Professional Documents
Culture Documents
Signos Neurologicos en Dolor de Cabeza
Uploaded by
Anonymous tIjszTfSuGOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Signos Neurologicos en Dolor de Cabeza
Uploaded by
Anonymous tIjszTfSuGCopyright:
Available Formats
Neuroscience Letters 595 (2015) 4144
Contents lists available at ScienceDirect
Neuroscience Letters
journal homepage: www.elsevier.com/locate/neulet
Research article
Neurological soft signs in primary headache patients
L. Tremolizzo , S. Ferrario, A. Pellegrini, L. Fumagalli, C. Ferrarese, I. Appollonio
Neurology Unit, San Gerardo Hospital, Department of Surgery and Translational Medicine (DCMT) and Milan Center for Neuroscience (Neuro-MI),
University of MilanoBicocca, Monza, Italy
h i g h l i g h t s
Neurological soft signs (NSS) are clinical markers of minor brain alterations.
NSS are increased in primary headache outpatients (HP).
NSS are increased in HP expressing white matter hyperintensities at brain imaging.
Headache type and characteristics do not inuence NSS presentation.
NSS identify a subset of primary HP sharing brain anomalies and comorbidities.
a r t i c l e
i n f o
Article history:
Received 31 January 2015
Received in revised form 4 March 2015
Accepted 3 April 2015
Available online 4 April 2015
Keywords:
Comorbidity
Endophenotypes
Episodic frequent tension-type headache
Migraine
Neurological soft signs
White matter hyperintensities
a b s t r a c t
Neurological soft signs (NSS) are semeiotic anomalies not assessed by the standard neurological examination, primarily developed in psychiatric settings and recently proposed as potential markers of
minor brain circuit alterations, especially the cerebellarthalamicprefrontal network. Primary headache
patients present with normal neurological examination and frequent psychiatric comorbidity. Aim of this
exploratory study consisted in assessing NSS in 20 episodic frequent migraine (MH) and in 10 tensiontype headache (ETTH) outpatients compared to 30 matched healthy controls. NSS were assessed by the
Heidelberg scale; clinical characteristics and brain MRI were additionally obtained in all patients. NSS
were increased by 70 and 90% in ETTH and MH, respectively, with respect to controls (p < 0.001)
and the difference remained signicant even after controlling for age and education. Headache type and
characteristics did not inuence NSS presentation, while headache patients with white matter hyperintensities (WMH) at brain MRI had higher NSS scores compared both to normal controls and patients
without WMH. NSS identify a subset of primary headache patients sharing the same comorbidities or
minimal brain anomalies, suggesting that tailored prophylactic options might apply.
2015 Elsevier Ireland Ltd. All rights reserved.
1. Introduction
Neurological soft signs (NSS) are minor semeiotic anomalies
not assessed during the standard neurological examination and
for a long time postulated to indicate a diffuse dysfunction within
the nervous system [1]. A more recent concept assumes the presence of micro-anomalies within more specic brain networks [2,3].
In particular, studies suggest the NSS might predict abnormalities within the cerebellarthalamoprefrontal circuitry [4,5] and
be viewed as an index of cognitive dysmetria [5,6]. NSS assessment encompasses different domains, such as motor coordination
Corresponding author at: Neurology Unit, University of MilanoBicocca, Via
Cadore 48, 20900 Monza, Italy. Tel.: +39 2 6448 8128; fax: +39 2 6448 8108.
E-mail address: lucio.tremolizzo@unimib.it (L. Tremolizzo).
http://dx.doi.org/10.1016/j.neulet.2015.04.007
0304-3940/ 2015 Elsevier Ireland Ltd. All rights reserved.
(e.g., nger-to-nose test or diadochokinesis), up to complex motor
sequences (e.g., Ozeretzkis or Lurias tests), and often include also
sensory integration (e.g., stereognosis or graphesthesia). Furthermore some NSS scales include the assessment of primitive reexes
as well (e.g., snout or Myerson reexes).
NSS have been studied extensively in the eld of psychiatry, and
mainly of schizophrenia [7]; accordingly, several authors considered them as a potential marker for endophenotypes of psychotic
conditions, being already present before transition to psychosis in
at-risk individuals to the same extent as after transition [8] and
even among non psychotic relatives in affected pedigrees [9].
By contrast, NSS expression has been rarely addressed in the
eld of neurology, possibly because the concept of a neurological
semeiotics failing to localize lesions is in dramatic contrast with
its founding principles [10]; the only notable exceptions relate to
NSS correlations with specic cognitive functions and impairments,
mainly of the executive type [1113].
42
L. Tremolizzo et al. / Neuroscience Letters 595 (2015) 4144
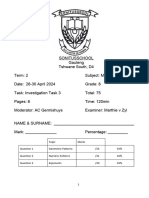
Table 1
Demographic and clinical data. CTRL, healthy controls; ETTH, frequent episodic tension-type headache; MH migraine; NP, not performed; PROF, prophylaxed primary
headache patients (including 3 MH and 2 ETTH). Data are reported as mean SD (range).
Sex, M/F
Age, years
Education,
years
HDI
Symptomatic drugs,
n/month
Frequency, n
attacks/month
CTRL
n = 30
MH
n = 20
ETTH
n = 10
PROF
n=5
7/23
39.7 12.1
(2272)
13.1 3.2
(518)
NP
4/16
40.3 9.3
(2557)
12.7 2.5
(818)
47.1 12.1
(2672)
9.4 5.9
(430)
8.9 3.5
(414)
3/7
39.1 16.6
(2374)
12.2 5.8
(523)
40.6 12.6
(2864)
8.6 3.5
(414)
8.8 3.3
(414)
2/3
40.6 13.7
(2662)
11.2 3.5
(513)
NP
NP
NP
Primary headaches are very prevalent conditions that imply
high social and personal costs with the constant need of developing effective therapeutic strategies [14]. Standard neurological
examination in these disorders is almost always not informative
and often brain imaging studies are requested in order to reach an
exclusion diagnosis. Often these conditions are co-morbid to mood
disorders [15], besides other psychiatric diseases, due to a mix of
psychological adaptation to frequent pain, genetic predisposition,
and neurotransmitter imbalance [1618].
The availability of endophenotypes for psychiatric conditions
in primary headache patients might be useful for further exploring boundaries between these conditions and testing drugs more
rationally. Therefore, the primary aim of this pilot work consisted in
assessing NSS in primary headache patients with respect to healthy
matched controls, assessing as secondary aims the relationship
between NSS scores and headache characteristics both clinical and
of brain imaging.
2. Methods
In this exploratory case-control study, 30 consecutive primary headache patients (HP) were recruited following informed
consent during the headache-free period from the outpatients
afferent to the Neurology Unit. Inclusion criteria were: (a) diagnosis of migraine (MH) with or without aura or frequent episodic
tension-type headache (ETTH) according to current criteria from
the International Headache Society [19]; (b) age >18 and <75 years
old; (c) history of at least 10 episodes and number of attacks 1
and <15/month; (d) no current prophylaxis or other psychoactive
medications; (e) no previous history of neurological or psychiatric
disorders other than headache; (f) a fully normal standard neurological examination.
For both MH patients (n = 20) and ETTH ones (n = 10) number of
attacks/month and number of over-the-counter medication/month
referring to the previous three months period were recorded;
patients were also asked to complete the headache disability inventory (HDI) [20]. Only one MH patient reported more than 15
symptomatic drugs/month (specically n = 30), raising the suspect
of a concomitant medication-overuse headache. Considering the
exploratory nature of this study and the impossibility of a formal a
priori power calculation, the recruited sample size was considered
sufcient for generating the reported preliminary data.
Furthermore, 5 primary headache patients (3 MH and 2
ETTH) taking amitriptyline 10 mg o.d. as prophylaxis (PROF) were
recruited post hoc in order to explore the potential contributory role
on the NSS score of the exposure to anticholinergic and sedative
medications.
Finally, healthy controls (CTRL) were age- (2 years) and sexmatched and education-comparable and they were recruited from
the spouses of other neurological outpatients. They had no previous
NP
NP
history of neurological or psychiatric disorder (including significant headache), nor were they under psychoactive medications.
Demographic and clinical data are included in Table 1.
Besides a complete neurological examination, all patients were
also evaluated for NSS. The examination was carried out in a
calm environment, without interruptions or additional observers.
Among the available tools [21], we choose the 16-items Heidelberg scale [22] since, unlike other batteries, it excludes primitive
reexes. These are, in fact, automatic responses marking, more
properly, cognitive and upper motor neuron dysfunctions [23].
As so, they are qualitatively different from the core NSS, mainly
addressing sensorimotor integration and coordination [22]. In the
Heidelberg scale, the examination procedure is so chosen that the
initial tests are carried out with the patient in a standing position.
The patients ability to perform a given exercise is scored on a 4point scale, from 0 (no difculties) up to 3 (marked difculties).
The Heidelberg scale explores ve different subdomains, as follows:
(1) motor coordination, including: Ozeretskis test, diadochokinesis, pronationsupination, nger-to-thumb opposition, speech and
articulation, (2) integrative functions, including: gait, tandem walking, two-point-discrimination, (3) complex motor tasks, including:
nger-to-nose test, st-edge-palm-test, (4) right/left and spatial
orientation, including: right/left orientation, graphesthesia, facehand test, stereognosis, (5) hard signs, including: arm holding test,
mirror movements. In the original report, this scale was found to
have a high internal reliability (Cronbachs alpha 0.83) and a high
inter-rater reliability (0.88) [22].
All patients also underwent a brain MR scan (1.5 T), including
axial FLAIR sequence (slice thickness 5 mm with a gap of 1 mm;
TR 6000 ms/TE 120 ms; eld of view: AP 230 mm/RL 183 mm/FH
155 mm), performed in order to provide whole brain coverage.
Images were assessed blindly and the Fazekas scale applied to
qualitatively score white matter hyperintensities (WMHs), dividing them in periventricular white matter, and deep white matter
(DWM) signal alterations [24].
Statistical analysis was performed by SPSS. NSS differences
among the recruited groups were assessed by ANCOVA followed
by Bonferroni post hoc test, controlling for age and education. Twotailed Students t-test, ANOVA followed by Bonferroni and Pearson
analysis of correlation were used as appropriate.
3. Results
The impact of age on the NSS score was initially determined in
the group of CTRL (n = 30). However, since the age of the recruited
subjects distributed unevenly in the older group, we recruited 8
more elderly controls. The whole group of CTRL subjects (n = 38)
displayed a very strong correlation with the NSS scores (r = 0.91
p < 0.0001). A similar albeit less strong correlation was present in
primary HP (r = 0.31 p = 0.01 n = 20 and r = 0.65 p < 0.005 n = 10, for
L. Tremolizzo et al. / Neuroscience Letters 595 (2015) 4144
43
Fig. 1. NSS scores. CTRL, healthy controls (n = 30); ETTH, frequent episodic tensiontype headache (n = 10); MH migraine (n = 20); PROF, prophylaxed primary headache
patients (n = 5). Average values are reported. ANCOVA p < 0.001 followed by Sidakcorrected post-hoc test (*p < 0.001 versus all the other groups).
MH and ETTH, respectively). Education years also correlated, negatively, with NSS scores both in CTRL (r = 0.69 p < 0.0001), and MH
(r = 0.52 p = 0.0003) patients, while did not reach signicance in
ETTH ones (r = 0.33 p = 0.082).
The NSS score was increased (70% and 90%, for ETTH and
MH, respectively) in primary HP with respect to CTRL, regardless
of the headache type; the same result was shown including PROF
patients (Fig. 1). Age and education were analyzed as covariates
without modifying this result. Estimated baseline characteristics
(frequency and symptomatic drug use) were not correlated to the
NSS score. On the other hand, HDI scores demonstrated a correlation with NSS (r = 0.54 p = 0.01) only in MH patients. The single
suspect medication-overuse headache did not show differences
with respect to the other MH recruited subjects. HDI correlated
with NSS in the whole HP group as well (r = 0.52 p < 0.003).
Analyzing each NSS separately, HP presented increased values
(p < 0.05) for items belonging to all subdomains: (1) motor coordination (Ozeretzkis test, diadochokinesis, speech and articulation;
3 out of 5 NSS belonging to this category), (2) integrative functions
(tandem walking; 1 out of 3), (3) complex motor tasks (st-edgepalm-test; 1 out of 2), (4) right/left and spatial orientation (right/left
orientation, stereognosis; 2 out of 4), and (5) hard signs (armholding test; 1 out of 2) (data not shown). Dichotomizing HP
according to the diagnostic category, each of these items resulted
signicant at ANOVA (p < 0.05) and MH patients were always different from CTRL at the post hoc test (p < 0.05). On the other hand,
ETTH patients presented a signicant increase versus CTRL only for
items: tandem walking, right/left orientation, st-edge-palm-test,
speech and articulation (data not shown).
WMHs were found in 8 out of 20 MH patients (40%) and 2 out of
10 ETTH patients (20%). At the Fazekas score none of the patients
displayed periventricular white matter signal alterations. Almost
all positive patients displayed a DWM score of 1, and only one
MH patients had a score of 2, while none had a score of 3. Diabetes and dyslipidemia were not represented among the recruited
patients. Three MH patients and one ETTH reported hypertension,
albeit this did not appear to be related to the presence of WMHs.
Dichotomizing patients according to the presence or absence of signal alterations, WMH+ subgroups showed signicantly increased
NSS scores when compared to WMH- for both MH (+40%, p = 0.003,
Fig. 2a) and ETTH (p = 0.05, Fig. 2b). Furthermore, after lumping
patients independently from headache type, a signicant overall
difference in NSS scores (p < 0.0001) emerged at ANOVA. At the subsequent analysis, even with Bonferroni correction, all three tests
were signicant; in particular, HP without WMHs (n = 20, 66%) displayed a signicantly increased NSS score (+58% p < 0.001) with
respect to CTRL (Fig. 2c).
Fig. 2. NSS scores in both (a) MH patients and (b) ETTH ones, dichotomized according to the presence (DWM > 0) or absence (DWM = 0) of WMHs at the Fazekas scale.
#p = 0.003 and p = 0.05 two-tailed Students t-test. (c) Headache patients (HP) with
WMHs (DWM > 0; n = 10) display increased NSS scores with respect to HP without
WMHs (DWM = 0; n = 20) and CTRL (n = 30). ANOVA p < 0.0001, followed by Bonferroni post hoc analysis (p < 0.001 for all the comparisons).
4. Discussion
We report here a clear increase of NSS expression in neurological
outpatients affected by frequent episodic MH or ETTH with respect
to matched controls. However, at least in our sample, NSS did
not differentiate MH from ETTH notwithstanding the impressive
44
L. Tremolizzo et al. / Neuroscience Letters 595 (2015) 4144
differences, in terms of physiopathology, between them. Taken
together, these results seem to suggest the presence of a common
downstream phenotypic trait (or comorbidity) that leads to NSS
increase in both populations.
In addition, given the lack of correlation between NSS and
headache characteristics this hypothetic common factor appears
only minimally related, if at all, to headache severity. One potential
bias to this latter point consisted, however, in obtaining baseline data only from the history, without having a diary. Recruited
patients reported a quite signicant number of attacks/month
(average 9): this might be due to the fact that they have been
recruited as outpatients coming for a neurological consultation and
they might, therefore, display more aggressive diseases within the
denition of episodic frequent.
Moreover, we found increased NSS in headache patients with
WMHs at brain imaging. These data conrm that NSS expression is,
indeed, somehow related to minimal brain circuitry anomalies not
identied by the standard neurological examination and suggests
a minimal localization value for these semeiotic gestures. Indeed,
altered sensory integration and poor motor coordination have
already been previously reported in primary headache patients
[25,26], suggesting that the observed increase in NSS scores might
simply quantify and reect such anomalies.
However, WMHs do not fully explain the higher NSS scores in
HP; in fact, compared to controls, they were higher also in HP without WMHs. One additional intriguing possibility is that a further
common phenotypic trait might be looked for in the psychiatric
eld. Here we included only episodic frequent headaches, since the
relationship between chronic headaches and psychiatric conditions
might be much more complex to unravel [27]. However, mood and
anxiety dysfunctions were not addressed and deserve full consideration as possible links between MH and ETTH in future studies.
In partial contrast is the report that prophylaxis patients display
similar NSS values to untreated patients. These data should be probably replicated considering the reduced size and post hoc nature of
the prophylaxis group, but one issue might be that the amitriptyline dose was quite low for targeting depression. Nevertheless,
the search for this missing psychiatric link in headache might be
very complex to be accomplished, since NSS expression has been
reported unchanged in depressed patients with respect to controls
[28]. On the other hand, obsessivecompulsive disorder, another
relevant headache comorbidity [15], displays increased NSS motor
coordination scores with respect to healthy controls [29].
In conclusion, an overall pattern emerges, where NSS identify
a specic subset of primary headache patients presenting with
more pronounced minimal brain anomalies and, perhaps, psychiatric and/or psychological maladjustment traits. Further studies are
needed, since this subgroup might in principle benet from tailored
prophylactic options.
Conict of interest and sources of funding
None.
Acknowledgment
None.
References
[1] E. Hollander, E. Schiffman, B. Cohen, M.A. Rivera-Stein, W. Rosen, J.M. Gorman,
A.J. Fyer, L. Papp, M.R. Liebowitz, Signs of central nervous system dysfunction
in obsessivecompulsive disorder, Arch. Gen. Psychiatry 47 (1990) 2732.
[2] S.M. Cox, A.M. Ludwig, Neurological soft signs and psychopathology. I.
Findings in schizophrenia, J. Nerv. Ment. Dis. 167 (1979) 161165.
[3] D.W. Heinrichs, R.W. Buchanan, Signicance and meaning of neurological
signs in schizophrenia, Am. J. Psychiatry 145 (1988) 1118.
[4] Q. Zhao, Z. Li, J. Huang, C. Yan, P. Dazzan, C. Pantelis, E.F. Cheung, S.S. Lui, R.C.
Chan, Neurological soft signs are not soft in brain structure and functional
networks: evidence from ALE meta-analysis, Schizophr. Bull. 40 (2014)
626641.
[5] V.A. Mittal, D.J. Dean, J.A. Bernard, J.M. Orr, A. Pelletier-Baldelli, E.E. Carol, T.
Gupta, J. Turner, D.R. Leopold, B.L. Robustelli, Z.B. Millman, Neurological soft
signs predict abnormal cerebellar-thalamic tract development and negative
symptoms in adolescents at high risk for psychosis: a longitudinal
perspective, Schizophr. Bull. 40 (2014) 12041215.
[6] S. Varambally, G. Venkatasubramanian, B.N. Gangadhar, Neurological soft
signs in schizophrenia the past, the present and the future, Indian J.
Psychiatry 54 (2012) 7380.
[7] P. Dazzan, R.M. Murray, Neurological soft signs in rst-episode psychosis: a
systematic review, Br. J. Psychiatry 43 (Suppl) (2002) s50s57.
[8] C. Tamagni, E. Studerus, U. Gschwandtner, J. Aston, S. Borgwardt, A.
Riecher-Rssler, Are neurological soft signs pre-existing markers in
individuals with an at-risk mental state for psychosis? Psychiatry Res. 210
(2013) 427431.
[9] R.C. Chan, I.I. Gottesman, Neurological soft signs as candidate
endophenotypes for schizophrenia: a shooting star or a Northern star?
Neurosci. Biobehav. Rev. 32 (2008) 957971.
[10] L. Tremolizzo, R. Galbusera, M.A. Riva, G.C. Cesana, I. Appollonio, C. Ferrarese,
The hand pronation phenomenon: a franco-german tale, Eur. Neurol. 66
(2011) 165169.
[11] S. Arabzadeh, H. Amini, M. Tehrani-Doost, V. Shari, M. Noroozian, F.
Rahiminejad, Correlation of neurological soft signs and neurocognitive
performance in rst episode psychosis, Psychiatry Res. 220 (2014) 8188, pii:
S0165-1781(14)623-4.
[12] H.J. Li, P.Y. Wang, Y. Jiang, R.C. Chan, H.L. Wang, J. Li, Neurological soft signs in
persons with amnestic mild cognitive impairment and the relationships to
neuropsychological functions, Behav. Brain Funct. 8 (2012) 29.
[13] R.C. Chan, Y. Wang, L. Wang, E.Y. Chen, T.C. Manschreck, Z.J. Li, X. Yu, Q.Y.
Gong, Neurological soft signs and their relationships to neurocognitive
functions: a re-visit with the structural equation modeling design, PLoS One 4
(2009) e8469.
[14] G. Rolle, L. Tremolizzo, F. Somalvico, C. Ferrarese, L.C. Bressan, Pilot trial of
osteopathic manipulative therapy for patients with frequent episodic
tension-type headache, J. Am. Osteopath. Assoc. 114 (2014) 678685.
[15] E. Beghi, G. Bussone, D. DAmico, P. Cortelli, S. Cevoli, G.C. Manzoni, P. Torelli,
M.C. Tonini, G. Allais, R. De Simone, F. DOnofrio, S. Genco, F. Moschiano, M.
Beghi, S. Salvi, Headache, anxiety and depressive disorders: the HADAS study,
J. Headache Pain 11 (2010) 141150.
[16] P. Torelli, G. Abrignani, P. Castellini, G. Lambru, G.C. Manzoni, Human psyche
and headache: tension-type headache, Neurol. Sci. 29 (Suppl. 1) (2008)
S93S95.
[17] C. Gentili, P. Panicucci, M. Guazzelli, Psychiatric comorbidity and
chronicisation in primary headache, J. Headache Pain 6 (2005) 338340.
[18] M. Curone, D. DAmico, G. Bussone, Obsessivecompulsive aspects as
predictors of poor response to treatments in patients with chronic migraine
and medication overuse, Neurol. Sci. 33 (Suppl. 1) (2012) 211213.
[19] Headache Classication Committee of the International Headache Society
(IHS), The international classication of headache disorders, Cephalalgia 33
(2013) 629808, 3rd ed. (beta version).
[20] G.P. Jacobson, N.M. Ramadan, S.K. Aggarwal, C.W. Newman, The Henry Ford
hospital headache disability inventory (HDI), Neurology 44 (1994) 837842.
[21] C.L. Hui, G.H. Wong, C.P. Chiu, M.M. Lam, E.Y. Chen, Potential endophenotype
for schizophrenia: neurological soft signs, Ann. Acad. Med. Singapore 38
(2009) 408413.
[22] J. Schrder, R. Niethammer, F.J. Geider, C. Reitz, M. Binkert, M. Jauss, H. Sauer,
Neurological soft signs in schizophrenia, Schizophr. Res. 6 (1991) 2530.
[23] L. Tremolizzo, E. Susani, C. Lunetta, M. Corbo, C. Ferrarese, I. Appollonio,
Primitive reexes in amyotrophic lateral sclerosis: prevalence and correlates,
J. Neurol. 261 (2014) 11961202.
[24] F. Fazekas, J.B. Chawluk, A. Alavi, H.I. Hurtig, R.A. Zimmerman, MR signal
abnormalities at 1.5 T in Alzheimers dementia and normal aging, AJR Am. J.
Roentgenol. 149 (1987) 351356.
[25] A.M. Harriott, T.J. Schwedt, Migraine is associated with altered processing of
sensory stimuli, Curr. Pain Headache Rep. 18 (2014) 458.
[26] M. Esposito, A. Verrotti, F. Gimigliano, M. Ruberto, S. Agostinelli, G.
Scuccimarra, A. Pascotto, M. Carotenuto, Motor coordination impairment and
migraine in children: a new comorbidity? Eur. J. Pediatr. 171 (2012)
15991604.
[27] F.J. Carod-Artal, Tackling chronic migraine: current perspectives, J. Pain Res. 7
(2014) 185194.
[28] Q. Zhao, Y.T. Ma, S.S. Lui, W.H. Liu, T. Xu, X. Yu, S.P. Tan, Z.R. Wang, M. Qu, Y.
Wang, J. Huang, E.F. Cheung, P. Dazzan, R.C. Chan, Neurological soft signs
discriminate schizophrenia from major depression but not bipolar disorder,
Prog. Neuropsychopharmacol. Biol. Psychiatry 43 (2013) 7278.
[29] Z.W. Peng, T. Xu, G.D. Miao, Q.H. He, Q. Zhao, P. Dazzan, R.C. Chan,
Neurological soft signs in obsessivecompulsive disorder: the effect of
co-morbid psychosis and evidence for familiality, Prog.
Neuropsychopharmacol. Biol. Psychiatry 39 (2012) 200205.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Blood Physiology 2022Document116 pagesBlood Physiology 2022Gurmessa FekaduNo ratings yet
- A. A. Allen The Price of Gods Miracle Working PowerDocument52 pagesA. A. Allen The Price of Gods Miracle Working Powerprijiv86% (7)
- Heat Sink Capacity Mesurment in Inservice PipelineDocument13 pagesHeat Sink Capacity Mesurment in Inservice PipelineSomeshNo ratings yet
- ISO 8861 Blower Engine RoomDocument28 pagesISO 8861 Blower Engine Roommohammad choirul huda100% (1)
- PDS Syncade RADocument6 pagesPDS Syncade RAKeith userNo ratings yet
- Newton Papers Letter Nat Phil Cohen EdDocument512 pagesNewton Papers Letter Nat Phil Cohen EdFernando ProtoNo ratings yet
- Heat Shrink CoatingDocument5 pagesHeat Shrink CoatingMekhmanNo ratings yet
- Numerical WindingDocument12 pagesNumerical Windingsujal jhaNo ratings yet
- Exercises On Algebra MI1036Document12 pagesExercises On Algebra MI1036Sâm Mai HuyềnNo ratings yet
- Herpes Simplex KeratitisDocument20 pagesHerpes Simplex KeratitisriskhapangestikaNo ratings yet
- EngineeringDocument107 pagesEngineeringSuezakumeNo ratings yet
- S800 SCL SR - 2CCC413009B0201 PDFDocument16 pagesS800 SCL SR - 2CCC413009B0201 PDFBalan PalaniappanNo ratings yet
- Construction and Building Materials: Paolo ForaboschiDocument21 pagesConstruction and Building Materials: Paolo ForaboschiMarco CamposNo ratings yet
- Sa 387Document6 pagesSa 387ismaelarchilacastilloNo ratings yet
- ACP Supplement For SVR AUG 2017Document104 pagesACP Supplement For SVR AUG 2017Kasun WijerathnaNo ratings yet
- Car Frontal ImpactDocument25 pagesCar Frontal Impactapi-3762972100% (1)
- Mechanics of Solids - (Riveted and Welded Joints)Document37 pagesMechanics of Solids - (Riveted and Welded Joints)TusherNo ratings yet
- Indigenous Resources ActivitiesDocument17 pagesIndigenous Resources Activitiesscribbler49971100% (1)
- TrerwtsdsDocument167 pagesTrerwtsdsvinicius gomes duarteNo ratings yet
- Hemiplegia Case 18.12.21Document5 pagesHemiplegia Case 18.12.21Beedhan KandelNo ratings yet
- ShimadzuDocument66 pagesShimadzueka_setyowati0No ratings yet
- QuizBowl QuestionsDocument84 pagesQuizBowl QuestionsJowel MercadoNo ratings yet
- I Give You Glory LyricsDocument5 pagesI Give You Glory LyricsJhy Sandro MarkusNo ratings yet
- Ecs C42iix Rev C Vit m2400 1Document36 pagesEcs C42iix Rev C Vit m2400 1Victor Pic100% (1)
- 1cobalt Is An Element in Period 4 of The Periodic TableDocument3 pages1cobalt Is An Element in Period 4 of The Periodic TableZigla MooreNo ratings yet
- Outline On Dengue Fever - EDITEDDocument2 pagesOutline On Dengue Fever - EDITEDDavid Skeat0% (1)
- JVC KD-G331Document179 pagesJVC KD-G331Saša DumanovićNo ratings yet
- Proline Table-Top Machines Z005 Up To Z100: Product InformationDocument2 pagesProline Table-Top Machines Z005 Up To Z100: Product InformationErika Mae EnticoNo ratings yet
- Investigation Gr. 8Document6 pagesInvestigation Gr. 8Marthie van zylNo ratings yet
- uPASS Target: Installation GuideDocument40 pagesuPASS Target: Installation GuideMohammed ElsayedNo ratings yet