwasnotperformedandarapidHIVtestreturnspreliminarilypositive,thepatientshouldbe
treatedlikeanyotherwomaninfectedwithHIV.Certainly,thegestationalageandobstetricalscenariomaydictate
thetreatmentoptionsavailable,butastheexposurerisktoantiretroviralmedicationisminimaltobothmotherand
fetus,antiretroviraltherapyshouldbeinitiated. [4]
Thepatientwithapositiverapidtestmustbecounseledregardingthepossibilityofafalsepositivescreen,andthe
resultsshouldbedocumentedaspreliminaryinthemedicalchart.Ifthistestwasperformedonarrivalinlabor,
treatmentwiththeZDVprotocolthroughlaborisrecommended,followedbyadministrationtotheneonateuntil
confirmatorytestingonthemotherbecomesavailable.
Antiretroviralregimens
TreatmentofwomeninfectedwithHIVshouldnotbewithheldbecauseofpregnancy.Althoughthedecision
regardingstartingormaintainingcurrentantiretroviraltherapyisbasedonthesamecriteriaasinnonpregnant
patients,severalconsiderationsmustbetakenintoaccountbecauseofpotentialeffectsonthefetus.
Theuseofthe3partZDVprophylaxisregimen,aloneorincombinationwithotherantiretroviralmedications,should
bediscussedandofferedtoallpregnantwomenbecauseZDVwasthefirstagenttoshowsignificantdecreasein
themothertochildtransmissionofHIV. [2]Theregimenchosenshouldalsotakeintoaccountpriortherapyand
responsetothatregimen,aswellasresistancetesting.Gestationalageandpotentialfetalandneonataltoxicity
mustalsobetakenintoaccountwhenselectingaregimen.
Themechanismofactionwithwhichthesedrugsreduceperinataltransmissionincludesloweringmaternalviral
loadhowever,asthesedrugscrosstheplacenta,thereappearstobeprenatalprophylaxisaswell.Thethird
component,prophylaxisofthenewborn,furtherdecreasestheriskofperinataltransmission.
Theantiretroviraldrugsusedinpregnancyfallbroadlyinto3categories:thenucleosideandnucleotideanalogue
reversetranscriptaseinhibitors(NRTIs),nonnucleosidereversetranscriptaseinhibitors(NNRTIs),andprotease
inhibitors(PIs).Thereareinsufficientdatatoallowrecommendationsregardingtheuseofentryinhibitorsor
integraseinhibitorsinpregnancy.
GuidelinesforperinatalARTwererevisedinJuly2012regardingwhichagentsareconsideredpreferred,alternative,
ortobeusedunderspecialcircumstances.Combinationregimens,usuallyincluding2NRTIswitheitheranNNRTI
or1ormoreproteaseinhibitors(PIs)arerecommended.Forfurtherinformation,seeTable1.
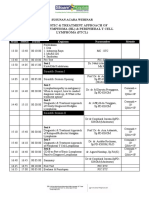
Table1.ARTagentsduringpregnancy[18](OpenTableinanewwindow)
ARTClass
Preferred*
Alternate
SpecialCircumstances InsufficientDatatoRecommend
NRTIs
zidovudine(ZDV)
abacavir
didanosine
lamivudine(3TC)
emtricitabine stavudine
tenofovir
NNRTIs
nevirapine
efavirenz
etravirine
rilpivirine
PIs
atazanavir
darunavir
indinavir
fosamprenavir
lopinavir+
ritonavir
saquinavir
nelfinavir
tipranavir
enfuvirtide
ritonavir
FusionInhibitors
maraviroc
Integrase
Inhibitors
raltegravir
*ZDVplus3TCisarecommendeddualNRTIbackboneregimenplusanNNRTIand1ormorePIsforpregnant
womenwithHIV
http://emedicine.medscape.com/article/1385488overview
5/10
6/8/2015
HIVinPregnancy
Nucleotideanaloguereversetranscriptaseinhibitors
TheNRTIsaregenerallywelltoleratedandcrosstheplacenta.TheFDAhasclassifiedtheseaspregnancyclassB
orC,dependingontheagent.ThesedrugsdobindtomitochondrialDNAgammapolymeraseandmaycause
mitochondrialdysfunctionmanifestingascardiomyopathy,neuropathy,lacticacidosis,andliverdysfunction.Genetic
susceptibilitytothesedrugsmayplayarole,andtheeffectsusuallyresolvewithcessationofthemedication. [1]
Thecombinationofdidanosineandstavudinehasbeenassociatedwithlacticacidosisandhepaticfailureleadingto
fatalitiesandshouldbeusedwithcautionoronlyincaseswhereotherNRTIscannotbeusedduetoresistanceor
toxicity.Finally,ZDVandstavudinehaveoverlappingtoxicitiesandareantagonisticandshouldbeavoidedin
combination. [27]
Nonnucleosidereversetranscriptaseinhibitors
FiveNNRTIsareFDAapproved:delavirdine(Rescriptor),efavirenz(Sustiva),etravirine(Intelence),nevirapine
(Viramune),andrilpivirine(Edurant).AlthoughlessinformationisavailableregardingNNRTIuseinpregnancy,
nevirapineandefavirenzbothcrosstheplacenta.Themostcommonsideeffectisrash,whichcanoccurinupto
17%ofpatientsonnevirapine. [14]
Useofefavirenzisnotrecommendedinthefirsttrimesterbecauseofreportedcasesoffetalneuraltubedefects.
TheFDAhaschangedthepregnancyclassificationofthisdrugtocategoryD. [28]
Severenevirapineassociatedskinrashandhepatictoxicityhavebeenreportedinpregnancy.Thepotentiallyfatal
hepatotoxicityappearstobeincreasedinwomen,duringpregnancy,andinpatientswithaCD4+Tcellcount
greaterthan250cells/mL.Becauseofthesesignificantcomplications,nevirapineshouldnotbeusedasfirstline
therapyunlessnootheroptionisavailable.
InwomenwhoseCD4+Tcellcountswerebelow200cells/mLandwhowerepreviouslyexposedtoperipartum
singledosenevirapine,ritonavirboostedlopinavirplustenofoviremtricitabinewassuperiortonevirapineplus
tenofoviremtricitabineforinitialantiretroviraltherapy. [29]
InchildrenpreviouslyexposedtosingledosenevirapineforperinatalpreventionofHIVtransmission,zidovudineand
lamivudineplusritonavirboostedlopinavirforantiretroviraltreatmentresultedinbetteroutcomesthantreatment
withzidovudineandlamivudineplusnevirapine. [30]
Proteaseinhibitors
Proteaseinhibitorsdonotcrosstheplacentaeasily,andnoteratogeniceffectshavebeennotedinanimals.They
areclassifiedasclassBorCbytheFDA.
AlsoseetheMedscapeDrugs&DiseasestopicAntiretroviralTherapyforHIVInfection.
PeripartumTreatment
InanypregnantwomaninfectedwithHIVwhopresentsinlabor,whetherherHIVpositivestatuswaspreviously
knownorwasdeterminedbyrapidtestresult,morethanonetreatmentoptionisavailableduringlaboranddelivery.
AllHIVinfectedwomenwithHIVRNA400copies/mL(orunknownHIVRNA)neardeliveryshouldbeadministered
IVzidovudine(ZDV)duringlabor,regardlessofantepartumregimenormodeofdelivery.IVZDVisnolonger
requiredforHIVinfectedwomenreceivingcombinationARTregimenswhohaveHIVRNA<400copies/mLnear
delivery. [18]
ZDVisgivenintravenouslyduringlaboratadoseof2mg/kginfusedover1hour,followedbyacontinuousinfusion
of1mg/kgthroughoutlabor.Thisregimen,alongwithmaternalantepartumandinfantzidovudine,reducedperinatal
transmissionby66%overall. [18]Ifthepatientishavingaplannedcesareandelivery,theIVinfusionshouldbegin3
hoursbeforetheprocedure. [14,27,31]AnotheroptionisZDVinfusionfollowedbyasingledoseof200mgof
nevirapine.Thisregimenshouldbefollowedbylamivudine(3TC)150mgevery12hours.Ifthelatterregimenis
usedinpregnancy,thepatientmustcontinueZDV/lamivudine(Combivir)foratleast7dayspostpartumtoavoid
nevirapineresistance. [14]
WomenwithdocumenteddrugresistancetoZDVorwhoseantepartumregimendidnotincludeZDVshouldstillbe
giventheintravenousZDVprotocolduringlaboranddeliveryorbeforecesareandelivery. [14,31]Furthermore,the
otherantiretroviralagentsmustbecontinuedonschedulethroughouttheintrapartumorpreoperativeperiod.
StavudineistheonlyagentthatcanantagonizeZDVandshouldbestoppedpriortotheIVinfusionofZDV. [27]
Inpatientsattemptingavaginaldelivery,allinvasiveproceduressuchasamniotomy,internalfetalscalpelectrode,
orscalpsamplingshouldbeavoided,asthesemayincreasetheriskoftransmission.
WhenHAARTisgivensolelyforpreventionofperinatalHIVtransmission,itmaybestoppedinthepostpartum
period.TheriskofpromotingthedevelopmentofresistantviralstrainsbyusingshortcoursesofHAARTcanbe
decreasedbyusingamaximallysuppressiveregimenanddiscontinuingallagentsatthesametime.Theexception
remainsiftheregimenincludesanucleosidereversetranscriptaseinhibitor(NRTI).TheNRTIshouldbecontinued
foranadditional7daystodecreasetheriskofresistance. [14]
InfantARTprophylaxis [18]
AllHIVexposedinfantsshouldreceivezidovudineinthefollowingdoses:
<30weeksgestation:2mg/kgPOor1.5mg/kgIVBIDafterage4weeks,advanceto3mg/kgPOor2.3
mg/kgIVq12hr
>30to<35weeksgestation:2mg/kgPOBIDafterage15days,advanceto3mg/kgPOor2.3mg/kgIV
q12hr
>35weeksgestation:4mg/kgPOor3mg/kgIVBIDx6weeks
Initiateassoonafterdeliveryaspossible(preferablywithin612hours)andcontinuethroughage6weeksand
administerbirththrough6weeks.
AdditionalprophylaxiswithnevirapineisneededforHIVexposedinfantsofwomenwhodidnotreceiveantepartum
http://emedicine.medscape.com/article/1385488overview
6/10
6/8/2015
HIVinPregnancy
ARTatthefollowingweightsanddosages:
Birthweight1.52kg:8mg/dosePO
Birthweight>2kg:12mg/dosePO
Administer3dosesinthefirstweekoflife1stdose48hoursafterbirth,give2nddose48hoursafter1stdose,and
3rddose96hoursafter2nddose.
HepatitisCoinfection
ThecurrentrecommendationfortreatingwomencoinfectedwithHIVandHBVistotreatthesewomenwith
tenofovirandlamivudineoremtricitabine. [32]All3haveshownactivityagainstHBV.Ametaanalysisfoundthatthe
useoflamivudineeffectivelypreventsmothertochildtransmission,eveninpregnantwomenwhohaveahigh
degreeofHBVinfectiousnessinlatepregnancy. [33]
Althoughdataareinsufficientfortheuseoftenofovirinpregnancy,thebenefitslikelyoutweightherisksinwomen
withHBV/HIVcoinfection.Womenreceivingtreatmentshouldbeadvisedofthesignsandsymptomsofliver
toxicity,andregularfollowupoftransaminaselevelsiswarranted.TheinfantshouldreceivehepatitisB
immunoglobulinandstartthe3doseseriesofhepatitisBvaccinewithinthefirst12hoursoflife. [18]
PregnancydoesnotappeartoalterthecourseofHCVinfectionhowever,coinfectionwithHIVdoesappearto
increasetheriskofperinataltransmissionofHCV.Assuch,a3drugantiviralcombinationisrecommended
regardlessoftheviralload.AswithHBVcoinfection,patientsshouldbemadeawareofthesignsandsymptomsof
livertoxicity,andtransaminasesshouldbefollowedevery24weeks.
AswithHIV,prolongedruptureofmembranesmayincreasetheriskofperinatalHCVtransmissionhowever,the
dataremaininconclusiveregardingtheuseofcesareansectiondeliverytodecreasetheriskoftransmission.As
such,deliveryrecommendationsarebasedontheHIVstatus.InfantscanbeevaluatedbytestingHCVRNAat2
and6monthsofageorHCVantibodyafter15monthsofage. [18]
CesareanDelivery
Cesareandeliverymustbediscussedandthepatientcounseledregardingthepossibilityofanunnecessarysurgical
procedureshouldthefinalHIVresultbenegative. [18]Careshouldbeindividualizedaccordingtoclinicalscenario.
Earlystudiesregardingcesareandeliveryandtransmissionriskshowedconflictingresults.Cesareandeliverybefore
theonsetoflabormaypreventmicrotransfusionthatoccurswithuterinecontractions,andavoidingvaginaldelivery
eliminatesexposuretovirusinthecervicovaginalsecretionsandbloodattimeofdelivery.
Inthelate1990s,prospectivecohortstudiesnotedadecreaseinmothertochildtransmissioninwomenon
zidovudine(ZDV)whounderwentelectivecesareandeliverycomparedwithwomenwhodidnottakeZDV
prophylaxis. [34,35]In1999,resultsfromalargemetaanalysisofindividualpatientdatafrom15prospectivecohort
studiesdemonstrateda50%reductionofverticaltransmissionwiththeuseofelectivecesareandeliveryforwomen
withHIV,afteradjustingforantiretroviraltherapy,maternalstageofdisease,andinfantbirthweight.
Ofnote,verticaltransmissionriskdidnotchangewhenthestudygroupwaslimitedtothosewomenwhohad
ruptureofmembranesshortlybeforesurgery.Thetransmissionriskwasdecreasedbyabout80%forwomenwho
hadbothanelectivecesareandeliveryandweretakingantiretroviralmedication. [36]
Inthesameyear,ACOGissuedanopinionthatelectivecesareandeliveryshouldbediscussedandofferedtoall
pregnantwomenwhowereHIVpositiveat38weeksgestationtoavoidthepotentialriskofspontaneouslaborand
ruptureofmembranes. [31]
ThesestudiesdidnotadjustforviralloadandwereperformedbeforeHAARTcameintouse.InpatientsonHAART
withanundetectableviralload(<1000copies),theriskoftransmissionisverylow,andwhethercesareandelivery
offersanyfurtherbenefitremainsunknown.
ThisledtoanupdatedACOGstatementin2000,statingthatwomeninfectedwithHIVwhoseviralloadsare
greaterthan1,000copies/mLshouldbecounseledregardingthepotentialbenefitofscheduledcesareandeliveryto
furtherreducetheriskofverticaltransmissionofHIVbeyondthatachievedwithantiretroviraltherapyalone. [31]
However,dataareinsufficienttodemonstrateabenefitforneonatesofwomenwithviralloadslessthan1,000
copies/mL.
Longerdurationofrupturedmembranesmaybeassociatedwithahigherrateofmothertochildtransmission.The
InternationalPerinatalHIVgroupmetaanalysisfoundthattheriskofverticaltransmissionincreasedby2%for
everyincreaseof1hourinthedurationofrupturedmembranes.Ifcesareandeliveryisperformedaftertheonsetof
labororruptureofmembranes,thebenefitofsurgerymaybelost.Inthisscenario,adecisionregardingtherouteof
deliveryshouldbeindividualized. [31,36]
OperativeriskmayoutweighthepotentialbenefitoffurtherreducingHIVtransmission.InastudybyLouisetalthat
comparedtheoutcomeofcesareansectionin378womeninfectedwithHIVandinmorethan54,000uninfected
women,HIVinfectedwomenhadahigherrateofintraoperativeneedforbloodtransfusionaswellasincreased
incidenceofpostpartumendometritis,sepsis,pneumonia,admissiontotheintensivecareunit,andmaternaldeath.
[37]
IntheHIVinfectedgroup,morbidityandmortalitywereassociatedwithinfectionandrelatedtoimmunefunction,
withthegreatestriskbeingforwomenwithaCD4countlessthan200cells/mL. [37]
BecausemorbidityisincreasedinwomeninfectedwithHIVwhoundergocesareandelivery,prophylacticantibiotics
shouldbeadministered.Scheduledcesareandeliveryshouldbediscussedandrecommendedforwomenwithviral
loadsgreaterthan1000copies/mL,whetherornottheyaretakingantiretroviraltherapy.
Discussionoftheoptionofscheduledcesareandeliveryshouldbeginasearlyaspossibleinpregnancywithevery
pregnantwomaninfectedwithHIV,togiveheranadequateopportunitytoconsiderthechoiceandplanforthe
procedure.Therisks,whichappeartobegreaterforthemother,mustbebalancedwiththebenefitsexpectedfor
theneonate.Thepatient'sautonomymustberespectedwhenmakingthedecisiontoperformacesareandelivery,
http://emedicine.medscape.com/article/1385488overview
7/10
6/8/2015
HIVinPregnancy
becausethepotentialformaternalmorbidityissignificant.
Consultationandfollowupwithspecialistsininfectiousdiseaseandmaternalfetalmedicineisrecommended.
DietandActivity
Duringpregnancy,ahealthy,wellbalanceddietisrecommended,andthisrecommendationisnotalteredbyHIV.
Certainfoodsneedtobelimitedandavoidedduringallpregnancies.Alcoholshouldbeavoided.Generally,eating
fishlowinmercurycontentisrecommended.Caffeinemustalsobelimited,aswellasfoodshighinnitritesandsoft
cheeses.CurrentavailableevidencesuggeststhatvitaminAsupplementationduringpregnancy(nottoexceed
10,000IUinthefirsttrimester)improvesbirthweight. [38]Lightexerciseisrecommendedinpregnancy,andthis
recommendationisnotalteredbyHIVinfection.Walkingandswimmingareexcellentprogramsduringpregnancy.
Womenshoulddiscusstheirexerciseroutinewiththeirphysician.
DeterrenceandPrevention
Currently,novaccineisavailableforHIVtherefore,preventioniscrucialtodecreasingtheriskoftransmission. [39]
Womenmustbecounseledonmethodstoavoidtransmissiontoothers,includingsafesexpracticeandavoiding
donationofbloodororgans.
Regularuseoflatexcondomsandavoidanceofunprotectedintercourseisimportant.Treatmentofgenitaltract
infectionsandinflammationinbothpartnersisimportanttoavoidmucosalbreaks.Thefrequentuseofnonoxyynol9
vaginalgelhasbeenassociatedwithincreasedriskofHIVacquisitioninthehighriskpopulation.Womenshouldnot
sharetoothbrushesorrazors,assmallamountsofbloodmaybepresent.
Inareasoftheworldwheresafealternativesareavailable,breastfeedingisnotrecommended.Thisalsoappliesto
womenonantiretroviraltherapy. [5,14]Passageofantiretroviralsintobreastmilkhasbeenshownforseveralagents,
includingzidovudineandlamivudine. [18]
ContributorInformationandDisclosures
Author
TeresaMarino,MDAssistantProfessor,AttendingPhysician,DivisionofMaternalFetalMedicine,Tufts
MedicalCenter,TuftsUniversitySchoolofMedicine,Boston,Massachusetts
Disclosure:Nothingtodisclose.
SpecialtyEditorBoard
FranciscoTalavera,PharmD,PhDAdjunctAssistantProfessor,UniversityofNebraskaMedicalCenter
CollegeofPharmacyEditorinChief,MedscapeDrugReference
Disclosure:MedscapeSalaryEmployment
ChiefEditor
ThomasChihChengPeng,MDProfessor(Collateral),DepartmentObstetricsandGynecology,Virginia
CommonwealthUniversitySchoolofMedicine,VCUHealthSystem
ThomasChihChengPeng,MDisamemberofthefollowingmedicalsocieties:AmericanCollegeof
ObstetriciansandGynecologists,AmericanInstituteofUltrasoundinMedicine,andSocietyforMaternalFetal
Medicine
Disclosure:Nothingtodisclose.
References
1. BrinkmanK,terHofstedeHJ,BurgerDM,SmeitinkJA,KoopmansPP.Adverseeffectsofreverse
transcriptaseinhibitors:mitochondrialtoxicityascommonpathway.AIDS.Oct1199812(14):173544.
[Medline].
2. ConnorEM,SperlingRS,GelberR,etal.Reductionofmaternalinfanttransmissionofhuman
immunodeficiencyvirustype1withzidovudinetreatment.PediatricAIDSClinicalTrialsGroupProtocol076
StudyGroup.NEnglJMed.Nov31994331(18):117380.[Medline].
3. GarciaPM,KalishPA,PittJetal.MaternallevelsofplasmaHIVtype1RNAandtheriskofperinatal
transmission.WomenandInfantsStudygroup.NewEnglandJournalofMedicine.1999341:385393.[Full
Text].
4. RahangdaleL,CohanD.Rapidhumanimmunodeficiencyvirustestingonlaboranddelivery.Obstet
Gynecol.Jul2008112(1):15963.[Medline].
5. CentersforDiseaseControlandPrevention(CDC).EpidemiologyofHIV/AIDSUnitedStates,19812005.
MMWRMorbMortalWklyRep.Jun2200655(21):58992.[Medline].
6. AmericanCollegeofObstetricsandGynecology.ACOGCommitteeOpinion.Humanimmunodeficiency
virusandacquiredimmunodeficiencysyndromeandwomenofcolor.ObstetGynecol.Aug2008112(2Pt
1):4136.[Medline].
7. JointUnitedNationsProgrammeonHIV/AIDS.AIDSepidemicupdate2009.Availableat
http://bit.ly/iHUsZK.AccessedJune17,2011.
8. Combinationantiretroviraltherapyanddurationofpregnancy.AIDS.Dec22200014(18):291320.
[Medline].
9. TuomalaRE,ShapiroDE,MofensonLM,BrysonY,CulnaneM,HughesMD.Antiretroviraltherapyduring
pregnancyandtheriskofanadverseoutcome.NEnglJMed.Jun132002346(24):186370.[Medline].
[FullText].
http://emedicine.medscape.com/article/1385488overview
8/10
6/8/2015
HIVinPregnancy
10. JaoJ,AgwuA,MhangoG,etal.Growthpatternsinthefirstyearoflifedifferininfantsborntoperinatally
vs.nonperinatallyHIVinfectedwomen.AIDS.Jan2201529(1):1116.[Medline].
11. KourtisAP,SchmidCH,JamiesonDJ,LauJ.UseofantiretroviraltherapyinpregnantHIVinfectedwomen
andtheriskofprematuredelivery:ametaanalysis.AIDS.Mar12200721(5):60715.[Medline].
12. ThorneC,NewellML.Thesafetyofantiretroviraldrugsinpregnancy.ExpertOpinDrugSaf.Mar
20054(2):32335.[Medline].
13. HittiJ,AndersonJ,McComseyG,etal.Effectofproteaseinhibitorbasedantiretroviraltherapyonglucose
toleranceinpregnancy.Abstract.13thConferenceonRetrovirusesandOpportunisticInfections.Feb2006.
14. WattsDH.Managementofhumanimmunodeficiencyvirusinfectioninpregnancy.NEnglJMed.Jun13
2002346(24):187991.[Medline].
15. MinkoffH,HershowR,WattsDH,FrederickM,ChengI,TuomalaR.Therelationshipofpregnancyto
humanimmunodeficiencyvirusdiseaseprogression.AmJObstetGynecol.Aug2003189(2):5529.
[Medline].
16. SaadaM,LeChenadecJ,BerrebiA,BongainA,DelfraissyJF,MayauxMJ.Pregnancyandprogressionto
AIDS:resultsoftheFrenchprospectivecohorts.SEROGESTandSEROCOStudyGroups.AIDS.Oct20
200014(15):235560.[Medline].
17. FrenchR,BrocklehurstP.TheeffectofpregnancyonsurvivalinwomeninfectedwithHIV:asystematic
reviewoftheliteratureandmetaanalysis.BrJObstetGynaecol.Aug1998105(8):82735.[Medline].
18. PerinatalHIVGuidelinesWorkingGroup.PublicHealthServiceTaskForceRecommendationsforuseof
antiretroviraldrugsinpregnantHIV1infectedwomenformaternalhealthandinterventionstoreduce
perinatalHIV1transmissionintheUnitedStates.NationalInstitutesofHealth.Availableat
http://www.aidsinfo.nih.gov/guidelines/html/3/perinatalguidelines/0/.AccessedNovember28,2012.
19. InterimguidanceforcliniciansconsideringtheuseofpreexposureprophylaxisforthepreventionofHIV
infectioninheterosexuallyactiveadults.MMWRMorbMortalWklyRep.Aug10201261(31):5869.
[Medline].[FullText].
20. BaetenJM,DonnellD,NdaseP,MugoNR,CampbellJD,WangisiJ,etal.Antiretroviralprophylaxisfor
HIVpreventioninheterosexualmenandwomen.NEnglJMed.Aug22012367(5):399410.[Medline].
21. LiaoC,WahabM,AndersonJ,ColemanJS.Reclaimingfertilityawarenessmethodstoinformtimed
intercourseforHIVserodiscordantcouplesattemptingtoconceive.JIntAIDSSoc.201518(1):19447.
[Medline].
22. RoughK,TassiopoulosK,KacanekD,etal.DramaticdeclineinsubstanceusebyHIVinfectedpregnant
womenintheUnitedStatesfrom1990to2012.AIDS.Jan2201529(1):11723.[Medline].[FullText].
23. AmericanCollegeofObstetricsandGynecology.ACOGCommitteeOpinionNo.389,December2007.
Humanimmunodeficiencyvirus.ObstetGynecol.Dec2007110(6):14738.[Medline].
24. ThomasSL,NewellML,PeckhamCS,AdesAE,HallAJ.AreviewofhepatitisCvirus(HCV)vertical
transmission:risksoftransmissiontoinfantsborntomotherswithandwithoutHCVviraemiaorhuman
immunodeficiencyvirusinfection.IntJEpidemiol.Feb199827(1):10817.[Medline].
25. MwapasaV,RogersonSJ,KwiekJJ,etal.Maternalsyphilisinfectionisassociatedwithincreasedriskof
mothertochildtransmissionofHIVinMalawi.AIDS.Sep11200620(14):186977.[Medline].
26. MassadLS,XieX,DarraghT,etal.GenitalWartsandVulvarIntraepithelialNeoplasia:NaturalHistory
andEffectsofTreatmentandHumanImmunodeficiencyVirusInfection.ObstetGynecol.Oct
2011118(4):831839.[Medline].[FullText].
27. MinkoffH.Humanimmunodeficiencyvirusinfectioninpregnancy.ObstetGynecol.Apr2003101(4):797
810.[Medline].
28. AntiretroviralPregnancyRegistrySteeringCommittee.AntiretroviralPregnancyRegistryInternational
InterimReportforJanuary1989throughJuly2005.[FullText].
29. LockmanS,HughesMD,McIntyreJ,ZhengY,ChipatoT,ConradieF,etal.Antiretroviraltherapiesin
womenaftersingledosenevirapineexposure.NEnglJMed.Oct142010363(16):1499509.[Medline].
30. PalumboP,LindseyJC,HughesMD,CottonMF,BobatR,MeyersT,etal.Antiretroviraltreatmentfor
childrenwithperipartumnevirapineexposure.NEnglJMed.Oct142010363(16):151020.[Medline].
31. AmericanCollegeofObstetricsandGynecology.Scheduledcesareandeliveryandthepreventionof
verticaltransmissionofHIVinfection.No.234.ObstetGynecol.2000.
32. [Guideline]AmericanCollegeofObstetricsandGynecology.ACOGPracticeBulletinNo.86:Viralhepatitis
inpregnancy.ObstetGynecol.Oct2007110(4):94156.[Medline].
33. ShiZ,YangY,MaL,LiX,SchreiberA.Lamivudineinlatepregnancytointerruptinuterotransmissionof
hepatitisBvirus:asystematicreviewandmetaanalysis.ObstetGynecol.Jul2010116(1):14759.
[Medline].
34. KindC,RudinC,SiegristCA,WylerCA,BiedermannK,LauperU.PreventionofverticalHIV
transmission:additiveprotectiveeffectofelectiveCesareansectionandzidovudineprophylaxis.Swiss
NeonatalHIVStudyGroup.AIDS.Jan22199812(2):20510.[Medline].
35. MandelbrotL,LandreauMascaroA,RekacewiczC,etal.Lamivudinezidovudinecombinationfor
preventionofmaternalinfanttransmissionofHIV1.JAMA.Apr252001285(16):208393.[Medline].
36. Themodeofdeliveryandtheriskofverticaltransmissionofhumanimmunodeficiencyvirustype1ameta
analysisof15prospectivecohortstudies.TheInternationalPerinatalHIVGroup.NEnglJMed.Apr1
1999340(13):97787.[Medline].
http://emedicine.medscape.com/article/1385488overview
9/10
6/8/2015
HIVinPregnancy
37. LouisJ,LandonMB,GersnoviezRJ,LevenoKJ,SpongCY,RouseDJ.Perioperativemorbidityand
mortalityamonghumanimmunodeficiencyvirusinfectedwomenundergoingcesareandelivery.Obstet
Gynecol.Aug2007110(2Pt1):38590.[Medline].
38. WiysongeCS,SheyM,KongnyuyEJ,SterneJA,BrocklehurstP.VitaminAsupplementationforreducing
theriskofmothertochildtransmissionofHIVinfection.CochraneDatabaseSystRev.Jan19
2011CD003648.[Medline].
39. FowlerMG,LampeMA,JamiesonDJ,KourtisAP,RogersMF.Reducingtheriskofmothertochildhuman
immunodeficiencyvirustransmission:pastsuccesses,currentprogressandchallenges,andfuture
directions.AmJObstetGynecol.Sep2007197(3Suppl):S39.[Medline].
MedscapeReference2011WebMD,LLC
http://emedicine.medscape.com/article/1385488overview
10/10
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Red Flags For Unhealthy RelationshipsDocument2 pagesRed Flags For Unhealthy Relationshipskepler8092% (13)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Open Response To The Confused SSPXDocument33 pagesOpen Response To The Confused SSPXgilbertnunesNo ratings yet
- BETA and Gamma Functions Hand Out UNIT - IIDocument3 pagesBETA and Gamma Functions Hand Out UNIT - IISanjana PulapaNo ratings yet
- Aerosols in AyurvedaDocument13 pagesAerosols in AyurvedaDr ajayNo ratings yet
- Gut-Brain AxisDocument33 pagesGut-Brain AxistioNo ratings yet
- Adolescent TuberculosisDocument29 pagesAdolescent TuberculosistioNo ratings yet
- 3 - Deteksi Dini CHF - 22.3.23Document53 pages3 - Deteksi Dini CHF - 22.3.23tioNo ratings yet
- 9 - Penanda Diagnostik Pada Gagal Jantung AnakDocument22 pages9 - Penanda Diagnostik Pada Gagal Jantung AnaktioNo ratings yet
- Susunan Acara Webinar PDFDocument1 pageSusunan Acara Webinar PDFtioNo ratings yet
- Acute Limb Compartment Syndrome: Observation ChartDocument2 pagesAcute Limb Compartment Syndrome: Observation CharttioNo ratings yet
- Cole Melanie BJM 2014 A Modified Early Obstetric Warning SystemDocument9 pagesCole Melanie BJM 2014 A Modified Early Obstetric Warning SystemtioNo ratings yet
- Pone 0217864Document15 pagesPone 0217864tioNo ratings yet
- EF Adults-English-Phrasal-Daily LifeDocument32 pagesEF Adults-English-Phrasal-Daily LifetioNo ratings yet
- NIH Public Access: Author ManuscriptDocument19 pagesNIH Public Access: Author ManuscripttioNo ratings yet
- Diagnostic Approach To Pleural Effusion in AdultsDocument20 pagesDiagnostic Approach To Pleural Effusion in AdultstioNo ratings yet
- Kaplan Focus ReviewDocument9 pagesKaplan Focus ReviewSaidel ElizondoNo ratings yet
- Tutorial 12 - Surface Temperature - QuestionsDocument3 pagesTutorial 12 - Surface Temperature - QuestionsAntonioNo ratings yet
- 20 FactsDocument62 pages20 FactsAlison_VicarNo ratings yet
- Chapter 1 Developmental Disorders of The Oral CavityDocument6 pagesChapter 1 Developmental Disorders of The Oral CavityArafat Masud NiloyNo ratings yet
- Student Support Material Class XII PhysicsDocument291 pagesStudent Support Material Class XII PhysicsHemanshi KocharNo ratings yet
- Trouble Shooting of Motor ElectricalDocument32 pagesTrouble Shooting of Motor ElectricalCharles100% (1)
- National Rural Development Programme 2007 - 2013 - June 2010Document832 pagesNational Rural Development Programme 2007 - 2013 - June 2010alexia_s_mNo ratings yet
- Considerations When Using Charging Current Compensation in Line Current Differential ApplicationsDocument12 pagesConsiderations When Using Charging Current Compensation in Line Current Differential ApplicationsJeferson HrnNo ratings yet
- Technical Definitions: 10 To 1000 kVA - 50 HZ / 12.5 To 1250 kVA - 60 HZDocument1 pageTechnical Definitions: 10 To 1000 kVA - 50 HZ / 12.5 To 1250 kVA - 60 HZJean Luc FrancisNo ratings yet
- Paper: IBM System Storage DS3950 IntroductionDocument18 pagesPaper: IBM System Storage DS3950 IntroductionTerence MuripoNo ratings yet
- Appendix A - WMT Berthing and Mooring AnalysisDocument75 pagesAppendix A - WMT Berthing and Mooring AnalysisKarim OuNo ratings yet
- Geology AssignmentDocument9 pagesGeology Assignmentgrace azasNo ratings yet
- LTE DL Power AllocationDocument3 pagesLTE DL Power Allocationdeepakbhl100% (1)
- Business Policy Chapter 7 SlidesDocument32 pagesBusiness Policy Chapter 7 SlidesAsadChishtiNo ratings yet
- Environmental Assessment, Old York RoadDocument208 pagesEnvironmental Assessment, Old York RoadThe Elmhurst TitanNo ratings yet
- The Pros and Cons of Parents' Educational Expectations To The Academic Achievements of Junior High School StudentsDocument198 pagesThe Pros and Cons of Parents' Educational Expectations To The Academic Achievements of Junior High School Studentsyannah kristineNo ratings yet
- Long Term Internship BComCA) - VI Sem 2023-24 (1) - 1Document11 pagesLong Term Internship BComCA) - VI Sem 2023-24 (1) - 1maheswarilokku5No ratings yet
- JBL - Sistema de Configuracion VERTECDocument19 pagesJBL - Sistema de Configuracion VERTECErling SanchezNo ratings yet
- MathChE MATLAB ODE Part1Document16 pagesMathChE MATLAB ODE Part1Arm CharoenkoolNo ratings yet
- Gpa & Cgpa CalculatorDocument7 pagesGpa & Cgpa CalculatorQaisKhanNo ratings yet
- 2008-Indo-European Languages Tree by Levenshtein DistanceDocument8 pages2008-Indo-European Languages Tree by Levenshtein DistanceDaniel FonnesuNo ratings yet
- HP Deskjet Printers - Printing Internal TestsDocument3 pagesHP Deskjet Printers - Printing Internal Testserick_ssNo ratings yet
- TCD6 20110408 19 - 44Document316 pagesTCD6 20110408 19 - 44Midhun Pillai (P&M)No ratings yet
- RMM 27 FINAL - CompressedDocument105 pagesRMM 27 FINAL - Compressedbrada12350% (2)
- Aluminium - Handling, Storage, Maintenance and CleaningDocument7 pagesAluminium - Handling, Storage, Maintenance and CleaningKiran KarthikNo ratings yet
- Educational Research Quantitative Qualitative and Mixed Approaches 6th Edition Johnson Solutions ManualDocument35 pagesEducational Research Quantitative Qualitative and Mixed Approaches 6th Edition Johnson Solutions Manualstrunttriose1xjj100% (21)