Professional Documents
Culture Documents
Formal 202-4
Uploaded by
api-295856604Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Formal 202-4
Uploaded by
api-295856604Copyright:
Available Formats
PHYSICIAN ASSISTED SUICIDE AND MORAL REASONING
How Moral Reasoning Affects Stance in Agreement or Disagreement to Physician Assisted
Suicide and Euthanasia
Constance Brooks
University of Memphis
PHYSICIAN ASSISTED SUICIDE AND MORAL REASONING
Introduction
Physician assisted suicide or euthanasia has been a debate for some time now, and the
reasoning or justification for performing the act can be viewed by various perspectives (Turner,
1997). My purpose is to determine whether or not physicians, relatives or even patients make a
decision to enable physician assisted suicide based off moral reasoning. In order to do this, the
background of these procedures must be known and the moral reasoning of the persons who are
affected by the decision to enable or not enable the act of euthanizing is important to note as
well.
Discussion
Euthanasia and assisted suicide are terms used to describe the process in which a doctor or close
relative of an ill or disabled person which directly or indirectly leads to the demise of the
individual (2013, pg. 402). To begin discovering the origin of peoples decision to enable a
physician assisted suicide, one could look at the work of theorists. According to Winsor, Murrell
& Magun-Jackson (2015) moral reasoning is how people decide that a behavior or action is right
or wrong. Moral reasoning is separate from religion as Winsor et al., (2015) informs us that
moral reasoning is not how people participate in religious thought. The first theorist to mention is
Jean Piaget who felt that games were great models of society (Winsor et al., 2015). He believed
that there are two stages of one being heteronomous moral development which is moral
reasoning that focuses on how bad the consequences are (Winsor et al., 2015). On the other hand,
stage two is autonomous moral reasoning which focuses on your why he or she does something
(Winsor et al., 2015). If we were to put these two stages in the context of performing a physician
assisted suicide, a person who uses autonomous moral reasoning consider why the procedure was
PHYSICIAN ASSISTED SUICIDE AND MORAL REASONING
done. Maybe the patient requested or the family of the suffering patient has voted to proceed
with euthanasia, but either way the basis for deciding what is right or wrong is based off why the
procedure of physician assisted suicide is being done. As cited in Winsor et al. (2015), Lawrence
Kohlberg gave the analogy of a mans whose wife is terminally ill and has no means to retrieve
the medications. This scenario is relatable to the article written by Huddle (2015) who goes more
in depth and describes a man who is terminally ill and is suffocated by his wife while he is
unconscious, and on the other hand the wife stops the operation of the husbands mechanical
ventilation. Who is to blame in the latter scenario? According to Huddle, (2015) our moral
reasoning can be based on whether we allowed the behavior to occur or if we did the behavior.
This theory also ties with Piagets two stages (Winsor et al., 2015). Our moral compasses can
view the same outcome differently depending on how the outcome was achieved. This leads to
the debate in the aspect of public policy.
Public policy for physician assisted suicide and euthanasia varies all over the world.
According to Levy, Azar, Huberfeld, Siegel & Strous, (2013) most European have laws that view
euthanasia and physician assisted suicide as illegal acts. As mentioned by Levy et al., (2013)
Belgium and the Netherland allow euthanasia due to mental suffering. However, in the same
study it is mentioned that euthanasia and physician assisted suicide are forbidden by law (2013,
pg. 403). There are various guidelines the Dutch Medical Association lays out that the physicians
of the Netherlands must adhere to (Levy et al., 2013). Another issue with public policy is the
role of physicians in the process of physician assisted suicide and euthanasia. The study of Levy
et al, (2013) surveyed 103 subjects in Israel with a range of subspecialties in medicine. The study
found that when the practice was religion controlled the psychiatrist were more conservative in
how they viewed euthanasia than those of other practices (Levy et al., 2013). It was also noted
PHYSICIAN ASSISTED SUICIDE AND MORAL REASONING
that female physicians had more conservative views towards euthanasia than their male
counterparts (Levy et al., 2013). ). According to Leigh Turner (1997) if more than one person is
involved in the decision to proceed with euthanasia the amount of opposition is not as great as
when one person decides. This stems from the notions that both or all parties are in agreement
that no harm is being done to the patient who is terminally ill, and it also ensure that the
procedure is not being requested because of depression or other mental issues (Turner, 1997).
that It can be inferred from the study conducted by Levy et al. (2013) that religion does affect
the views towards physician assisted suicide and euthanasia. The various doctrines of religion
around the globe must also be considered in the stance of how an individual regards physician
assisted suicide and euthanasia.
One moral issue being addressed around the world is the degree to which individuals
should be enabled to determine the circumstances of their own deaths (1997, pg. 191Jewish and
Christian religions view human life as unqualified gift from God which originates reasons to
prohibit death through autonomous decisions (1997, pg. 192). With this being noted, a person
who is a part of such religion would possibly reason that physician assisted suicide and
euthanasia are not acceptable. Jewish and Christians religious communities view life as a gift
from God which leads to the more conservative regard towards physician assisted suicide and
euthanasia (Turner, 1997). Also, as cited in the study of Turner we see that it is written in the
Declaration of the Sacred Congregation for the Doctrine of Faith for the Roman Catholic
church no one is to dispose of their life at will (1997, pg. 196). However, we must realize that
what is acceptable as an explanation for moral reasoning in one community may not be
acceptable to an individual in another community (Turner, 1997). We must also analyze when it
is acceptable to adhere to the wishes of the patient.
PHYSICIAN ASSISTED SUICIDE AND MORAL REASONING
Leigh Turner (1997) informs the readers that a patient cannot request for their physician
or nurse to hasten the dying process. We must also realize that now medicine is more advanced;
therefore, physicians can give a diagnosis and even the symptoms of an illness to expect down
the road (Turner, 1997). This access to such information plays a role in patients requesting
physician assisted suicide or euthanasia (Turner, 1997). The patient has his or her own identity
and moral perspective which is why we must consider everyone and their personal judgement.
This goes against what was discussed earlier with the aspect f religion and the value of life. If
people who are in certain religious communities view their lives as a unimaginable gift which
hold sacred value, their regards towards physician assisted suicide would differ from someone
who bases morality off individualism alone (Turner, 1997).
Conclusion
Physician assisted suicide and euthanasia still have current debates. Even I, myself
experienced a loved and the turmoil caused to proceed with physician assisted suicide, and there
were individuals on both sides of the spectrum of whether to continue with the usage of a feeding
tube or remove the feeding tube and allow for the body enter into a state of utopia and lead to the
loved ones demise. There are so many factors to be considered that moral reasoning is only one
component in the decision to allow a physician assisted suicide or euthanasia. When Piaget is
considered and how it relates to Huddle (2013) you realize that agreements are being made in
how we perceive what is morally right or wrong. But to put in the context of being a patient, a
family member or even the physician and the discussion of performing a physician assisted
suicide or euthanasia we know that there is still much more for debate in generations to come.
There is much work still be done in order to come to common policy on physician assisted
suicide and euthanasia. The differences between individualistic morality and religious based
PHYSICIAN ASSISTED SUICIDE AND MORAL REASONING
morality are both complex in thought, but both aspect affect regards towards physician assisted
suicide and euthanasia.
PHYSICIAN ASSISTED SUICIDE AND MORAL REASONING
References
Huddle, T. S. (2013). Moral fiction or moral fact? The distinction between doing and allowing in medical
ethics. Bioethics, 27(5), 257-262 6p. doi:10.xxx/xxx.xxxx
Levy, T. B., Azar, S., Huberfeld, R., Siegel, A. M., & Strous, R. D. (2013). ATTITUDES TOWARDS
EUTHANASIA AND ASSISTED SUICIDE: A COMPARISON BETWEEN PSYCHIATRISTS
AND OTHER PHYSICIANS. Bioethics, 27(7), 402-408 7p. doi:10.xxx/xxx.xxxx
Turner, L. (1997). Euthanasia and distinctive horizons of moral reasoning. Mortality, 2(3), 191-205 15p.
Winsor, D., Murrell, V. & Magun-Jackson, S.. Lifespan development: An educational psychology
perspective. United States of America: Pearson Education.
You might also like
- Assisted Suicide ThesisDocument10 pagesAssisted Suicide Thesisrebeccadiamondrochester100% (2)
- Euthanasia: Which "M" Is It? Mercy or Murder?From EverandEuthanasia: Which "M" Is It? Mercy or Murder?Rating: 5 out of 5 stars5/5 (1)
- 2004 Parke Jan and Mortimer GlennDocument5 pages2004 Parke Jan and Mortimer Glenncantona78No ratings yet
- Thesis On Physician Assisted SuicideDocument7 pagesThesis On Physician Assisted Suicideafkojmkhs100% (2)
- Research Paper On Physician Assisted SuicideDocument6 pagesResearch Paper On Physician Assisted Suicideorotmbbkf100% (1)
- Research Paper On Legalizing EuthanasiaDocument4 pagesResearch Paper On Legalizing Euthanasiaadyjzcund100% (1)
- Bergman-Levy Et Al. 2012Document7 pagesBergman-Levy Et Al. 2012Danica PerišićNo ratings yet
- Euthanasia SynthesisDocument7 pagesEuthanasia SynthesisBenNo ratings yet
- English I Believe Revised DraftDocument5 pagesEnglish I Believe Revised DraftMoh HensleyNo ratings yet
- Matters of Life and Death: Making Moral Theory Work in Medical Ethics and the LawFrom EverandMatters of Life and Death: Making Moral Theory Work in Medical Ethics and the LawNo ratings yet
- Medicine - Religion - Spirituality: Global Perspectives on Traditional, Complementary, and Alternative HealingFrom EverandMedicine - Religion - Spirituality: Global Perspectives on Traditional, Complementary, and Alternative HealingDorothea LüddeckensNo ratings yet
- Physicians Assisted SuicideDocument10 pagesPhysicians Assisted Suicideapi-272625187No ratings yet
- Flourishing: Health, Disease, and Bioethics in Theological PerspectiveFrom EverandFlourishing: Health, Disease, and Bioethics in Theological PerspectiveNo ratings yet
- Blind Faith: The Unholy Alliance of Religion and MedicineFrom EverandBlind Faith: The Unholy Alliance of Religion and MedicineRating: 4 out of 5 stars4/5 (7)
- Religious Beliefs and Healthcare DecisionsDocument8 pagesReligious Beliefs and Healthcare DecisionsDavid WhiteheadNo ratings yet
- FSU Research Paper Argues Euthanasia and Physician-Assisted Suicide are Morally PermissibleDocument16 pagesFSU Research Paper Argues Euthanasia and Physician-Assisted Suicide are Morally PermissibleMeghan PelehacNo ratings yet
- Expressive Therapies for Sexual Issues: A Social Work PerspectiveFrom EverandExpressive Therapies for Sexual Issues: A Social Work PerspectiveNo ratings yet
- Thesis Statement Against EuthanasiaDocument6 pagesThesis Statement Against Euthanasiadwg1pv0n100% (2)
- Term Paper On Assisted SuicideDocument8 pagesTerm Paper On Assisted Suicideeyewhyvkg100% (1)
- The Impact of Emotional Support in Managing Cardiovascular Diseases Among Hispanic and Non -Hispanic Menopausal Women Aged 55 to 84 YearsFrom EverandThe Impact of Emotional Support in Managing Cardiovascular Diseases Among Hispanic and Non -Hispanic Menopausal Women Aged 55 to 84 YearsNo ratings yet
- Euthanasia Thesis StatementDocument7 pagesEuthanasia Thesis Statementsarahturnerdesmoines100% (2)
- Thesis Statement Against Physician Assisted SuicideDocument8 pagesThesis Statement Against Physician Assisted Suicideallisonweavereugene100% (2)
- Jiquiroz LitreviewDocument17 pagesJiquiroz Litreviewapi-318495757No ratings yet
- Resort To Faith Healing Practices in The Pathway To Care For Mental Illness A Study On Psychiatric Inpatients in OrissaDocument13 pagesResort To Faith Healing Practices in The Pathway To Care For Mental Illness A Study On Psychiatric Inpatients in OrissaGuilherme Alves PereiraNo ratings yet
- Dissertation Lit Review PDFDocument52 pagesDissertation Lit Review PDFSandria KingNo ratings yet
- Legalization of EuthanasiaDocument9 pagesLegalization of EuthanasiaDaniel Sabori HerreraNo ratings yet
- Aging Aggressively:: How to Avoid the Us Health-Care CrisisFrom EverandAging Aggressively:: How to Avoid the Us Health-Care CrisisNo ratings yet
- Factors Associated With Good DeathDocument73 pagesFactors Associated With Good DeathMan MedNo ratings yet
- Literature ReviewDocument7 pagesLiterature Reviewapi-580070141No ratings yet
- Healing America: Hope, Mercy, Justice and Autonomy in the American Health Care SystemFrom EverandHealing America: Hope, Mercy, Justice and Autonomy in the American Health Care SystemNo ratings yet
- Euthanasia LatestDocument8 pagesEuthanasia LatestDenessaLugoNo ratings yet
- Evidence-Based Practices for Christian Counseling and PsychotherapyFrom EverandEvidence-Based Practices for Christian Counseling and PsychotherapyNo ratings yet
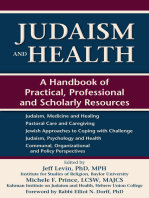
- Judaism and Health: A Handbook of Practical, Professional and Scholarly ResourcesFrom EverandJudaism and Health: A Handbook of Practical, Professional and Scholarly ResourcesNo ratings yet
- Active Euthanasia ThesisDocument4 pagesActive Euthanasia Thesislauriegunlickssiouxfalls100% (1)
- Gender Identity and Faith: Clinical Postures, Tools, and Case Studies for Client-Centered CareFrom EverandGender Identity and Faith: Clinical Postures, Tools, and Case Studies for Client-Centered CareNo ratings yet
- Medical Conditions Associated with Suicide Risk: Suicidal Thoughts and Behavior and Nonadherence to Medical RegimenFrom EverandMedical Conditions Associated with Suicide Risk: Suicidal Thoughts and Behavior and Nonadherence to Medical RegimenNo ratings yet
- Against Euthanasia ThesisDocument4 pagesAgainst Euthanasia Thesispzblktgld100% (2)
- Medical Conditions Associated with Suicide Risk: Prescription Medications and Increased Suicide RiskFrom EverandMedical Conditions Associated with Suicide Risk: Prescription Medications and Increased Suicide RiskNo ratings yet
- Euthanasia Research Paper Thesis StatementDocument4 pagesEuthanasia Research Paper Thesis Statementgbxqaf9v100% (2)
- Good Thesis Statement For Physician Assisted SuicideDocument6 pagesGood Thesis Statement For Physician Assisted Suicidegbvc57fd100% (1)
- Assisted Suicide Thesis StatementDocument8 pagesAssisted Suicide Thesis Statementmarcygilmannorman100% (2)
- Medical Conditions Associated with Suicide Risk: Suicidal Behavior Among Individuals with ArthritisFrom EverandMedical Conditions Associated with Suicide Risk: Suicidal Behavior Among Individuals with ArthritisNo ratings yet
- Medical Conditions Associated with Suicide Risk: Suicidal Risk in Patients with Diabetes MellitusFrom EverandMedical Conditions Associated with Suicide Risk: Suicidal Risk in Patients with Diabetes MellitusNo ratings yet
- Medical Conditions Associated with Suicide Risk: Suicide and Chronic PainFrom EverandMedical Conditions Associated with Suicide Risk: Suicide and Chronic PainNo ratings yet
- Research Paper On Pro EuthanasiaDocument4 pagesResearch Paper On Pro Euthanasiazrpcnkrif100% (1)
- VILLEZAR & CORTEZ RRL - A Right To Die Ethical Dilemmas of Euthanasia PDFDocument13 pagesVILLEZAR & CORTEZ RRL - A Right To Die Ethical Dilemmas of Euthanasia PDFOmar sarmientoNo ratings yet
- Medical Conditions Associated with Suicide Risk: Suicide and Multiple SclerosisFrom EverandMedical Conditions Associated with Suicide Risk: Suicide and Multiple SclerosisNo ratings yet
- Euthanasia Paper ThesisDocument6 pagesEuthanasia Paper Thesislisabrownomaha100% (3)
- Final Project - Assisted SuicideDocument5 pagesFinal Project - Assisted Suicideapi-716442096No ratings yet
- Medical Conditions Associated with Suicide Risk: Suicide and Spinal Cord InjuryFrom EverandMedical Conditions Associated with Suicide Risk: Suicide and Spinal Cord InjuryNo ratings yet
- Medical Conditions Associated with Suicide Risk: Amputation and SuicideFrom EverandMedical Conditions Associated with Suicide Risk: Amputation and SuicideNo ratings yet
- Research Paper Pro EuthanasiaDocument8 pagesResearch Paper Pro Euthanasianekynek1buw3100% (1)
- Medical Conditions Associated with Suicide Risk: Suicide and EpilepsyFrom EverandMedical Conditions Associated with Suicide Risk: Suicide and EpilepsyNo ratings yet
- Research Paper Euthanasia ThesisDocument8 pagesResearch Paper Euthanasia Thesisanitastrongannarbor100% (2)
- Medical Conditions Associated with Suicide Risk: Suicide Risk and CancerFrom EverandMedical Conditions Associated with Suicide Risk: Suicide Risk and CancerNo ratings yet
- NutritionDocument4 pagesNutritionapi-295856604No ratings yet
- Interactive Whiteboard ActivityDocument2 pagesInteractive Whiteboard Activityapi-295856604No ratings yet
- Interactive Learning Activities TableDocument2 pagesInteractive Learning Activities Tableapi-295856604No ratings yet
- Formal 201Document7 pagesFormal 201api-295856604No ratings yet
- Title 2111 Physical DevelopmentDocument4 pagesTitle 2111 Physical Developmentapi-295913850No ratings yet
- Application 1Document1 pageApplication 1api-295856604No ratings yet
- Gambaran Pengetahuan Remaja Mengenai Perilaku Cyber Dating AbuseDocument10 pagesGambaran Pengetahuan Remaja Mengenai Perilaku Cyber Dating AbuseAdrilia AnissaNo ratings yet
- The Communication ProcessDocument2 pagesThe Communication ProcessHamad NaseemNo ratings yet
- Cooperative Learning StrategiesDocument7 pagesCooperative Learning Strategiesverasenan100% (2)
- ExecutiveFunctionInfographic FINALDocument1 pageExecutiveFunctionInfographic FINALJenny M Rodríguez100% (1)
- Who are Opinion Leaders and Seekers in Consumer BehaviorDocument1 pageWho are Opinion Leaders and Seekers in Consumer BehaviorRahul NeelakantanNo ratings yet
- Contacts & Contrasts in Educational Contexts and TranslationDocument196 pagesContacts & Contrasts in Educational Contexts and TranslationqabsNo ratings yet
- Category 1 GuidebookDocument30 pagesCategory 1 GuidebookUsamaTariq100% (1)
- Free Reading Comprehension Worksheet - Active Passive SmokingDocument2 pagesFree Reading Comprehension Worksheet - Active Passive SmokingИлонаNo ratings yet
- QuestionnaireDocument3 pagesQuestionnaireSam Evans88% (8)
- Spain Consumer Values & SegmentationDocument32 pagesSpain Consumer Values & Segmentationsheeba_roNo ratings yet
- Peer Teaching: Presented To DR Samina Malik by Shaista YasirDocument22 pagesPeer Teaching: Presented To DR Samina Malik by Shaista Yasirguddar kooraNo ratings yet
- Research Prob and IntroDocument11 pagesResearch Prob and IntroTop TierNo ratings yet
- Continuum TheoryDocument13 pagesContinuum Theoryhimaja lankaNo ratings yet
- Evaluation of The Use of A Sensory Room On An AdolescentDocument8 pagesEvaluation of The Use of A Sensory Room On An AdolescentKaylee OmanNo ratings yet
- Dual Process Theory To Implicit BiasDocument12 pagesDual Process Theory To Implicit BiasMalley O'Mwaka AmisiNo ratings yet
- Cyclothymia & DysthymiaDocument11 pagesCyclothymia & DysthymiaJulia kwapeNo ratings yet
- TPR ModelDocument10 pagesTPR ModeliniNo ratings yet
- Enhancing Organizational Innovation in Indian Automobile IndustryDocument20 pagesEnhancing Organizational Innovation in Indian Automobile IndustryLejandra MNo ratings yet
- Kapampangan Instructional MaterialsDocument7 pagesKapampangan Instructional MaterialsMej Landayan - CayananNo ratings yet
- Ict and Assessment LearningDocument1 pageIct and Assessment LearningLenoel Nayrb Urquia CosmianoNo ratings yet
- RIASEC and CareersDocument7 pagesRIASEC and Careersziapsychoology100% (1)
- Modified Daily Lesson Log: Mimaropa Region Schools Division of Oriental MindoroDocument7 pagesModified Daily Lesson Log: Mimaropa Region Schools Division of Oriental MindoroHarlene Dela Cruz OzarNo ratings yet
- Gerd Gigerenzer Gut Feelings Short Cuts To BetterDocument6 pagesGerd Gigerenzer Gut Feelings Short Cuts To BetterTruthPathlessJourneyNo ratings yet
- Training and Development A Dissertation: Submitted in Partial Fulfillment For The Award of The Degree ofDocument43 pagesTraining and Development A Dissertation: Submitted in Partial Fulfillment For The Award of The Degree ofAkarsh GuptaNo ratings yet
- Honors in Action RubricDocument6 pagesHonors in Action Rubricapi-290528986No ratings yet
- Pem1 StressDocument20 pagesPem1 StressMarielyn CacheroNo ratings yet
- Counselling ProcessDocument23 pagesCounselling ProcessAshwini ONo ratings yet
- Attributes of Barangay Officials Impact Community ProgressDocument13 pagesAttributes of Barangay Officials Impact Community ProgressRomel FloresNo ratings yet
- 1.2.2 - Motivation in Language LearningDocument5 pages1.2.2 - Motivation in Language LearningZhenFeng ChiaNo ratings yet
- Saying Goodbye After 30 MonthsDocument2 pagesSaying Goodbye After 30 MonthsLucia Diez IbañezNo ratings yet