Professional Documents
Culture Documents
IMLE Flash Cards Almosadoctor
Uploaded by
tchanoch100%(1)100% found this document useful (1 vote)
119 views33 pagesOriginal Title
IMLE Flash Cards Almosadoctor(1)
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
100%(1)100% found this document useful (1 vote)
119 views33 pagesIMLE Flash Cards Almosadoctor
Uploaded by
tchanochCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 33
r
A
S+S
Atrial Fibrillation
Heart causes: IHD, HTN, Mi, Mitralvalve
disease, Heart failure
-Lung causes: PE, pneumonia
*Other- alcohol, thyrotoxicosis, JK, *Mg.
~5%6 of aver 65's, 10% of over 70's
~15% of stroke patients
Palpitations soaithough the ventricles contract,
irregularly irregular pulse sufficient blood pumping to produce a
*Pulse deficit: HR>radial pulse — pulse does not occur.
ventricular filling does not always occur, «Rarely: chest pain, dyspnoea
=P Atrial rate(300-600bpm). This cannot be conducted through the AV node, thus conduction
tothe ventricles is variable, hence the irregularly irregular pulse at 75-190bpm
-Cardiac output isreduced, and there is stasis of blood leading to an increasedrisk of stroke
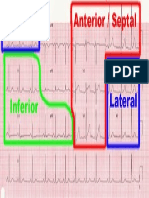
ECG!
*No discernable P waves
Irregular ORS
*Normal shape QRS and T
Acute AF - <48hr duration :
“Control rate (see chronic AF)
-Give heparin to prevent thrambus (Cl for CV)
«Try mechanical cardioversion (70% success}:
“ITU, with 02, with anaesthetist + sedation
+1001, 2001, 3601, 360)
*Medical cardioversion (less successful) =
“Amiodarone
*Flecanide - 2" line
debate
‘Bloods
*TFT’s—for hyperthyroidism
*Cardiac enzymes —for Ml
“Chronic AF - >48hr — Ryhthmn control
+B-blocker OR Ca2+ antagonist
+Add digoxin if ineffective
+Anticoagulate - dependent on
CHADS2 score (usually WARFARIN)
Paroxysmal AF — occasional spetis of AF
Pill in the pocket” ~ taken when
symptoms occur (e.g. Palpitations). 8-
blocker (elderly) OR Ca2+ antagonist (if
‘uuere);. Oteunin 2 Gre:
Rheumatic Fever
‘*More commonly found in developing countries.
“Due to cross-sensitivity reaction to group A B-haemolytic strep.
*Develop 2-3 weeks after a strep URTI Cardiac failure
“Fever *Subcutaneousnodules,
“Chest! ‘Migratory polyarthritis
eb Pericardial rub Erythema marginatum
“Pericardial effusion *Chorea
sHeartMurmur, depends on valve affected,
+ Exact pathogenesis not known
*Qedems and fibrinoid necrosis of collagen
“Aggregations of lymphocytes and macrophages > Aschoff's bodies
-Aschoffsbodies form MacCallum’s plaques.
“Diagnose with Jones criteria, either 2 major, or 1 major + 2 minor + evidence of strep infection
Major criteria = Carditis, Polyarthritis, Erythema marginatum, Subcut Nodes, Chores:
Minor criteria= Fever, SESR/CRP, Arthralgia, PR interval on ECG, +ve history.
‘Throat Swabs, ECG and echoneeded.
“Bed rest
=Procaine benzylpenicillin O.6megaunits IM daily for 8 days.
‘Aspirin at high doses (100m@/kg/day. Max 6-8¢/day for 2/52 > GOme/ke/day for 6/52
*Prednisolone 1-2mg/kg/day can be given if severe, tapered after 2/52
“Treat choreaif occurs.
if at high risk, or have 3 past history of rheumatic fever > Prophylaxis
Benzathine penicillin 1.2 megaunits, IM every3/52, or daily phenoxymethyipenecillin 250mg PC
Varicose Veins
*Affect 40% men and 32% of women but Higher proportion of women present.
Risk factors > Age, 1 No. Of Pregnancies, Pregnancy, Long periods of standing,
ve Family History.
sAppearance of Veins *Restless Leg syndrome
els “Heavy Legs
Aching *Cramping (worse at night}
*Hot/Burning Feeling
=Primary Varicose Veins — Weak vein walls -> Dilated veins > Valve cusps can'tmeet
> Valve incompetence.
“Secondary Varicose Veins — Pelvic or abdominal masses > Venous return obstructed.
Complications = Due to veins themselves > Bleeding, Thrombophlebitis
Due to venous hypertension > Oedems, Venous Ulceration, Varicose Eczema,
Pigmentation changes, Lipodermatosclerosis.
Good History and Examination
“Cough impulse (Fluid Thrill felt over incompetent vein on coughing)
“Trendelenburg Test > Use Tourniquet and position of ptto determine level of incompetent vein
Jour Doppler Venous Scans
“Often not needed >Reassure pt.
“Supportive (e.g compression stockings for oedema)
“Traditional surgery > Ligation and stripping (removal of affending veinand tying valve)
*Endovenous Laser Therapy (EVLT) > Catheter placed in leg and laser causes vein ablation.
+Radiofrequency Ablation (RFA) > Catheter placed in leg and alternating currentablates vein.
*Scerotherapy > Injection of sclerosant (commonly in @ faam) which promotes vein spasm.
#ineereer ull coreery lec Colmeicaitbien ‘wid Chere ere Tach relesce raed:
Chronic Asthma
‘Asthma is Extrinsic (External Cause) or intrinsic (no cause found)
Extrinsic > Atopy, genetic links
Environmental fectors > e.g. hygiene hypothesis
+808. Triggers for Asthma Attack
Wheezing. aun Exercise
-(nocturnal) productive cough. *smoke *Emotions
ap + Peak Flow (with dinural variation). Cold air
sffnerison's Sulci sallergens (dust/pet hair ete)
cHyperinflatedchest. “School Absence *Chemical irritants
sOthersigns of Atopy. “Exercise Tolerance
‘Hypersensitivity + Trigger factors (see list) = inflammation, Oedema, Bronchoconstriction and
“individual with genetic predisposition + Environmental factors = Bronchial hypersensitivity.
mucosal secretions.
Over time remodelling of the airway occurs= goblet cells, smooth muscle, thick membranes.
*Spirometry (with trial of treatment)
*Peakflow (peak flow diary)
*Exercise tests
*Skin Prick Tests
sChestX-ray (to rule out other causes)
*Step 1- Short acting B2-agonists (e.g salbutamol PRN}
Patient and family education. *Step 2- Add inhaled Steroid (e.g Beclomethasone)
Lifestyle advice (avoid triggers.) *Step 3 - Addlong acting B2-agonists (eg Salmetreol) or
“Medicaltreatment 3-335 99-9 *Step 4— Addin other agent (e.g montelukast)
Regular reviews, inhaler technique.
*Step 5 - Referto respiratory paediatrician
= Add in daily oral steroids:
Crohn’s Disease
“Genetics — (CARD-15 and NOD-2 genes)
“Environmental factors Smoking, Previous appendectomy
simmune response = Autoimmune, abnormal T cell response
*Relapsing-remitting symptoms +Anal Fissures Mouth Uicers
“Diarrhoea—(Pus, Mucous and blood) «Low grade fever, malaise “Arthritis
S S “Constipation — if strieture/obstruction andlethargy *Ureitis:
eb “Pain= ‘Cramp like’, not relievedon «Flatulence “Erythema nodosum
defecation, often in RIF. “Bloating Osteoporosis
“Weightloss - due to L appetite *Stunted Growth/Delayed *?Miscarriages
“Nutritional deficiencies Development *KidneyStones
“Anaemia “Clubbing Skin Tags.
‘Lesions can affect anywhere in Gi tract, from mouth to anus. They are therefore called skip
lesionsas there are areas of healthy gut between diseased areas.
sThe characteristic areas have transmural ulceration with granulomatic changes, giving &
cobblestone appearance, the gut lumen will narrow, giving strictures, and may cause obstruction.
The lesions may fissure, giving perforation or fistula formation.
\ Blood tests (FBC, CRP and ESR, LFT, U+E, iron and 812)
“Stool samples should be taken
“Barium swallow/bari
eae ener toexciude infective diarrhoea.
*Endoscopy/colonoscopy to see and biopsy lesions
“CT/MAl to see structure of gut and checkfor abscesses Bistro!
*Lifestyle changes! (Smoking, diet etc) *Surgery—Last resort, but 80% will
“Treat the acute, maintain the remission” need some!
‘Acute > Mild =Prednisolone ~Resect affected areas.
‘DSevere = Admit, TPN, Metranidazole -NOT CURATIVE
*Remission > Azathiprine, Methotrexate, infliximab
Hyperthyroidism
Ss a Ss + Symptoms - agitation, “eeling hot”, | Signs— AF/ arythmia, sinus tachy, fine tremor, gotre
“Thyroid Eye Disease — only GD - dry/aritty eyes, lia
retraction, lid lag, proptosis, oedema, optic nerve “Thyrotoxic storm - fever, diarrhoea, vomiting,
compression (can cause blindness)
*M:F— 1:5. prevalence 2-2% women
65% of cases due to Graves Disease (GD)- age of onset-20-00
35%6of cases due to toxic multinoduoar thyroid (TMIT}-age of onset—elderly women
palpitations, weight / 7 apetitie, | (GO=ciffuse, TMT=nodutar),paimar eythema, moist palms,
diarrhoea, menorrhagia, aligamenorrhoes | proximal weakness, gynaecomastia, pretibial myxoedema
(GD), increased reflexes with delayed retaxation.
seizures. 30% chance of death. Often with precipitant
P
*GD-production of TSH receptor stimuating ABs. Genetic predisposition and environmental factors (7E.
Coli). TMT - strong environmental association: high iodine intake (e.g. Dietary, or from drugs - amiodarone
*Comptications - osteoporosis, slight “Prisk of death in first 12 months (AF)
sBloods—TF1’s -TSH(-)4T3(4). T4 also raised, but T3 more sensitive in hyperthyroid. Test T4
andTSH if suspect hypothyroid.
*B-blockers - giveto all patients to reduce symptoms whilst other treatments take time (typically
2-3weeks due to long HL of T4) to have effect. Then, Several Options:
-Medical- Carbimazole - titrate dose until clinically euthyroid. Then, dose can be reduced over
period of 6-24 months. Can cause immunosuppression — particularlya neutropaenia.
*Blockand replace - high dose of carbimazole, then give throxine to replace endogenous
“incase of SEs alternative thiourelenes are available.
*Radioiodine -*41is given. Taken up into thyroid and destroys thyroid tissue.
-Surgical- thyroidectomy. Sometimes parathyroid glands are accidentally also removed, and thus
calcium levels should be monitored after surgery.
+Problems with treatment — many patients become hypothyroid. Life-long monitoring is often
required. NB — controlling hyperthyroidism in GD does not reduce development/risk of eye
complications. if patient become hypothyroid, even greater risk of eye complications
b)
a AO
“Migraine itself:70% without sure, 30% with sure
*Precipitants: chocolate, oro! contaceptives, cheese,
coffeine, alcohol exercise, troumo
sincidence 8-12%of the population
*Responsible for 30% of head-aches
Soe Associated with periods of rest (e.g. Occur at weekends)
“Unilateral head-ache *No neurological signs
*Often precede byaura — typically *Heightened pain perception and
ap visual, but may be sensory, speech sensitivity (e.g. To light)
orteste related eAssocisted with puberty, menarche,
*Episodes last 4 - 72 hours: pregnancy and menopause
*Due te alterations in cerebral bloodflow. Initial vasoconstriction may cause aura, then the
resultingwasodilation results in pain
*Clinical Diagnosis. Performa neurological exam to rule out other pathologies. May appesr similar
toTIA, but TIA will often have foeo! signs, sudden onset, and maximal symptoms at time of
onset. Tension headache tends to be bilateral, no aura, associated with stress / work.
*Diagnostic criteria - headaches lasting 4-72 hours with aura (clossicol migraine) OR headache
lasting 4-72 hours, no aura, with nausea or vomiting or photophobia, PLUS (2 of... unilateral,
intereferes with normal functioning, worsened with posture (e.g. Bending / walking), pulsating
*Acute management of pain: *Chronic Management: (f>2 attacks /month. 65%
‘Simpleanoigesia-parscetomol,espirn of patients will have a 50% reduction in attacks
*SHT agonists ~ Triptans— e.g, Sumatriptan *Pizotifen - antihistamine and SHT
*Rebreathing into = p=perbaghasbeen ie
ihyoo be Ree DIS pce antagonist — causes vasoconstriction
blood co2 *Beta-bockers — e.g. Propanclal
samytriptyline
b)
Wo
Parkinson’s Disease
Unknown! Thought to be a mix between genetic predisposition (a-synuclein + Parkin genes)
and environmental factors such as exogenous toxins.
S+S
sBradykinesia
“Tremor — “Pill-rolling” , typically but not exclusively in hands, J on movement.
Rigidity — Both Lead-Pipe and cogwheel, 7) on movement of opposite limb.
*Bradykinesia— Difficulty in starting, stopping and changing direction.
~ sbfacial expressions
-Posture—Stopped, with shuffling gait “Constipation
‘+ handwriting size and legibility. “Depression
‘Tremor “Rigidity. *Brisk Reflexes Dementia
=Degeneration of dopinergic neurons in substantia nigra of midbrain.
‘Eosinophilic inclusions called Lewy Bodies are found in affected areas.
Some changes of non-dopinergicneurones-> Why I-dopa doesn't affect all symptoms.
“Lab tests not particularly useful
“Headimaging is usually done. (MAI or CT).
Pharmacological Treatment > L-dopa is the mainstay, other drugs are usedto postpone it's use
+ L-Dopa > Replaces dopamine levels. Given with peripheral decarboxylase (eg Madopar) tc
ensure all dopamine goes to the brain. | effect over time so left as late as possible
*Dopamine agonists e.g Peroglide > Directly stimulate dopamine receptors.
*Anticholinergic agents > J tremor but lats of Side effects (CVS!)
*Selegline > | Breakdown of Dopamine
‘Surgery > Rare though ‘in use. Deep brain stimulation using electrodes in subthalamic region.
T “MOTI! > OT, Physio, SALT and psychiatric input vital to symptoms and 1 Quality of Life!!
e Myasthenia Gravis
"A Exact cause unknown, though there is thought to be a strong genetic link.
*Prevalence is 1/200000, and is most commonly seenin younger women and older men.
cat risk if Family history of autoimmune diseases, or if patient has any (e.g SLE, RA etc)
Myasthenia Gravis has a relapsing/remitting course.
ef the morning/after a rest.
+Weaknessof muscles > Ptosis, Diplobia, Dysphagia, Dysarthria, Dysphonia
Weak facial muscles, Weak Shoulders/thighs,
Weak neck/trunk muscles, weak Respiratory muscles
*Limb Reflexes -> Normal or Brisk
*Muscle wasting > Onlyin severe/ Prolonged disease
P ‘IgG autoantibodies produced against the Postsynaptic acetylcholine receptorsin
neuromuscular junctions.
disease of the thymus (75% get hyperplasia of thymus, 10% get a thymoma)
“Blood Tests -> Serum acetylcholine receptor antibodies and other autoantibodies.
i “Tensilon Test > injection of Edrophionium and Atropine > Sudden symptomatic improvement
Associ
‘*Electromyography > Fatigue following repeated electrical stimulation of muscle.
+ ‘litter’ found on Single Fibre Electrode
“Thymus imaging > To checkfor hyperplasia.
‘*Spirometry > To monitor respiratory muscles.
T ‘*Oralacetyicholinesterase inhibitors (e.g Pyridostigmine) to | breakdown of acetylcholine
‘“Immunosupression > Corticosteroids usually, but steroid sparing agents can be used.
~Immunomodulatory agents
acute crises IV immunoglobulin or Plasmapheresis used
Wiheeecione.
Lymphoma
*Thought to be secondary to EBV infection «More common in developed countries
“MF 1S21 *Rare (incidence 3 per 100 000)
*Peak incidence: 20's and 50-70's
*Cervical lymphadenopathy (70%)— Vague symptoms:
rubbery, painless, may *Pruntts {itch}, Fotigue, Anorexia
Spontaneously remit +Alcohol induced pain ot lymph nodes
ap +Ivediastinal widening (CXR) *B Symptoms indicate worse prognosis
*Splenomegaly Fever, night sweats, weight loss >10%
+Other lymphadenopathy
*Defectwith 8 cell maturation in lymph nodes. 8 cells stop expressing correctsurface
antigens, and are unable to fight infection. Reed-Sternberg cells are 3 classical feature — these
are essentially deformed multi nucleated 8 cells. Pathogenic process includes:
+Resistance to oveptesis, self-regulation, enviranmental factors (EBV), genetic factors
“FBC - narmocytic nonmochramic anaemia, high esoinophils, low lymphocytes
+ESR— raised “PLDH-Ioctote dehydrogenase — poor prognostic indicator
*CXR—mediastinol widening _CT scan - involvement of intrathoracic Iymoh nodes
+Lymph node biopsy - DIAGNOSTIC - Reed-Sternberg cells
b)
*Disease staged liv Ana-Arbor Classification. Stages | + I = mild, stege lll +IV = severe
+ 5yr Survival — varies, but Stage I— 95%, Stage IV— 40%
*Mild — Radiotheropy + Chemotherapy. Chemo if more severe. Cure rate ~B5%
*Severe~ Chemotherapy + Radiation to bulky areas. Cure rate ~60%. 15yr survival =65%
*Common chemo- AVBD Adriamycin, Bleomycin, Vinblastine, Decarbazine
“initial SE's (chemo); nauseo + vomiting, hairloss, myelosuppression (1% mortality}, neuropathy
*Long term Sé’s (chemo + radio): “risk of: lung cancer, infertility, cordiac abnormalities,
breast cancer
a AO
Rheumatoid Arthritis
* Autoimmune disorder Onset usually in young adults
*M-Fis 12: increased risk in: Smokers, stress, infection
-Genetic Component -Symptoms often worse in hot weather
Symmetrical inflammatory arthropathy, causing DEFORMITY, typically affecting the small
Joints of the hands and feet (but also knees, hips and elbows).
=Pain and stiffness worse in morning (*20mins)
4p ‘Characteristic hand signs: 2-thumbs, butonniere’s, swan-necking, uinor deviation, muscle
wasting, subluxation of MOP, sometimes carpal tunnel syndrome, anlanto-axiat subluxation
*Decreased hand function (knife and fork, doing up buttons), and nodules are common
+Extra-articular features; Sjogren’ds syndrome, Reynauds, vasculitis, Nodufes (firm but
usually painless
*Auto-antibody production (70% IgM, 30% IgG) against joint tissues
*DEFOMITY is the key characteristic clinical sign
*Bloods: Rheumatoid factor is not diagnostic. Present in 70%, but also in general
population. Rheumatoid positive disease has worse prognosis and more extensive
deformity. Anti-CCP antibodies test similar to rheumatoid factor. “ESR+4SCRP,
normochromic-nonmocyticanaemia common
X-ray: ia, deformity,
Sire Pecuce Tone cera efor LaF. Raereel ihc rean’sion; betlare SP'stone term
“DMARDs are mainstay. All can cause myelosuppression and rash plus: Sulfosaizine: hepatic
impairment, oligospermia, methotrexate; Gldisturbance (give folic acid to reduce), mouth ulcers,
hepatic impairment gold; medical emergency rash, photosensitivity, nephrotic syndrome;
leflunomide, chloroquine: retinitis, tinitus, infliximab ; anti TNF-a agent: can cause reactivation of
ime tccaecs te o Feb
SLE
F= 1:10 “Strong genetic component
Autoimmune connective tissue disorder Asians thanCaucasians
-More common in BlackAfricans and Indian -Onset at any age, peaks at 25-25 and 50-60
Photosensitive (often malar) rash _not cause lass of function
-Non-specific symptoms; malaise, «Splinter hemorrhage and nail infarcts
fatigue, weightloss, alopecia, mouth + Renalimpariment
ulcers +Haemaotlogical dysfunction;
-Arthritis—a symmetrical polyarthritis, leucopaenia and lymphoma, as well as
usually affecting the small joints, haemolytic anaemia
similarto RA. Unlike RA, changes do _+Neurological signs (e.g. Seizure)
+Resultsin the production of ANA (anti-nuclear antibodies). These are highly
sensitive, but not specific (can be due to. RA, medications (e.g. anti-TNFs))
Pp “Basically unknown, but thought toe autoimmune
Complications: Trisk of athersclerotic disease, infection, thrombosis
+Bloods — ESR + CRP, anaemia, thrombocytopaenia, lymphopaenia, leucopenia
*ANA-testing
| “Urine dipstick — for renal impairment -red cell casts, and proteinuria
-Anti-doublestranded-DNA—highly specific, but only present in 60% of cases
*Mild cases can be managed with NSAIDs and lifestyle changes (eg. Avoid sunlight)
*Moderate to severe: treatment similar to RA; steroids to induce remission, long-term use:
“DMARDs: All can cause myelosuppression and rash plus: Suifasalzine: hepatic impairment,
oligospermia, methotrexate; Gl disturbance (give folic acid to reduce), mouth ulcers, hepatic
impairment gold; photosensitivity, nephrotic syndrome; leflunomide, chloroquine: retinitis, tinitus,
(eles ¢ Grae TAF rest: cn tative cents ten uk steric ceases te 108
Scleroderma
oMGF= 1:4
Autoimmune connective tissue disorder «Smoking increases risk
-Onset at any age, peak 30-50
~CREST- C—Calcinasis calcium deposits, usually in fingers, R— Reynaud’, E—
Esophageal dymotility causing GORD, S—Sclerodactyly, T— Telangectasia
“Other signs — hypopigmentation (occasionally hyper-), ulceration, necrosis and
oP gangrene of affected tissue — usually hands and feet, Sjogren's syndrome (dry
eyes+ mauth), mouth ulcers, polyarthropathy
+Organ involvement — can affect any organ, but most commonly kidneys, Git,
heart and iungs
*Organ damage usually due to fibrosis, secondary to vascular pathology
+Renaland pulmonary complications are life threatening
Pp *Autoimmune disorder, resulting in vascular damage.
“There maybe periods, lasting from weeks to months, of apparent symptom regression
*Anti-centromere antibodies — in 40% of cases — associated with the milder limited!
cutaneous scleraderma- LCS
-Anti-Sclantibodies — in 70% of cases — associated with the more severe diffuse
cutaneous seleraderma- DCS
-Hardtotreat. Nospecifics for disease itself. Complications managed individually.
Immunosupressants may be used in severe flare-ups (e.g. IV cyclophosphamide)
+Renal impairment — ACE-inhibitors, Oesophageal - PP!'s, Pulmonary hypertension -
calcium channel blockers, annual spirometry monitoring Heart - annual ECG
*Prognosis - LCS—10yr »759%, DCS - 10yr-55%. Death usualy from tung/heart/ranal complications
Paget’s disease of the bone
sAffects5% of 55's. Rare under50 «Thought to bethe result of enviranmental factors
Slightly more commen in men (viral) in genetically susceptible individuals
*More common in pet owners
+3056 will have symptoms *Pathological fractures
*Bone pain *Usually unilateral, at one specific site
*Deafness— if the skull is affected Osteosarcoma (rare - “19% of cases)
the vestibulocochleor nerve con be
compressed
*Accelerated rate of bone turnover — osteoblasts are often enlarged and abnormal
Osteoclasts are abnormal but overactive.
*A chronic progressive disease
“Bloods Xray
*ALP—classically raised *Lytic and sclerotic lesions —lots of
*Gomma-GT —rule outliver couse of TALP dark blobs in the bone!
*Bone Scan — shows increased uptake in affected *Wideningof the bone cortex
bones sone deformities (often bones bent)
*Urine-often contains collagen due to high bone
reabsorption
“Based on symptom severity (¢.2. Poin, frocture, deformity / deafness}
sisphosphonates — e.g. Pomidronate - mainstay of treatment reduce osteoclast
activity - typical regimen ~2 months can induce remission
*Analgesio
sTreat complications (2.9. Joint replacement)
Osteoarthritis
A
*Canbe Primary (no known cause) or secondary (as 2 result of other pathology)
“Theres a genetic component (Collagen type ll genes!)
Risk factors = BMI, Hyperparathyroidism, Manual Labourers
Several different subsets giving different pictures.
cf *Nodal (hands), Hip, Knee, Primary generalised (Hands, knees, big toe, hip)
Erosive (hands)
“Pain > Ache/Burning, worse on movement, worse after inac
~Swellings, both fluid and bony e.g Heberden’s (OIP), and Bouchards (PiP)nodes
+loint stiffness sloint linetenderness +L range of movement
-Deformities (e.g Bow legs) Muscle wasting
‘pin cartilage so bone exposed =~
‘This gives T bone formation inside the bone = SCLEROSIS
sit also gives bone formation outside the bone = OSTEOPHYTES.
*Microfracturesin the new bone cause CYSTS to form.
“Theres also often an effusion due to the synovial membranes thickening due to damage
“Bloods -> Mainly to exclude septic/inflam/rheum arthritis
“X-Rays > Show 4.main changes.
DHloint space > Sdlerosis, > subchondral Cysts > Osteophytes
*Arthroscopy > Can look at the cartilage in the early stages
*No cure!
“Conservative -> Lifestyle advice (Weight loss!), Analgesics, NSAIDS (careful about ulcers!),
Physio, Steroid Injections, Glucosamine
*Surgical > Debride and washout (knees), Joint replacements, Joint fusion (small bones),
Joint excision (rare), Realignment surgery
Fractures (GENERAL)
“Pathological Bone — Metabolic Bone Disease(OSTEOPOROSIS) — -Tumours (mets!)
- Rheumatoid Arthritis - Infection
A -Happen with normal bone with a lot of force, or little/no force in Weak, pathological bone.
VARIES DEPENDING ON THE SITE OF THE FRACTURE, BUT THERE IS USUALLY
Pain “Visible Deformity
Unless pathological there is usually history of trauma *Crepitus may be present
-Usually a tender swelling over the site. *Signs of nervous insufficiency.
+Isthe fracture open (skin broken) or closed? *Signs of Vascular insufficiency.
Pp Different mechanisms of iniury give vou different fracture patterns.
ao cu ca op as
sTransverse Oblique “Spiral “Displaced -Angulated
a5 OD ce GP
impacted +Rotated ‘Distracted — Pathological =o rminuted
“X-ray — Minimum of 2 (AP and lateral) > Some fractures have special views, Joints need x-ray
“CT — Useful for assessing complicated fractures prior to surgery.
*MRI - Useful if fracture is hard to spot on x-ray, or in looking for Avascular Necrosis.
T
“ABC!
Reduction — Either open or clased
Fixation — Conservative (Casts, traction (rare) or Surgical (Wires, Internal/external fixation,
Intramedullary nails)
Mobilization - MDT + Physio, OT, Social workers
Endometriosis
“Genetic Link
+Retrograde Menstruation
*Sampson’s Theory (age with contraceptive/obstetric history)
‘May be some blood/lymph borne spread
“Can be asymatomatic “Symptoms of other sites
“Chronic Pelvic pain (cyclical) *cyelical haematuria.
*Dysmenorrhoea *blood in stools.
*Deep Dyspareunia *tHaemoptysis
*Subfertility *Ubililcal bleeding?
*Dyschezia (Pain on defecating) *On examination, Fixed, ?retroverted uterus
“May feel masses on abdo or pv exam.
*Presence of endometrial tissue outside of the uterus, normally on uterosacral ligaments,
ovaries pelvic wall.
“Tissue responds to cyclical hormones the same as uterine endometrial tissues.
*ifin ovaries, forms chocolate cysts, which if rupture give acute abdo pain and peritonitis.
* Because of the inflammation, fibrosis occurs and adhesions form, often fixing the pelvis.
“Bloods > Check for anaemia
j *Laparoscopy > Diagnosis by seeing active endometriosis or signs of previousendometriosis.
“Transvaginal ultrasound excludes cancersand may shaw cysts in the ovaries,
*MRI sean may be usefulto show undetected lesions.
‘sifasymptomatic then no treatment is needed. Analgesia for pain
‘Hormonal treatment > COCP, Progesterones, US, GnRH analogues
I “Surgical treatments > Laser/bipolar diathermy, dissection of adhesions, Hysterectomy
with bilateral salpingo- oophorectomy and HRT
*Fertilityhelp
Fibroids
A “Also known as leiomyomats, common benign tumours of myometrium.
“Enlargement due to oestrogens (sometimes progesterones too). As 8 result
growing after the menopause, but growth may be resumed by HRT.
Large variation in size, size change due to the hormonal cycle.
+*505% asymptomatic +Pressure effectsas fibroid grows, commonly
-Menorrhagia (typically iffibroid is Dysuria, hydronephrosis, constipation,
ee submucosal or polypoid) sciatica
Pain (rare unless torsion or *Subfertility
degeneration} *Abdominal/pelvic mass
0.1% may be malignant.
*if pedunclated, the fibroid can twist causing torsion, and acute pain.
Fibroids can also ‘degenerate’ due to \-bload supply, there is then pain,
hemorrhage and sepsis.
in Pregnancy, fibroids can give > Premature labour, malpresentation
1-submucosal
Ultrasound + lets you know if mass 2-Intracavity polyp
*MRI/laparoscopy > distinguish type (see picture) 22> 3-Subseruous
sHysteroscopy/hysteroscalpingogram if in cavity. 4-SubserousPolyp
5- Intramural
if asymptomatic and small > no treatment!
*Tranexamic acid, NSAIDS often used, but ineffective for fibroid induced menorrhagia
“GnRH agonists work by inducing menopause, but can only be given for 6/12 then
fibroids regrow.
“Surgery Hysteroscapic (if submucosal or polyps), hysterectomy, myomectomy,
thevine wrtere enkciaaion
Polycystic Ovarian Syndrome
Se Link
has also been implicated
insulin resistance (unproven, some think itis an effect, some think it’s a cause)
*Cushing’s Disease
*amenorrhoea *‘Cervical Secretions *Acanothosis Nigrans ,
*Oligomenorrhoea *Miscarriages patches of darker skin
*Acne *Onbimanual exam, lumpy ——_caused by “insulins
masses felt
“Signs of hyper/hypothyroidism
*Subfertilty “Signs of diabetes
ulin Resistance “Signs of CVS disease
sBither LH or ‘insulin gives Nandrogen production by the ovaries, and sometimes the
adrenals
“The androgens produced are then not converted into oestrogens as normal, so “tin free
blood androgens.
Hormone levels-> LH, €9/LFSH, Androgens, estrogens, ‘Prolactins,
> Thyroid function tests
sultrasound +laparoscopy > Multiple cysts on the ovaries (string of pearls)
*May need CT/MRI of adrenals with Dexamethasone suppression test
Lifestyle advice > Smoking cessation, Increase exercise, weight loss,
Treat associated conditions -> Diabetes, HTN, Hyperlipidsemia
‘Treat Hirsuitism (if wanted) > Local (shaving, plucking, bleaching), or systemic
(Cyproterone, Spirinolactone, Finasteride)
siftrying to conceive > 1* line, Metformin +Clomifine, 2" Line, Other Subfertility methods.
*For irregular bleeding > COCP
Cystic Fibrosis
A
Autosomal recessive condition. 1 in 25 are carriers(in UK) 1 in 2500 affected.
*Abnormal genes on Chromosome 7 which produce CFTR pratein, most
commonly defectis AFSOB
Failure to thrive +Maeconium ileus *H8emoptysis
-Malabsorption *Bronchiectasis ‘Productive cough
*Recurrent Chestinfections sHyperinflated Chest *CholesterolGallstones
infertility in males osigshorvhes *'Salty Taste’
-Pneumothorax (es) ‘Depression Nasal Polyps
jabetes School Absences
“CFTR = Cystic Fibrosis transmembrane regulator (Na/Cl pump)
sits absence gives T viscosity of secretions
soeffects on inflammatory pracessesand the immune response.
“infertility in males is due to absent vas deferens
Sweat test > sweating induced by pilocarpine iontophoresis, sweat collected, +ve if NaCl
concentration 60<, high false +ve and false ~ve rates
“Guthrie test as neonate. *Bloods (FBC, LFT, U+€, Malabsorption screen, glucose)
*Genetic screening. “CXR
*Sputum culture
+ life expectancy! ‘*Abx (?Prophylaxis, may need *Diet= Tcalorie protein {fat
*MOTII! centralvenous catheter). *Creon (pancreatic enzymes)
*Anqual reviewin tertiary “Regular nebs (saline) with meals
centres Counselling “Vitamin supplements
*PhysiotherapyBD Genetherapy (verynew) ——_+Lung/Liver transplantation
Croup
A “Usually caused by viral infection -> Parainfluenza, RSV, rarelymeasels.
Starts with Coryzal symptoms Signs of severe infection=
Gets a hoarse voice <1 Respiratory rate
Barking cough =P Restlessness
<5 Harsh Stridor, often described Fatigue
asrasping, may reduce as 02 Sats <95%
infection progresses. “Soft Stridor
inflammation around the subgiottic area.
*Mucosalinflammation and oedema which extends to larynx, with significant
sIncreased secretions
“Donot look in the throat, as this may precipitate total airway obstruction!
‘Monitor their O2 sats.
“Most cases can be managed at home, with parents advised about the warning signs of
severe infection
‘Some people use warm, moist air, but its clinical effects unproven
+Prednisolne 1-2mg/kg PO Stat dose or Dexamethasone 0.15me/kg Po Stat dose
“May need nebulised adrenaline for severe infection.
if not improving then will need to be transferredto ICU and may need expertintubation.
Epiglottitis
A “Usually as a result of Haemophilus influenzae Type 5 (Hi5)
*Sudden Onset
+P temperature
silllooking child, sitting up straight, mouth open, drooling,
<5 “Soft Stridor and “respiratory effort, getting worse over minutes
*Child wont speak or swallow fluids
Rising Sun Sign > Often present but don’t look for it-> Angry redepiglattis
visible above tongue.
Pp “Infection > Inflammation and oedema of the epigicttis.
> Septicaemia may also be present
[ “initially treatment is far more important than investigations, as minutes count.
+MedicalEmergency, minutes do count. Transferte ICU or specialist anaesthetic room.
*Don'tlie the child down or examine the *GA, and intubate carefully, can be extubated in 24h
throat. ‘if intubation not possible, tracheostomy is needed
*Call for help > Senior Paediatrician, *Then take bloods for culture
ENT surgeons and Anaesthetists. "IV antibiotics (Cefotaxime 2mg/kg/6h).
*Rifampicin prophylaxis to household contacts.
Croup
A “Usually caused by viral infection > Parainfluenza, RSV, rarelymeasels.
“Starts with Coryzal symptoms Signs of severe infectior
*Gets a hoarse voice ‘+ Respiratory rate
= see
S46 Slee SS
a ES
or =o
inflammation around the subglottic aret
‘increased secretions
Pp “=Mucosal inflammation and oedema which extends to larynx, with significant
‘*Donot look in the throat, as this may precipitate total airway obstruction!
j “Montortheir Or sats
“Most cases can be managed at home, with parents advised about the warning signs of
severe infection
*Some people use warm, moist air, but ts clinical effects unproven.
Prednisolne 1-2mg/kg PO Stat dose or Dexamethasone 0.1Smg/kg Po Stat dose
*May need nebulised adrenaline for severe infection
‘if not improving then will need to be transferred to ICU and may need expertintubation
Epiglottitis
f\ ‘Usually as a result of Haemophilus influenzae Type 8 (HiB)
Sudden Onset
+Ptemperature
«illlooking child, sitting up straight, mouth open, drooling
“Soft Stridor and ‘respiratory effort, getting worse over minutes
“Child wont speak or swallow fluids
“Rising Sun Sign > Often present but don't look for it > Angry red epiglottis
visible above tongue.
‘infection > Inflammation and oedems of the epiglottis.
> Septicaemia may also be present
| “Initially treatment is far more important than investigations, as minutes count.
‘Medical Emergency, minutes do count. “Transfer to ICU or specialist anaesthetic room.
*Don'tlie the child down or examine the *GA, and intubate carefully, can be extubated in 24h
throat. “ifintubation not possible, tracheostomy is needed.
“Callfor help > Senior Paediatricians, «Then take bloods forculture.
ENT surgeons and Anaesthetists. IV antibiotics (Cefotaxime 2m@/kg/6h).
“Rifempicin prophylaxis to household contacts.
Re Neonatal Jaundice
*Before 24h = Usually either -Prolonged Jaundice ~
Sepsis or Blood diseases Pe ee Poe Breastfeeding jaundice,
eciece apo commonly Physiological ere
incompatibility or HS Or Breesfending thyroid problems (hypo),
(Hereditary spherocytosisy —_‘#undice cr
*Jaundiced! Skin and scleraare orange! *Signs of Kernicterus (Bilirubin >350umol/L)
ap -Signs of underlying disease ~Lethargic —- Poor feeding
S Biliary Atresia=Pale stools - muscle tone -Fits
-Rhesus— Splenomegally. = Coma = Death!
“Jaundice in general = bilirubin (breakdown of haemoglobin) in blood.
*Physiological Jaundice= Fetal Hb has short life span, and the neonatal liver often has difficulty in
metabolising it all. Fetal Jaundice happens in around about 60% of babies, so is very common.
*Breastfeeding Jaundice = Breastfed babes more likely to be jaundiced for longer. Multifactoral.
+Kernicterus = bilirubin levels cause bilirubin to crass 888 and deposit in basal ganglia and
brainstem. This can give long lasting neurological damage, but with good treatment this is avoided.
*Good history and examination
*Bloods (Bilirubin, FBC, LFT, Blood groups, Blood film, blood culture - TORCH SCREEN, Coombs test
[=
if persistent jaundice, consider USS of biliary tree.
“Each centre has its own treatment chart, which look like this >>>
*Supportive therapy (hydration status etc), if breastfeeding, keepdoing sol 3 | _-Transfusionline.
‘Phototherapy- 450nm wavelength light converts unconjugated bilirubin £ |“ —Photatherspy_
toa harmless substance, baby must be completely naked but wear eve p
Protection.Can be done via fibre-optic blanket. 7
Time
“Transfusion Either done through UVC or peripheral vein and arterial line.
‘fier ieuinien turer! erdnsme wok tarenuiabeurren ined tained te trmndhsane
A
Pyloric Stenosis
*More common in boys.
Genetic link, (strongly maternal)
*Presentsin first 2 months of life. *Epigastric/LUQ mass (olive mass)
*Projectile Vomiting of stomach “Visible Peristalsis
contents (no bile, soon after feeds. *Hypochloraemicalkalosis
*Very hungry baby, even after being *|- serum potassium
fed Dehydration
+ Dweight/weight gain Constipation
*Hyperplasiaand hypertrophy of the circular and longitudinal muscle layers in pylorus.
“This leads to narrowing of pyloric lumen.
“Good history and examination.
«if dehydrated, rehydrate before investigating
“Bloods (FBC, glucose, U+E,).
sABG .
“Test feed.
Ultrasound,
“Barium meal (rare) will show ‘shoulder sign’.
“Treat any fluid balance
sinsert Nasogastric tube
*Ramstedt's Pyloromyotomy
~ muscle is cut but not mucosa
~can be done open (RUG transverse incision), laprascopically, or umbilically
*Medical treatment with atropine sulphate showing promising results.
‘Triple Risk Model - High Risk Infant + Environmental factors + Physiological Changes
“Risk Factors = Age (1-6m) *Low socioeconomic group
Preterm *Single Parents
*Boys>Girls *Smoking in household
*Multiple Births *Co-sleeping
“Family History “winter
Maternal age (++ if mum <20) “Baby sleepson frontor side
255
“Overheating
“Unfortunately only
lp “The sudden and unexpected death of a child under 1 for which no
te couse is. tl mortem and case
sn/a
Autopsy s a legal requirement, despite how distressing it must be for the family.
*Do bloods, LP, Urine and stool cultures
Samples of infants clothing/bedding might be tested.
“PREVENT! BACK TO SLEEP CAMPAIGN!
| *Thoroughhistory
*Reassure family its no ones fault
ee “Be aware of Non-accidental injury
"Notify relevant people “Advice about the grieving process
Dash ieresigstions sifwented, suppress lactation (Cabergoline)
“Put family on Care of next infant scheme (CONI)
FBC
wec— 4-411x10°/L
Neutrophils 2-7.5x107/L (40-7556 WCC)
Eosinophils 0.04-0.44x10/L_ (1-6%Wwec)
Lymphocytes 1.3-3.5 x108/L (20-4556 WCC)
Monocytes 0.2-0.8x10°/L (2-10% wc)
Basophils 0.0-0.1x10°/L (0-1%wec)
Platelets — 15 -400x102/L
HB- Men: >13.02/dl
Women: >12.0e/dl
Reticulocytes 25-100x10°/L
MCV 80-96 fl
ct 25-35
Ferrit 12-300,
Clotting
Pr 11.5-15.5sece
APT 30-40secs
7 25.35
Biochemistry
Urea 2.5-6.7 mmol/L
cr Men 68-150 mol/L
Women 68-98 mol/L
Nat 135-145 mmol/L
ra 3.5-5 mmol/L
cit 2.05-2.6 mmol/L
Me 0.75-1.05 mmol/L
ck (24-195 U/L
LH 10-250 U/L
Amylase 60-180 U/L
Lactate 0.6-1.8 mmol/L
Urate 0.23-0.46 mmol/L
Inflammatory Markers
ESR Men 10 ng/ml
Fats
Cholesterol >5.2 mmol/L
Triglycerides 0.45-1.69 mmol/L
LoL <3.36 mmol/L.
HOL >1.55 mmol/L
Total /HDL 55
Diabetes
Random Gluc <1. mmol/L
Fasting Gluc <6 mmol/L
HbA. 3.8-6.4%
CSF
Protein <0.45¢/L
Glucose 2.5-4.4 mmol/L (~2/3 of plasma
level)
Cells <5 WCC/ml
Pressure 50-180 mmiig
Urology
PSA <6 nmol/L Age dependent—
‘older Men may have high level but no disease
Urine Levels
Creatinine 500-200mg/day
Usually higher in Men due to
greater muscle mass
Urea
BC's nil-3 /HPF
weC's nil-2 /HPF
Glucose nil
Nitrites wil
pH 57
Protein nil trace)
Ketones nil
Hyperkalemia- Tall peaked Twave, Widen QRS
complex, prlong PR interval, Flat P wave
Hypokalemia- Flat or inverted T wave, Appearence of
U wave, Depressed T wave
Hypocalcemia- Prolong ST&QT intervals
Hypercalcemia- Short ST, Wide T,
Hypermagnesemia- Prlong PR interval, widen QRS
complex
Hypomagnesemia- Tall T wave, Depressed ST
segment
es :
tee = Newupon = 301 pom
aan oman pees iS 2 Sie
co im |r fae = ine Seen
Sime te |e tary teem ieee: atts
= ire ‘one = Vipers 2 Are
Soe at la = 2
we me le ome = :
~ = = s 2
Sm on |S e :
Rl = =
amen oot
teenies
i cena
Sees ane
ie eeee ee
“Qsen- 24mm iden =
rue ie
teeth 1G 2 S20 roommates Tortie a
a a se tome Vices reaeemee
Font meee eS Se acco es cee Siicend ceo”
fe Se ee eee meee upg testes
for eee om ist aera focteuerem —pedoenain el kaon
= = eee ener O14 Tqwn* Rares 1 hata Arties ont ae
a ae cee eee teeta
ar (Saeeec snectini Hares habe Irie
2 cy a een + 1 Soe 6pm Rector © 60 Tags Mi awe
i ars oe egestas tence ester
os pret cos a ea per
* feccimn thames leit
|| i eer ere ee
eo fe See OS SS eee
a
uw ow [eo
eon |e om Ss,
wom lw ow Be SS Soa ot pons ie
Beli Be + See mo far ims foe
Lae el Bat 2 we ae OM =
cee = beeen Sera @ re fee ie
t wo 3. as lee
[Stee LS ac be
= moma fra er
bag coe STF Tia ate mnt eed
PoE Ta wena toe
Uamehe = tate ese rec coe
ee — ee Oa eae ey tee
cs eee thse is
rae Cal n-8 -e < vo WS me WO
Description | Osmolality Use Miscellaneous
0.9% NaClin Tsoronie | Increases Replaces losses without altering
Water (308 mosm) | circulating fluid concentrations
Crystalioid plasma volume |. Helpful for Na+ replacement
Solution when red cells
are adequate
0.45% Natl i Hypotonic | Raises total Userul for dally munintenance of
Water (154 mOsm) | fluid volume body fluid, but is of less value
Crystalloid for replacement of NaCI deficit.
Solution Helpful for establishing renal
function.
Fluid replacement for clients
who don't need extra glucose
= (diabetics) a
Normal saline Isetonic | Replaces fluid Normal saline with Ke, Cars,
with (275 mOsm) | and buffers pH | and lactate (buffer)
electrolytes and Often seen with surgery
buffer
Dextrose Sin | Isotonic (in | Raises total Provides 170-200
water the bag) | fiuld volume. | calories/1,000cc for energy.
Crystalloid *Physiologice | Helpful in |» Phystologicalty hypotonic -
solution lly hypotonic | rehydrating the dextrose is metabolized
(260 mOsm) | and excretory | quickly so that only water
purposes. remains ~ a hypotonic fluid
Dextrose 52 in | Hypertonic | Replaces fluid |e Watch for fuid volume overload
0.9% saline | (560 mOsm) | sodium,
chloride, and
calories,
Dextrose 5% in | Hypertonic | Useful for daily | » Most common postoperative
0.45% saline | (406 mOsm) | maintenance fluid
‘of body fluids
and nutrition,
and for
rehydration.
Dextrose 5% in | Hypertonic | Same as LR Watch for fluid volume overload
Lactated (875 mOsm) | plus provides
Ringer's about 180
calories per
1000ce's
Normosol Tsotonic _ | Replaces fluid pH?
(295 mosm) | and buffers pH | « Contains sodium, chloride,
calcium, potassium and
magnesium
‘Common fluid for aiid PAU]
Common causes ; Less common causes
Malaria
rants by monastca)
Non-specific
Viral ©)
Infection
(comment
ag
Osis |: awagakif Childhood
bisease § Leukaemia!
Pneumonia
\ Typhoid
Cellulitis ®
° wwe
Urinary Arthritis
Septic Tract
arthritis Infection
Fabricated or
Induced Iliness
‘Cranial Nerve Fibres: ‘Structures innervated Functions Brainstem Nucleus
1Olfactory Sensory Olfactory epithelium (via olfactory bulb) (Offaction
WOptic Sensory Retina Vision
Ml Oculomotor ‘Motor ‘Superior/middle/inferior rectus, inferioroblique, | Movementofeyeball | Oculomotornucleus
levator palpebrae.
Parasympathetic | Pupillary constrictor, cilary muscle of eyeball. Both | Pupillary constriction | Oculomotor nucleus
via the ciliary ganglion and accommodation
IWTrochlear ‘Motor ‘Superior oblique Movementofeyeball__| Trochlear nucleus
VTrigeminal ‘Sensory Face, scalp, cornea, nasaland oral cavities, cranial | Generalsensation Trigeminal sensory nucleus
dura mater.
‘Motor Muscles of mastication Opening/closingmouth_| Trigeminal Motor nucleus
TensorTympani muscle Tension oftympanic | Trigeminal Motor nucleus
membrane
‘WiAbducens ‘Motor Lateral rectus Movementofeyeball__| Abducens nucleus
Vil Facial ‘Sensory ‘Anterior 2/3 of tongue Taste Nucleus Solitarius
‘Motor Muscles of facial expression Facial Movement Facial Motor nucleus
Stapedius Muscle Tension of ossicles Facial Motor Nucleus
Parasympathetic | Salivary and lacrimal glands via submandibular and | Salivation and ‘Superior Salivaroty Nucleus
pterygopalatine ganglia Lacrimation
vill Vestibulocochlear | Sensory Cochlea Hearing Cochlear Nucleus
Vestibular apparatus Proriceptionof head, | Vestibularnucleus,
balance.
1XGlossopharyngeal_| Sensory Eustachian tube, middle ear GeneralSensation, Trigeminal Sensory nucleus
Caroitd Body, and sinus Chemo/baroreception
Pharynx, posterior 1/3 of tongue Taste Nucleus Solitarius
‘Motor Styropharyngeous Swallowing
Pare tic | Salivary glands via the otic ganglion Salivation Inferior Salivatory nucleus
X Vagus Sensory Pharynx, larynx, oesophagus, externalear General Sensation Trigeminal Sensory nucleus
Aortic bodiesand arch Chemo/baroreception
Thoracic and abdominal viscera Visceral Sensation Nucleus Solitarus
Motor Soft Palate, larynx, pharynx, upper oesophagus Speech, swallowing Nucleus Ambiguus
Parasympathetic | Cardiovascular, respiratory and gastrointestinal Controlof these Dorsal Motor nucleus of
systems. systems Vagus
XI Accessory Motor Stermomastoid, trapezius Movementofheadand | Nucelus Ambiguus, cranial
shoulders nerves
XII Hypoglossal ‘Motor Intrinsicand extrinsicmuscles of tongue ‘Movementoftongue | Hypoglossalnucleus
You might also like
- טיפול ב חוסרהשקט חדDocument2 pagesטיפול ב חוסרהשקט חדtchanochNo ratings yet
- 10 Common EKG Heart Rhythms PDFDocument1 page10 Common EKG Heart Rhythms PDFtchanochNo ratings yet
- טיפול ב חוסרהשקט חדDocument2 pagesטיפול ב חוסרהשקט חדtchanochNo ratings yet
- 63 Must Know Lab Values Cheat Sheet - NCLEX (Caribbean Nurses of Puerto Rico and Latin America) PDFDocument4 pages63 Must Know Lab Values Cheat Sheet - NCLEX (Caribbean Nurses of Puerto Rico and Latin America) PDFChristineBiankii100% (1)
- Treatment of Acute Agitation in Psychotic Disorders PDFDocument9 pagesTreatment of Acute Agitation in Psychotic Disorders PDFtchanochNo ratings yet
- H B PoemDocument1 pageH B PoemtchanochNo ratings yet
- Drug of Abuse (Table) PDFDocument2 pagesDrug of Abuse (Table) PDFtchanochNo ratings yet
- Ecg Axis DeviationDocument1 pageEcg Axis DeviationtchanochNo ratings yet
- Ecg TopoDocument1 pageEcg TopotchanochNo ratings yet
- Drug of Abuse (Table) B PDFDocument2 pagesDrug of Abuse (Table) B PDFtchanochNo ratings yet
- Ecg AxisDocument1 pageEcg AxistchanochNo ratings yet
- שחזור מרץ 2012Document31 pagesשחזור מרץ 2012tchanoch0% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)