Professional Documents
Culture Documents
Dropbox - Renal Tubular Disorder
Uploaded by
Jude Roshan Wijesiri0 ratings0% found this document useful (0 votes)
20 views12 pagesrta
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentrta
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
20 views12 pagesDropbox - Renal Tubular Disorder
Uploaded by
Jude Roshan Wijesirirta
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 12
SHPOSIUM: NEPHROLOGY
Renal tubular disorders
David Broodbank
Martin T Christian
Abstract
Renal tubular disorders are challenging and comprise a heterogeneous
‘10up of disorders This review concentrates on those presenting in chi
hood with electrolyte abnoemaltes. Pater recognition of these abr
malts is important in making siagnoses and abasic understanding of
renal tubular physoloy f helpful to understané why these paerns
Cinical cases ae used as ilustations inthis review, supported by
physological descriptions a the dsorders and notes about their manage
ment.
[Athough these disorders almost invalably come under the lng term
management of padi nepivoogss they wills as imal pre-
sent t geneal pacdiatiars. This review should equip general paca
tans wit the skis to request the appropiate inal investigation to
make the correct agnosis. Theres also some advice on when to suspect
diagnosis ofa renal tubular dsorder and how to spot a child with a
senuine polycnsa,
Keywords Barter: cstnesss diabetes insipidus: Fanconi: Gelman’:
oldie: polyutia: pseudohypoalosteronism renal tubular acidosis:
renal tubular disorder tubulopathy
Introduction
Pacdiatricians find tubular disorders challenging: sor
them as cerebral challenges to explore when children have
abnormal electrolytes; others still come out in a sweat at the
thought of having to remember the classifications of renal
tubular acidosis for membership!
There is a tendency for membership candidates to focus on
renal tubular acidosis as the beall and end-all of renal tubular
lisorders. This is unhelpful since proximal renal tubular acidosis,
in fsolation is extremely rare and even distal renal tubular
acidosis is not one of the most common tubulopathies encoun-
tered in clinical practice. 11 is more helpful, we believe, for the
paediatrician to have a feel for the clinical features of the more
common pattems of electrolyte disturbance and learn how
liffering diseases ft into these patterns.
In their entirety, renal tubular disorders are a heterogeneous
group affecting different aspects of tubular function and as such
may present in a variety of ways. Many present with growth
faltering and polyuria/polydipsia as a consequence of
salt-wasting but renal tubular disorders may also be
David Broodbank wacrs maces i an SpR in Poediarc Nephvology at
[Nottingham University Hospitals, Q€C Campus, Nottingham, UK. Con-
Picts of interest: none.
‘Martin T Christan escmo crc i Consultant Palate Nephrologst
{at Nottingham University Hospitals, QMC Campus, Nottingham, UK.
Conflicts of interest: rane.
responsible for renal calculi or hypertension in otherwise
healthy children,
Most commonly, paediatricians encounter renal tubular dis-
lers in the context of investigating a child with abnormal
electrolytes. The disorders are caused, directly or indiscetly,
Lough dysfunction of transporter proteins which are respon
sible for the tubular reabsorption or secretion of various elec:
lrolytes. Within recent years many genes encoding for these
lransporter proteins have been located and these genctic ad
vances have served to improve our understanding of tubular
physiology. However, as yet there is no gene therapy available
for these challenging disorders.
A comprehensive review ofall tubular disorders takes several
chapters in paediatric nephrology texts so this article will offer a
flavour of tubular disorders by focussing on several of the more
common tubulopathies. The individual conditions are ilustrated
through case presentations but the names of patients have been
changed,
[At the end of this article, the reader should have a basic u
derstanding of the role of the renal tubule in homeostasis, un-
derstand how tubular disorders deviate from the norm to result
In their characteristic biochemical patterns and have confidence
in how to begin to investigate a child presenting with electrolytic
derangement
Renal physiology
Faced with abnormal elecicoyte results there is @ need for a
foundational understanding of renal tubular physiology. ‘The
three major functions ofthe kidneys comprise
‘© Maintenance of a constant extracellular environment for
optimum eel functioning (homeostasis).
+ Hozmone secretion (including: erythropoietin for red blood
cell production; renin and angiotensin It affecting renal
and systemic haemodynamies; and hydroxylated vitamin
D affecting caleiaes, phosphate and bone metabolise
‘+ Miscollaneous functions including peptide hormone
catabolism and gluconeogenesis,
Homeostasis is achieved through the kidney excreting waste
products (eg urea and uric acid) and specifically adjusting the
unary excretion of water and electrolytes (Solute) to match the
body's dietary intake and endogenous production through
metabolism
“The human body contains around one million nephrons in
each kidney. This is the functional unit of the kidney and its
precise homeostatic function is achieved through «iffering
properties of cells that define each segment of the tubule 3s well
28 a numberof internal feedback mechanisms which requite the
close juxtaposition of the distal tubule with its parent
slomerulus.
Each nephron comprises a glomerulus and tubule. The
glomerulus, the initial part ofthe nephron, is 3 tal of capillaries
ot by epithelial cells. The endothelial coll and epithelial cell
sandwich the glomerular basement membrane and these struc
tures together constitute a sieve which results in a glomerular
ultrafilyate passing into Bowman's space at the start of the tw
bule. A schematic view ofthe nephron is shown in Figure |
The average adult glomerular filtration rate (GFR) is 125 ml
mnin/1.73 um. Therefore the glomeruli of a healthy adult (of
‘Plesee cite this article in press ax: Broodbank D, Christian MT, Renal tubular disorders, Pamdiatrics amd Chibi Health (2014), beige //slx.docxpy |
10.1016/).paed.2014.03.008
SHPOSIUM: NEPHROLOGY
conex
Bulk iconametic
reabsorption
<
Concentration
Medulla
Figure 1 Simplified drawing of a nephron. Isonatremic reabsorption of
‘tubular Rid takes place inthe proximal tubule inthe cortex. The thick
_ascending limb ofthe loop af Henle ica citing segment in which sodium
Chlotide is avidly recovered but water does na follow. Al the distal
nephron can be regarded asa functional whole. It is derived from the
ginal ureteric bud. IIs responsive to hormones that regulate volume
‘osmolality and potassium concentiate. Note that the junction between
the diluting and concentrating segments meets at the juntaglomersar
apparatus ofthe sel-same nephron providing 3 point at wich tubular
performance regulates the rate of glomerular ftration. (From Forfar and
‘melt figure 16.1)
average body surface area 1.73 m) filter 180 litre of plasma each
day. Since the average daily adult urine production is only 1.5
litre, itis clear that the reabsorptive properties ofthe tubule, for
water at least, must be highly efficient, The fact that 180 litre of
plasma are filtered each day also means that the extracellular
fluid volume is turned over approximately 10 times daily. hence
homeostatic mechanisms with regard to acid—base and electro:
Iyte regulation need to be able to respond rapidly and precisely to
avoid major perturbations in body chesmisty
In gross terms, the proximal tubule and loop of Henle are
bulk resorbers of water and solute whilst the distal tubule has
an important role in fine-tuning may be
across the tubular cells (transcellular) or passively across the
Light junctions in between tubular eells (paracellular). It is the
polarity of tubular cells that gives them their unique properties
Polarity means that the apical (that side of the cell adjacent to
the tubular lumen) and basolateral (that side ofthe cell adjacent
to peritubular capillaries) membranes have differing propertios
through expressing different channels oF transporters. The po-
larity is maintained by the intercollular tight junctions. Most
twansport, both reabsorption and secretion, is Linked directly or
The reabsor
indirectly to sodium reabsorption. ‘The sodium~potassium
‘AtPase pump on the basolateral membrane actively pumps
three sodium ions from the tubular cell into the peritubular
space (where they are subsequently absorbed into peritubular
capillaries) in exchange for two potassium ions, at the cost of
fone molecule of ATP. This active wansporter thus generates a
state of intracellular sodium depletion which favours entry of
sodium from the tubular lumen down an electrochemical
gradient, Sodium is reabsorbed through sodium channels or co-
transporters which link the absorption of sodium to that of other
‘molecules against their own electrochemical gradient. Sodium
seabsomplion in exchange for hydrogen ion secretion in the
proximal tubule is an important example of this and is shown in
Figure 2.
Renal regulation of potassium and acid base balance
Around 65% of filtered potassium is reabsorbed in the proximal
tubule where itis closely linked to the reabsorption of sodium
and water. Here sodium—potassiuim co-ransporters reabsorb
potassium in a similar way to the exeretion of acid shown in
Figure 2, 4 further 30% is reabsorbed in the thick ascending limb
ff the loop of Henle via a sodium co-transporter specific lo the
loop ~ the sodium—potassium—chloride co-transporter, NKCC2
(Figure 3). This eo-transporter is the site of action of loop di
uretics such as furosemide. In the loop there is further reab-
sorption of potassium via the paracellular route which proceeds
down an electrochemical gradient
The remaining S~10% of filtered potassium is deivered to the
distal tubule. In the cortical collecting tubule and duct, there is
both potassium secretion (by principal cells) and potassium
reabsorption (by intercalated cells) but the mote significant
tors affecting potassium excretion
process is secretion,
include.
‘+ Hyperkalaemia (lavours increased potassium secretion,
through a greater osmotic oad).
4 Aldosterone secretion. Aldosterone combines with a eyto-
solic receptor to increase the number of open sodium
PROXIMAL TUBULE
‘Tubular tumen Peri-capllay space
Nak ATPase
basolateral pump
23a"
Net effect:
excretion of
resorption of
“bicarbonate
Cater
cn
Figure 2 The driving force isthe generation of alow intracellular sodium
Concentration when oceure ue to the Na-K ATPase pump inthe baco-
lateral membrane pumping out three sodium ions in exchange fortwo
potassium ions atthe cost af one molecule of ATP
10.1016/),paed.2014.03.005
Tease te saree in press as Boodbunk Dy Chisuan MT, Reval tubular dsorrs, Paciaics wad Chl Heath (2014), Mp0]
SHPOSIUM: NEPHROLOGY
LOOP OF HENLE -THICK ASCENDING LIMB
‘ubulat lumen Peri-capillary space
wore o
-rJ @ ™
Figure 3 In the thick ascending limb ofthe loop of Henle. sodium reab
sorption occurs via the apical sodiumpotassium-chloride channel
(NKCCR) whichis the target of loop dureties such as furosemide. intra
Cellular ow sodium caused by extrusion of sodium by the basolateral
[ATPase pump drives NKCC2. The apical potassium channel ROMK recycles,
Potassium whichis essential for NKCC2 functioning. Chioride is removed
basolateraly by two homologous chovide channels CICKa and CICKE.
They fequite the presence ofthe subunit bartin for normal functioning.
epithelial (ENaC) channels on the apical membranes of
principal cells, thus favouring sodium reabsorption. The
Jumen-negative potential difference that is created favours
potassium excretion via the renal outer medullary
potassium channel (ROMK) but aldosterone also directly
increases the activity of ROMK (Figure 4).
© Filtrate flow rate (greater filtrate flow favours increased
potassium secretion).
The principal cells which comprise 659% of the tubular cols in
the cortical collecting tubule account for most sodium reab-
sorption (via an epithelial sodium channel, ENaC, which is the
site of action of the diuretic amiloride) ancl for most potassiu
secretion (via the inwardly rectifying ROMK channels). ‘This is
illustrated in Pigare 4
‘The other type of tubular cell in the distal tubule is the
intercalated cell, of which there are two subtypes, types A an
B. Type A cells which are more numerous, are responsible for
the secretion of hydrogen ions via apical H* ATPase and H
K* ATPase pumps (Figure 5). Secreted hydrogen ions can
then combine with urinary buffers, most importantly
ammonia, forming ammonium which taps freely difusible
the tubular lumen. Type B cells which are a
reverse polarity form of type A cells, serve to excrete bicar-
bbonate ions. The number and polarity of type B intercalated
cells are determined by plasma pll: metabolic acidosis favours
4 reduction in the number of type B i
reversal of polarity such that they act like type A cells. Loss of
function of either of the apical ATPase pumps results in distal
renal tubular acidosis,
Aldosterone enhances the activity of the apical H* ATPase
pump of type 4 intercalated cells, This is the reason that volume-
contracted sates, such as a hypovolaemic child with nephrotic,
syndrome, may provoke hypokalaemic alkalosis
calated cells an
CORTICAL COLLECTING TUBULE
Pesicapilary space
Figure 4 Sodium moves ito principal els trough fon-specific sodium epithelia channels (ENaC rather
than eo-rancporters ivan by the electrical rather than the osmotic gradient. The distinction is
‘to less than $ mmol/ and this is lower than the intracellular concentration of sodium. Sodium
10.1016/),paed.2014.03.005
Tease te is arco In press as Bodbank Dy Chisuan MT, Reval tabular disor Pacdwics wad Chil Heath 2014), Rp 01 On
SHPOSIUM: NEPHROLOGY
Case 1
Hugh presented at 17 months of age with 2 t-month history of
vomiting and weight loss. On admission, despite clinical signs of
hydration, he remained polyuric with & heavy nappies 2 day. He
had signs suggestive of rickets with splayed wrists and ankles and
‘chic rosary. Weight and height wee both below the 0.4th centile
Usnalysie showed lycosuria and proteinuria 4}. His i
biochemistry shows!
Na 127 mmoltive
K 1.8 mole
Ho, 15 mmole
res 8.6 mmoytitre
Creatinine 78 umole
Calcium 2.34 mmole
PO, 0.71 mmovtixe
Hyponatracmia, hypokalaemia, low bicarbonate and hypo:
phosphataemia are consistent with generalised proximal tubular
dysfunction which is known as Fanconi syndrome. In the prox:
imal tubule there are several types of co-transporter linking
reabsorption of sodium to that of other ions as is demonstrated
with the sodium—hydrogen exchanger illustrated in Figure 2. In
the example sodium reabsorption is in exchange for hydrogen
ons, but the absorption of other ions is Unked with sodium
reabsorption in the same way. Proximal tubular cell funetion is
dependent on the basolateral Na~K ATPase pump. Due to their
‘bulk resorbing capacity, Na~K ATPase dysfunction preferentially
affects proximal tubular cell function.
The diagnosis of Fanconi syndrome can be
uy Findings such as glycosuria, generalised
and inappropriately high urinary potassium and phosphate.
Usine phosphate excretion can be quantified simply by cale
lating tubular reabsorption of phosphate (TRP):
TRP— 100.
(2 Wr fa)
where Up is usinary phosphate, Uc, is urinary creatinine, Pp is
plasma phosphate and Poy is plasina creatinine. Uc, is usually
measured in mmol/litre whereas Po, {8 usually measured in
umol/litre and these need to be converted into the same ui
Outside of infancy the normal TRP is more than 80%.
‘The most common cause of a Fanconi syndrome in Caucasian
children is eystinosis but other rarer causes that are seen not
infrequently by paediatric nephrologists include Lowe's syt
drome, Dent's disease and mitochondrial eytopathies. In Hugh's
case a diagnosis of eystinosis was made promptly by a referral 0
ophthalmology when corneal crystals were seen on slit
‘examination of the cornea. The diagnosis was conlirmed with a
blood test by finding a high concentration of white cell cystine
measured in a reference laboratory.
cystinosis
‘The classical child with cystinosis is fairhaired, blue-eyed and
Caucasian but it also occurs amongst other ethnic groups. The
primary defect isin the gene CTNS which encodes for cystinosin
Cystinosin transports cystine out of lysosomes and th
‘CORTICAL AND MEDULLARY COLLECTING TUBULE
“Tubular lumen
Pet-capilay space
Figure 5 Hydrogen ion excretion takes place in the type A intercalated cells of the cortical and medullary collecting tubule. Intracellular water and
eae ne one ee enone eeeneoeeneese ee een ose oes een oes ee ee
Chloride exchanger in exchange for chloride. Hydrogen fons are secreted by either the H'-ATPase or the HK ATP pumps in the apical membrane.
Secreted hydrogen ions can buffer with ammonia which has freely difused across cellular membrane but becomes trapped inthe tubular lumen 35.
10.1016/),paed.2014.03.005
‘lease cite this aris m press as: Broodbank D, Chiltan MT, Renal tubular disorders, Paediatrics and Child Health (2018), Ripy//ax dolore
SHPOSIUM: NEPHROLOGY
cystinosis cystine is trapped within lysosomes causing malfunc-
tion of the Na-K ATPase.
Symptomatic treatment of cystinosis comprises electrolyte
replacement (potassium and sodium citrate mixlures provide
bicarbonate as well as sodium and potassium since citrate is
‘metabolised to bicarbonate in the liver). Phosphate and activated
vitamin D are also needed to treat the rickets. Indometacin re
duces the glomerular filtration rate and subsequent tubular los-
ses but is also useful to reduce a frequently disabling degree of
polyuria. The Fanconi syndrome causes chronic renal impair:
‘meat and eventually individuals with eystinosis will need renal
replacement therapy. Children with cystinosis frequently have
very poor appetites and severely reduced growth velocity whict
is out of proportion to the degree of renal impairment. Specialist
dietetic support is required and often growth hormone as well to
optimise growth
|A specific treatment for the lysosomal storage is available.
Mereaptamine (previously called cysteamine) combines with
cystine in the lysosome so that a mixed disulphide is able o exit
the lysosome utilising a lysine transporter. The advent of mer:
nine has slowed but not halted the decline of renal fune-
is now more common for childzen with eystiaosis not to
require dialysis or transplantation until at least the second
decade, The drug may also improve growth and slow the
development of other multi-system effects,
Monitoring of leucocyte cystine levels is required after
commencement of treatment, A three to four times daily regime
and the unpleasant side ettects of mercapiamine can all affect
concordance with the drug. Cystinosis is a multisystem disease
and cystine deposition occurs in other organs through life so that
even post-ransplant, mercaptamine needs to be taken regulary.
Sequentially cystine deposition in other organs can cause hypo-
Uyroidism, diabetes mellitus, male infertility, myopathy and
nourological symptoms i
Case 2
Carle's hypokalaemia was picked up following routine blood tests
for investigation of lft thigh pain under the care of orthopaedic
surgery at his local hospital. He was a 14-year-old boy with short
stature, delayed puberty and persistent noctumal enuresis despite
‘multiple traps.
Initial blood results were
Na 136 mmole
K 28 mmole
Heo» 31 mmole
a 90 mmo
Urea 67 mmole
Geatinine 42 umolitre
a 2.41 mmolfire
The pattern of electrolyte abnormalities here is different to the
above Fanconi syndrome case where bicarbonate wasting and
subsequent metabolic acidosis predominate, Metabolic alkalosis,
in combination with hypokalaemia and hypochloraemia is char-
acteristic of sal-wasting disorders of the loop of Henle (Bartter's
syndrome) or early distal convoluted tubule (Citelman’s syn-
drome). In this part of the nepliron, sodium reabsorption is linked
{ochloride reabsorption through the furosemide-sensitive sodium
potassium chloride channel (NKCC2) in the loop of Henle (see
Figure 3) oF the structurally similar thiazide-sensitive sodium
chloride channel (NCCT) in the early distal convoluted tubule
respectively. Salt-wasting disorders from these parts of the
nephron will always be associated with urinary chloride loss in
‘excess of urine sodium loss for the following reasons:
«All chloride reabsorption is linked with sodium, with twice
as much chloride as sodium reabsorbed via NKCC2.
+ Sodium reabsorption but not chloride reabsorption ean
‘occur partly via the paracellular route.
# ‘There is no capacity for chloride reabsorptior
distally
To maintain electrochemical neutrality from increased chloride
loss, other cations are lost which include ammonium and potas-
sium, Ammonia isan important cartier of hydrogen ions in tubular
fluid and so increased ammonium Joss will result in systemic
alkalosis, The urinary potassium loss from this mechanism eom-
bines with the byperkaluria caused by the subsequent secondary
hyperaldosteronisi to cause a profound hypokalaemia,
In Charlie's case the hypocalciuria and hypomagnes
well as the age and el
Iman’s syndrome.
ical presentation are more consistent with
Gitelman’s and Bartter’s syndromes
‘The constellations of symptoms in the first children to be
described with a hypokalaemic, hypochloraemic, metabolic
alkalotic salt-wasting disorder took the name of the clinician who
published the paper in 1960, Frederic Bartter. As more cases
were published, two clinical phenotypes emerged: younger
children with bypercalciuria and nephrocaleinosis, and older
children or adults with hypomagnesaemia and hypocalciuria
‘This latter group was renamed, again after the clinician who fist
‘made the description in 1966, Hille! Gitelman. More recently,
possibly with advances in neonatal intensive care a third
phenotype comprising matermal polyhydramnios, prematurity
and severe polyuria in the neonatal period has been described
and has become known as antenatal Bartte’s syndrome.
Over the last 20 years, genes responsible for these disorders
have been discovered which have greatly contributed to our
understanding of the physiology of the loop of Henle and early
distal convoluted tubule (DCT). Bartter syndrome may therefore
be classified as type I-V which isa system based purely upon the
lorder in which the affected genes were described. The fist to be
described and most logical to understand is a defect in the gene
SLCI2A1 encoding for NKCC2. This usually causes a severe
Albumin 36 gre
Mg 0.64 motive
sin calcium excretion was low and plasma renin and aldosterone
were elevated.
neonatal form of Bartter’s. If ROMK is dysfunctional and return
of potassium to the tubular lumen impaired then this will sul
sequently afect functioning of NKCC2 and thus these two groups
will be phenotypically similar. Disorders of the CIC-Kb compo-
reat of the basolateral chloride transporter cause “classical”
10.1016/),paed.2014.03.005
lease cite this acl i press as: Broodbank D, Chistian MT, Reval lubular donde, Paediatrics and Child Health (2018), Rip: /ax G01 or
SHPOSIUM: NEPHROLOGY
Classification of Bartter’s and Gitelman's syndromes
Classification Gene affected ‘Transporter affected nica picture
Barter syndrome type! SLCI2AY uxcea ‘Antenatal Barter syndrome
Barter syndrome type oun RON Antenatal Barter syndrome
Barter syndrome type IN CCKB ack Chssical Batter syndrome
Barter syndrome type IV &SND Bartin subunit of CIC-Ka and CICKb Antenatal Batter syndrome and
Barter syndrome type V__CLCNKA and cLCNKE
Gelman syndrome Suc12a3 ect
Table 1
Barttr’s syndrome, by which is meant children fitting the early
descriptions of the disorder and not presenting in the neonatal
period. The transporter is present in the thick ascending limb of
the loop of Henle and the early part of the DCT so some of these
children exhibit phenotypic crossover with Gitelman’s. Infants
with a severe salt-wasting disorder and sensori-neural deafness
hhave most recently been found to have a defect of the gene BSND
Which encodes for barttin, a sub-unit of the basolateral chloride
channel which is also present in the inner ear, or a defect of the
‘gene coding for the basolateral chloride channel CIC-Ka and CLC:
kb themselves. The classification is summarised in Table | with
the affected transporters illustrated in Figure 3
Older children with a pure defect of salt reabsorption in the early
DCT have dysfunction of the apical thiazide-sensitive sodium
tuansporter NCCT which s present only in this pat of the nephron,
One ion each of sodium and chloride only is absorbed with this
transporter and an abnormality here results in Citelman syndrome.
‘The I-V classification is rather arbitary and does not assist the
clinician in deducing the underlying abnormality and hence the
clinical presentation. Seyberth suggests that Bartet’s type cond
tions are classified according to pharmacotype, that is, according
to which diuretic the condition mimics. Under this system Type |
would be "Furosemide Type”, Type Il "Furosemice-Armiloride
Type” and so forth. A full description of this classification is
beyond thescopeof this review butt may provide the doctor with a
Uusoful alternative way to classify this group of tubulopathies.
‘Hypercalciuria occurs in Bartier’s because calcium reabsorp-
tion isa linked paracellular process. Hypomagnesaemia does not
jccur because of compensatory reabsorption inthe early DCT. By
contrast, Gitelman’s has hypocaleiuria and hypomagnesaemia
because of a compensatory mechanism in the early DCT which
down-tegulates cells expressing NCCT (and an apical magnesium
channel) in favour of cells which reabsorb sodium and calcium,
Gitelman’s generally presents in older children or even adults
with muscle weakness and cramps, and short stature, It is not
‘uncommonly diagnosed following investigation of growth, con-
gtipation or enuresis. Classical Bartter’s evndrome Is generally a
lca and lex
sensorineural deafness
‘Antenatal Barter syndrome and
sensorineural deafness
Gelman syndrome
‘oxygenase inhibitor Indometacin is especially effective in Bartter’s
syndrome since the salt-wasting is amplified through paracrine
signalling of the prostaglandin PGE. Indeed, antenatal Barter
syndrome is sometimes termed hyperprostaglandin Esyndrome.
Case 3
‘Abdul was the fist child to fst cousin parents. He was born at term
with no neonatal complications. He presented at 2 weeks of age with
‘mucousy vomiting and probably poor feeding. He was acutely hypo.
volaemic and it was very dificult to establish vascular acess. Mis
Intat bloods were:
Na 117 mmole
K 9.5 mmolfitre
Urea 113 mmole
Creatinine 37 mole
pM 698
HCO, 9.2 mmoyitre
Be 19.4
Lactate 73 mmolfitre
He was given emergency treatment for hyperkalaemia including
nebulised salbutamol and an insulin-destose infusion as well as
calcium gluconate to stabilise his myocardium. I was not possible to
obtain a sample for 17a-hydroxyprogesterone intially but this was
obtained several hours later after a dose of hydracotisone was given
Renin and aldosterone were also checked at this tine. The results
17achydroxyprogesterone 20 nmal/itre (normal range
for stressed neonates <40)
Renin 275 mitre (adit reference
ea pn a tine
more severe disorder, presenting in early childhood with growth
faltering, dehydration, hypotonia and lethargy. There is often a
history of maternal polyhydramnios with the classical form but
this feature is always present in antenatal Bartler's
‘These is no targeted treatment for Barter’s of Gitelman’s, Both
require potassium replacement though often magnesium replace
meat alone is sufficient for Gitelman’s. The non-selective eyclo
though high levels may be
‘seen in neonates)
3800 pmofitve (adult
ambulant range: up to 860
pmovfire though may be
higher in citdren)
Aldosterone
10.1016/),paed.2014.03.005
‘lease cite this aris m press as: Broodbank D, Chiltan MT, Renal tubular dsordes, Paediatrics and Child Health (2018), Rip//ax dolore
SHPOSIUM: NEPHROLOGY
The presentation is very similar to that of 21-hydroxylase det
ciency or congenital adrenal hyperplasia (CAH) and a nor
‘7achydroxyprogesterone may have been caused by adrenal
suppression from the hydrocortisone. However the severity of
the hyperkalaemia is against CAH and hyperaldosteronism states
tend to alkalosis. Renin and aldosterone are severely elevated
despite the caveats in the adult reference ranges. This is not
consistent with CAH.
From the tubular pathophysiology angle, comparing this,
pattern of salt-wasting to the above descriptions of Citelman’s
and Fanconi syndromes, the obvious difference is hyperkalaemia
rather than hypokalaemia. With intact distal tubular funetion,
hhyperaldosteronism in the face of hypovolaemia should always
{end to hypokalaemia, This is because the action of aldosterone,
as described above, serves to promote sodium conservation and
potassium loss in the cortical collecting duet. Therefore, hyper:
kalaemia in association with salt-wasting is characteristic of a
distal tubular disorder. This clinica picture is called pseudohy-
ppoaldosteronism because itis the clinical picture of a low aldo-
sterone slate (hyperkalaemia, volume depletion) whereas the
‘measured level of aldasterone is high. Its also known as type 4
renal tubular acidosis included within the classification of renal
tubular acidosis disorders: the acidosis occurs as reduced luminal
potassium provides less substrate for the apical K*-H"
exchanger.
Pseudohypoaldosteronism
Type | pseudohypoaliosteronism exists a8 an autosomal domi
rhant (senal specific) and autosomal recessive (multiple organ)
form. The autosomal dominant form results from a gene muta
tuon encoding for the mineralocorticald receptor. It presents
generally in infancy with growth faltering, vomiting and delty
ration with a biochemical picture of relatively. mild hyper-
kalacmia and hyponatraemia. Plasma renin and aldestesone
levels are elevated,
‘The autosomal recessive form, as might be expected, is more
severe and presents with severe salt-wasting and life-threatening
hhyperkalaemia soon after birth, The disorder is caused by mu
lations in genes encoding for the p and + sub-units of ENaC. The
‘main principle of treatment is adequate sodium replacement (in
the form of both sodium chloride and sodium bicarbonate usu
ally) which may require in excess of 15 mmol/kg sodium per
day, Increased sodium intake results in increased delivery of
sodium to the distal tubule which t a limited extent can
ameliorate the dysfunctional apical sodium channel and permit
‘more potassium secretion. However, the severity of the hyper:
kalaemia is such that a low potassium diet and ion-exchange
resins such as sodium resonium are also normally required to
prevent life-threatening hyperkalaemia. In contrast to the auto-
chronie kidney disease or a combination of these, The differen
liating feature fron 1 above is abnormal renal imaging
and usually the presence of impaired renal function, In this
scenario the pseudohypoaldosteronistn is a secondary phenom-
‘enon caused by a transient tubular insensitivity to aldosterone. A
this to be a surprisingly common compli-
cation of severe urinary tract infection in young infants,
recent review foun
Case 4
Freddie was 3 months with a background of mild developmental
concerms and constipation. He presented with sepsis. On admission
to hospital, the plasma sodium was 152 mmole but this had
Increased to 169 mmole ater he was given a bolus of 0.9% saline
for presumed hypovolaemia
Other biochemistry on admission was as follows:
K 41 mmole
Urea 5 mmobtitre
Creatinine 56 wmofire
Paired urine and plasma samples were taken with
results as follows:
Pq. 161 mmoles
Pra 340 mOsmfitre u,
ig, 12 mmole
1 164 mOseuire
Hypernatracmia usually indicates volume contraction and itis an
appropriate response to consider a fluid bolus in such a situation,
The repeat plasma sodium result was a surprise and suggests
impaired urine concentrating ability. This is confirmed by the
paised samples showing inappropriately dilute urine for thy
hyperosmolar plasma. Such a slate is called diabetes insipidus of
which there are central and nephrogenic forms. Central forms
‘most commonly occur in association with cerebral neoplasms,
craniopharyngiomas most commonly, and this is an unusual age
for a brain tumour. The diagnosis of nephrogenic diabetes
insipidus needs to be made with a desmopressin challenge
demonstrating no improvement in urine concentrating ability in
response to a dose of desmopressin, an arginine vasopressin
analogue. As this child was already hyperosmolar there was no
need to precede the desmopressin challenge with a water
deprivation test. Both a desmopressin challenge and a full water
deprivation tost may induce dangerous levels of dehydration and.
hhypermatraemia. It should only be undertaken with a clear pro-
tocol of weight and plasma/urine osmolality monitoring, with
facilities for tanid reauit tummarcund a0 that the teat can he ome-
ee i eee SS
life-long. There is also abnor
4gans, for example increased pulmonary secretions that may
mimic cystic fibrosis and the multiple organ type may be
confirmed through a positive sweat test
significantly
maturely terminated if
dehydrated
ial sodium transport in other or
Nephrogenic diabetes insipidus (NO).
Under normal physiological conditions water is reabsorbed from
the collecting duct via the water channels (AQP2) which are
presented to the apical membrane (Iusninal side) of the principle
cell of the collecting duct under the influence of arginine
‘Secondary psuedohypoaldosteronism
Blochemically similar presentations to that described above may
occur in the context of urosepsis, urinary tract malformation
. 7 201 Evi Li ee
lease cite this aici i press as: Broodbank D, Chistian MT, Renal tubular donde, Paediatrics and Chil Health (2018), Rip /ax G01 om
10.1016/),paed.2014.03.005
SHPOSIUM: NEPHROLOGY
Membrane shuttle mechanism
Physiologic Pathophysiologic
ADH AQPS AQP pkaked QPS AQP2
Ho NO! HO
- of ® of
r. 2
asotomal
reese
4ADH AQPS a
No! no
ne a
mon Ho mm ¢
camo
=E aara
roe NN = es = oom
Figure 6 Reproduced with permission of Curent Medicine Group. Under the influence of AVP the V2R receptor stimulates a series of cyclic adenosine
‘monophosphate-(AMP) mediated events that results in the fusion of cytoplasmic vesicles, caying water channel proteins (aquaporin? {AQP2D, with
the apical membrane, thereby increasing the water permeability ofthis membrane. Water exits the cll through the basolateral water channels AQP3 and
‘AQP4, Thase with Xnked NOI have a defect inthe V2 receptor withthe remaining group having mutations InvoWing the AQP2 gene. “Guay Woodiord,
eal. Renal tubular disordets, Als Dis Kidney 200:
vasopressin (AVP). This allows water out of the tubule via the
basolateral water channels AQP3 and AQP4 down the favourable
cosmotic gradient created by the removal of solute in the loop of,
Henle and distal tubule (See Figures 1 and 6). X-linked NDI,
Which accounts for 90% of cases, presents in male infancy with
failure to thrive, nonspecific symptoms including fever and
constipation, and episodes of hypernatraemic dehydration. In X-
linked NDI there is a mutation in the AVPR2 gene which encodes
for the AVP receptor V2R with a consequent loss of AVP
responsiveness and failure to mobilise the AQP2 water channels,
Far less commonly, inherited NDI may be caused by muta
tions in the AQP2 gene. This ean be inherited in both an auto-
somal dominant and recessive manner and resulis in the failure
of the AQP2 water channel to migrate to the apical surface of the
collecting duet where concentrating ability is impaired. This
strategy may result in hypokalaemia requiring supplements or
the addition of amiloride. Indometacin may also reduce the
polyuria probably through reducing the GFR and enhancing
Case 5
‘isha presented at 2 month of age with severe grawth falteing to
second cousin parents who were otherwise healthy. At this point she
weighed 2.3kg against a bith weight of3.5 k, She had no history of
Aiarthoea but was dehydrated on examination. She had no rickets.
Biochemistry results were as follows:
principal cell, again impairis
in inappropriately dilute urine.
Management of NDI requires free access to water and as this,
Is not possible for infants they should be fed every one to two
hours. Infants and young children with NDI do not gain weight
well and many need enteral feeding. Pharmacological therapies
include thiazide diuretics and indometacin. tis counterintuitive
to think that 2 diuretic may decrease polyuria but on a tubular
level it makes sense: by inducing a mild degree of volume
depletion sodium reabsorption (and thus water) in the proximal
tubule is enhanced, resulting in less water delivery 10 the
water reabsorption and resulting
Na 140 mmotitre
x 2.7 mmolfite
a 118 mmole
cos 12 mmole
rea 5.8 mmole
Creatinine 35 polite
Comctad Ca 2.9 mmolfite
PO, 17 mmofite
Renal ultrasound showed nephrocacinosis.
10.1016/),paed.2014.03.005
‘lease cite this aris m press as: Broodbank D, Chiltan MT, Renal tubular donde, Paediatrics and Child Health (2018), Ripy//ax dolor
SHPOSIUM: NEPHROLOGY
proximal sodium and water reabsorption although the exact
‘mechanism of its action remains unclear.
Of particular importance to the general paediatrician is that
daring intercurrent illnesses requiring intravenous fluids ebil-
dren with NDI should be managed with 5% dextrose to avoid a
sodium load which will drive the polyuria and rapidly lead to
dangerous hypernatraemia, Strict fluid balance including weight
assessment and frequent electrolyte monitoring is critical in these
patients and they should ideally be managed with regular advice
from a paediatric nephrologist
Investigation of suspected salt-wasting tubular disorders
In hyperchiloraemic metabolic acidosis, the anion gap (Na ~ [Cl
+ HCOs], which should be 5-11 mmol/itre) is normal. This
implies either bicarbonate wasting (lrom gut or kidney) or failure
o appropriately acidify the urine. This pattern of hyper-
chloraemia, metabolic acidosis, hypokalaemia and nephrocal
‘nosis with normal renal function fits best with a distal renal
tubular acidosis (ARTA). The diagnosis of ARTA would be further
supported by a urine pH more than 5.3 and can be confirmed by
an ammonium loading test or other test of distal tubular urinary
acidification
Test
sine dipstick
Venous blood 95
Magnesium
Renin and aldosterone
Usinary chloride
Usinary calcium
Usine pH
sine amino acids
Fractional excretion of sodium (Fy)
‘Transtubular potassium gradient (TTKG)
Interpretation
Gycosuria implies a proximal tubulopathy.
Metabolic alkalosis seen with Barters/itelman's
Metabolic acidosis seen with proximal and distal
tubulopathies.
Hypomagnesaemia occurs in Gtleman’.
Elevated with volume-contracted states,
‘especialy Barter’, Gltelmars and severely so
vith pseudohypoaldosteronism.
High values (>10 mmofitre) in association with
hypochloraemia exclude non-enal causes of
chloride loss.
Hypetcalcuria usually seen in Barter’ whereas
hypocacira is usually seen in Gitiemar's.
Should be performed in the laboratory with 3
glass electrode.
Generalised aminoacidria seen in proximal
‘ubulopathies.
In the Face of volume contaction,FEq, should be
1% (<2.5% in neonates). A result greater than
this confirms a dlagnosis of salt-wastng.
Should be <2.5 with hypokalaemia and >7 with
hyperkalaemia.
Notes
Proteinuria may also be present. Frequently
this Is tow molecular weight proteinuria in
Fanconi syndrome. Requesting urine NAG or
RBP may be helpful
Metabolic acidosis can be investigated
further to ascertain ste of renal tubular
acidosis,
Vial information to interpret hypo- or
hryperkalaemia,
Consult tables for age-specific reference
ranges. Ideally spot sample shouldbe the
second voided sample ofthe day.
pH > 5.5 with a metabolic acidosis
suggests ARTA,
Remember to covert Us, to wmf.
Use if tal tubular dysfunction is
suspected as this fs an indirect index of
potassium secretory activity in the cortical
collecting tubule. TTKG = $t2fon
Where an aNd Urnn are plasma and urinary
Tubular reabsorption of phosphate (TRP)
Values <80% in children >12 months implies TRP
Osmotaiiy respectively.
00 — (")
phosphate leak which, in combination with
hypokalaemia, acidosis, glycosuria and
generalised aminoaciduria implies a Fanconi
‘syndrome,
Handjwise Xray
To look for rickets which may be present with
Fanconi syndromes or in association with
hypercaliuia.
Renal ultrasound
malformations
Table 2
To look for nephrocaeinos's and urinary tract
Nephrocalenosis may be seen with Batters
symdrome, Dent’ disease and distal renal
tubular acidosis.
lease cite this acl i press as: Broodbank D, Chistian MT, Renal tubular disorders, Paediatrics and Chil Health (2018), Rip: /ax G01 om
10.1016/).paed.2014.03.008
SHPOSIUM: NEPHROLOGY
Renal tubular acidosis
The renal contributions to acid-base balance are through bi-
carbonate reclamation and acid secretion. Kidneys resorb 90% of
filtered bicarbonate in the proximal tubule. The proximal tubule
also regenerates bicarbonate so that all this reclaimed bicar
bonate ean be used for buffering — forming carbonic acid and
eventually carbon dioxide which is excreted by the lungs.
‘The collecting tubules are principally responsible for acid
secretion, Buffers in the tubular Lumen bind free hydrogen ions,
allowing excretion of the daily acid load within limits of the
‘miminal achievable urine pIT of 4.5~5. Ammonia and to a lesser
extent phosphate are the main urinary buffers. Ammonia (NH).
which is formed from amino acid metabolism, can freely diffuse
across tubular membranes where it combines with protons to
form ammonium (NIJ) which becomes trapped in the tubular
lumen.
Renal tubular acidosis (RTA) occurs in several ways: bicar
bonate wasting in the proximal tubule (historically known as
type 2 RTA) almost always occurs as part of a Fanconi syndrome
(described incase 1 and associated with hypokalaemia):
Impairment in formation of ammonia results in type 4 RTA
(deseribed in case 3) and in renal failure, where the acidosis is
associated with hyperkalaemia; and failure to adequately secrete
hydrogen ions is the primary defect in dRTA (associated with
hypokalaemia)
In childhood dRTA, most cases are genetic. Autosomal
recessive RTA can be associated with (ATP6VIB1) or without
(ATPSVOAA) sensorineural deafness. Both mutations code for
subunits of the H-ATPase apical hydrogen ion transporter. An
autosomal dominant ARTA is caused by mutations of the SLC4A1
‘gene which encodes the chloride-bicarbonate exchanger on the
basolateral membrane (Figure 5)
Urine pl in dRTa is always more than 5.5 in contrast to
proximal RTA where it varies according to the pla
Donate. Fractional excretion of bicarbonate ance serum bicat:
bonate is normalised should be less than 5% for dRTA. The
diagnosis of a distal RTA can further confirmed with other
tubular functional tests including, acid loading and furosemide
challenge
Initial correction of acidosis needs to lake into accou
po.
-h will both decrease in response to
alkali teatment. Maintenance treatment consists of sodium bi
carbonate or citrate (sodium and/or potassium). Generally the
lassium and caleium wh
I a basic renal profile (Na, K, Cl, HCOs, urea, creatinine, C2,
POs and albumin) suggests sat-wasting and electrolyte distur-
bance, Table 2 shows the next set of investigations to consider.
‘An assessment of volume slalus is essential and weight al this
point can be very helpful as a baseline before rehydration is
commenced. A blood pressure should also be performed and the
appropriate centile noted,
Rarely does alow concentration ofa single electrolyte occurin
isolation and pattern recognition is important as is illustrated
with the cases. Asa general principle, when there isa low plasina
lectrolyte it i usually helpful to look at its concentration in the
urine if there is no other obvious source of loss. There are a
rhumber of specific tests of tubular function based on this prin-
ciple that are listed in the table. To calculate them it is necessary
{0 request urinary creatinine or osmolality for a sample collected
atthe same time as a blood test is earried out requesting the same
P rs. It needs 10 be noted that if urine creatinine is
requested, it will be measured in millimoles perlite (mmol/Litre)
and needs to be converted to micromoles per litre (umol/lire) for
the equations listed
How to spot a polydipsic/potyuric child
Many children drink excessively and the majority of these chil-
dren will have behavioural polydipsia which in its most severe
form ean cause a transient
ypairment of urine concentrating
ability. To identify true polydipsic children it is necessary (0
probe more specifically. Features that are suggestive of 1
polydipsia and polyuria include:
‘© Equally happy to drink water as squash
© Night-time waking for drinks
4 Saturated nappies
‘Unusual drinking habits e.g. drinking water from
from toilets, rom dog drinking bow!
‘© Dehydration-related problems such as low-grade fevers,
inrtability oF constipation
Children whose preference is always for sweetened drinks or
juices, who sleep through the night and who are thriving are less
likely to have pathological polyuria and polydipsia,
bath,
Conclusions
Renal tubular disorders are rare usually life-long disorders that
require specialist management and are therefore usually cared.
doses of base required are less than for proximal acidosis. Chil-
‘deen require lifelong follow-up and are at risk of nephrolithiasis,
and long-term deterioration in renal function fom the
nephrocaleinosis.
How to investigate suspected tubulopathies
‘Tubular disorders must always be considered in the following
situations:
‘© Growth faltering or short stature
‘© Children or infants whose dehydration is out of proportion
to the clinical history
‘© Suspected polyuria/polydipsia
‘© Muscle weakness or unusual lethargy
‘© Intractable nocturnal enuresis
‘or ln peecietric rene comines where they ane sue to access the
‘multi-diseiplinary team including dictitans, specialist nurses and
psychosocial support. However, many who are stable will be
cared for in paediatric renal shared-care clinics, Their presenta-
tion will invariably be to general paediatricians. Prompt diag-
nosis and good initial management may prevent further
the case of certain disorders such as pseudo-
FURTHER READING
For a more detailed review of renal tubular disorders and
‘renal physiology the following texts are recommended:
‘Avner ED, Harmon WE, NiaudetP Yoshikawa N Pediatric nephrology. 6th
dn. Bein Heidelberg: Springer Vetiag, 2009: 37-42.
20 Evi Lis ee
SYHPOSIUM: NEPHROLOGY
‘Comprehensive pediatric nephrology. st edn. Mosby Elsevie, Philadel:
hia PR: 27-32.
Rose BD, Post TW. Clinical physiology of acid—base and eleclyte dis-
‘orders. 5th edn, New Yorks MeGraw-Hil, 2001
For a review of the terminology and classification of Bartter-
like syndrome the following is recommended:
Seyberth H. An improved terminology and classification of Barter ike
‘syndromes. Nat Cll Pract Nephr 2008: 4.
For a brief review in the assessment and investigation of
‘children with apparent polyuria/polydipsia the following is
recommended!
Carr Gil. Polya, plydipsia,polypopsi: “Mummy want adrnk. Arch
is Child Educ Pract Ed 2007; 92: 139-43. Geary OF, Schaefer, 2008.
‘The following reference is a recent case series and review of
secondary pseudohypoaldosteronism
BosdanovicR,StalicN, Putik J. Paripovic A. Transient type 1 pseudo-
hypoaldesteronisme: report on an eight patent series and Uterature
review. Pediatr Nephrol 2009; 24: 2167-75,
PREDATES AMD OALD HEA u 201 Evi Li ee
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Pre Course MCQ For Doctors November 2014 PDFDocument2 pagesPre Course MCQ For Doctors November 2014 PDFJude Roshan Wijesiri100% (1)
- Propranolol For Infantile Haemangioma: Sandeep Ramkrishna Hambarde, Pradnya Suhas Bendre, Ramdas Dagdu NagargojeDocument2 pagesPropranolol For Infantile Haemangioma: Sandeep Ramkrishna Hambarde, Pradnya Suhas Bendre, Ramdas Dagdu NagargojeJude Roshan WijesiriNo ratings yet
- Algorithms - HyperkalaemiaDocument1 pageAlgorithms - HyperkalaemiaJude Roshan WijesiriNo ratings yet
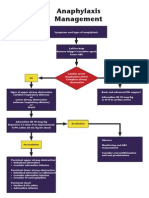
- Algorithms - AnaphylaxisDocument1 pageAlgorithms - AnaphylaxisJude Roshan WijesiriNo ratings yet
- Ventricular Tachycardia (VT) Management: Pulse Present? VF ProtocolDocument1 pageVentricular Tachycardia (VT) Management: Pulse Present? VF ProtocolJude Roshan WijesiriNo ratings yet
- SnakesDocument65 pagesSnakesJude Roshan WijesiriNo ratings yet
- Slma Vaccines Guidelines 2011Document111 pagesSlma Vaccines Guidelines 2011Jude Roshan WijesiriNo ratings yet
- Sri LankaDocument15 pagesSri LankaJude Roshan WijesiriNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)