Professional Documents
Culture Documents
2009.prasugrel in Clinical Practice..
Uploaded by
tristan9454Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2009.prasugrel in Clinical Practice..
Uploaded by
tristan9454Copyright:
Available Formats
PERS PE C T IV E Prasugrel in Clinical Practice
Prasugrel in Clinical Practice
Deepak L. Bhatt, M.D., M.P.H.
O n July 10, 2009, after an
18-month review, the Food
and Drug Administration (FDA)
prasugrel, is more effective than
ticlopidine and clopidogrel at in-
hibiting the ADP receptor (see dia-
of dual-antiplatelet therapy is war-
ranted after an acute coronary
syndrome. Questions of cost and
approved the thienopyridine pra- gram) — largely because it is serious risk of bleeding must be
sugrel for use in patients with more efficiently metabolized, so considered, but lifelong dual-
unstable angina or myocardial more active metabolite is deliv- antiplatelet therapy may be ben-
infarction who undergo percuta- ered to the platelet. Therefore, eficial for patients with a previ-
neous coronary intervention prasugrel prevents platelet activa- ous acute coronary syndrome.
(PCI). The new drug is the latest tion to a greater degree than does The future availability of generic
addition to a class of agents that clopidogrel at current doses. In clopidogrel and ongoing trials
inhibit the platelet adenosine theory, this greater ex vivo effect of other antiplatelet agents may
diphosphate (ADP) receptor, pre- should translate into a greater make such use more palatable.
venting initial platelet activation reduction in ischemic events — Many practical questions re-
and consequent platelet aggre- but it may also lead to more main. Although TRITON–TIMI
gation — a mechanism that has bleeding.2 Both hypotheses were 38 demonstrated a reduction in
represented a major advance in verified in the Trial to Assess the risk of myocardial infarction
the treatment of atherothrom- Improvement in Therapeutic Out- and stent thrombosis, there was
botic diseases.1 Indeed, the use comes by Optimizing Platelet In- an increase in major bleeding
of the thienopyridine ticlopidine hibition with Prasugrel–Throm- events, including a small but
in combination with aspirin to bolysis in Myocardial Infarction statistically significant excess of
inhibit platelet aggregation facili- (TRITON–TIMI) 38 (ClinicalTrials. fatal bleeding events (approxi-
tated the widespread use of cor- gov number, NCT00097591).3 mately 3 such events per 1000 pa-
onary-artery stenting. Because of Moreover, the risk of bleeding tients treated). Three subgroups
the potential for serious side ef- might be increased still further appeared to be particularly prone
fects such as neutropenia, ticlo- with real-life use, and the FDA to serious bleeding: the elderly,
pidine was quickly eclipsed by has required that prasugrel’s la- the underweight, and patients
clopidogrel, which had better he- beling include a black-box warn- with a previous stroke or tran-
matologic safety and fewer gas- ing about that risk. sient ischemic attack. Although
trointestinal side effects. Clopid- Among 13,608 study patients studies of clopidogrel have iden-
ogrel monotherapy was shown to with unstable angina or myocar- tified polyvascular disease as a
be somewhat superior to aspirin dial infarction who were under- predictor of benefit from dual-
monotherapy for preventing re- going planned PCI, prasugrel sig- antiplatelet therapy, in the small
current ischemic events in pa- nificantly reduced the risks of subgroup of patients in this
tients with recent myocardial recurrent myocardial infarction study with a previous stroke or
infarction, ischemic stroke, or and stent thrombosis as com- transient ischemic attack, prasu-
symptomatic peripheral arterial pared with clopidogrel. The ben- grel significantly increased the
disease, but because of its cost, efits were particularly sizable rate of intracranial hemorrhage.
it did not replace aspirin, instead among patients with diabetes or Therefore, it would be best to
becoming an alternative for pa- ST-segment elevation. There ap- avoid prasugrel in such patients.
tients who could not tolerate peared to be continued benefit Regarding the observations in
aspirin. Trials in patients with over the 15 months of the trial. the elderly and underweight, the
acute coronary syndromes and This study pushes the stan- pharmacokinetic data suggest that
those undergoing coronary stent- dard for the appropriate duration in patients who are 75 years of
ing showed that the combination of dual-antiplatelet therapy for age or older or who weigh less
of aspirin and clopidogrel was acute coronary syndromes (cur- than 60 kg, reducing the prasu-
superior to aspirin alone during rently 12 months) to at least 15 grel dose would probably miti-
12 months of treatment. months. What is uncertain is gate the bleeding risk. Instead
The new member of the class, whether an indefinite duration of the usual maintenance dose of
940 n engl j med 361;10 nejm.org september 3, 2009
Downloaded from www.nejm.org at UNIVERSITE RENE DESCARTES on September 3, 2009 .
Copyright © 2009 Massachusetts Medical Society. All rights reserved.
PE R S PE C T IV E Prasugrel in Clinical Practice
were having planned PCIs. A small
Prasugrel number of patients, however, went
O on to undergo coronary-artery
bypass grafting (CABG). Among
O
N these patients, the rate of major
bleeding in the prasugrel group
CH3 O
S F Rapid
absorption was more than four times that
after oral in the clopidogrel group (13.4%
ingestion vs. 3.2%). Cardiac surgeons who
have been reluctant to operate on
Hydrolysis by patients receiving clopidogrel will
esterases
probably find prasugrel even more
Liver
Oxidation by
objectionable. Thus, the strategy
cytochrome P-450 of administering prasugrel in the
emergency department to patients
ADP
with acute coronary syndromes
Active metabolite
will be viewed as problematic and
is untested, although an ongoing
trial is comparing prasugrel with
clopidogrel in the initial medical
Platelet ADP P2Y12 management of acute coronary
receptor syndromes. Until such data have
Platelet
activation decreased
been examined, early prasugrel
treatment without delineation of
the coronary anatomy by cardiac
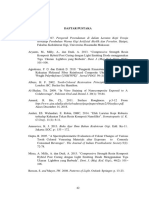
Mechanism of Action of Prasugrel. catheterization should not be rou-
COLOR FIGURE
Prasugrel is a prodrug with rapid and almost complete absorption after oral ingestion
Draft 7 7/14/09 tine in patients with myocardial
of a loading dose. It is metabolized into its active form, which
Author
binds irreversibly to the
Bhatt infarction without ST-segment ele-
adenosine diphosphate (ADP) P2Y12 receptor on platelets Fig for
# their 1 lifespan, thereby
vation. The finding of increased
inhibiting their activation and decreasing subsequent platelet
Title aggregation.
Mechanism Hydrolysis
of action
by intestinal carboxylesterases and oxidation by intestinal and
Prasurgrel
hepatic cytochrome bleeding rates among patients
ME
P-450 enzymes convert prasugrel into its active metabolite. DE Prasugrel Curfman has a greater
undergoing CABG also raises
antiplatelet effect than clopidogrel because it is metabolized
ArtistmoreKnoper
efficiently. Genetic concern about potentially elevat-
polymorphisms affecting the cytochrome P-450 system mayFigure explain
AUTHOR some
PLEASEof the differ-
NOTE:
has been redrawn and type has been reset ed risks of bleeding from non-
ences in metabolism between prasugrel and clopidogrel. Please check carefully
Issue date 3/05/09
CABG surgery that might occur
in patients who have received
10 mg a day, 5 mg is recommend- have frequent nuisance bleeding prasugrel in the previous 7 days.
ed in patients who weigh less when taking the higher dose. It will be important to accumu-
than 60 kg. It is hoped that even Again, there is no direct evi- late registry data to examine the
at lower doses, prasugrel will still dence that efficacy would be rate of bleeding outside the care-
be more effective than clopido- maintained, nor that switching fully defined population of a
grel; confirmation may be forth- to clopidogrel would be safer in clinical trial.
coming from an ongoing phase patients who have bleeding on Recent concerns regarding the
3 clinical trial. Prasugrel would standard-dose prasugrel. These risk of thrombosis with drug-
generally not be recommended questions are worthy of explora- eluting stents have captured the
for patients 75 years of age or tion. There is a potential role for attention of interventional cardi-
older, though it might be con- point-of-care testing of platelet ologists,4 some of whom will un-
sidered if they were at high risk function, and ongoing trials may doubtedly want to use prasugrel
because of diabetes or previous clarify whether assay-guided dose in patients undergoing complex
myocardial infarction. determinations affect the rates stenting procedures. In TRITON–
The option of using a lower of ischemic events or the bleed- TIMI 38, the finding of an ap-
dose of prasugrel is appealing ing risk. proximately 50% reduction in the
— for example, for patients who Patients in TRITON–TIMI 38 rate of stent thrombosis held true
n engl j med 361;10 nejm.org september 3, 2009 941
Downloaded from www.nejm.org at UNIVERSITE RENE DESCARTES on September 3, 2009 .
Copyright © 2009 Massachusetts Medical Society. All rights reserved.
PERS PE C T IV E Prasugrel in Clinical Practice
for both drug-eluting and bare- elevation myocardial infarction. No other potential conflict of interest rele-
vant to this article was reported.
metal stents. Reductions were Use in the elderly should be
seen in both early and late stent avoided except in high-risk situa-
From the Department of Cardiology at the
thrombosis. However, patients tions. Lower maintenance doses Veterans Affairs (VA) Boston Healthcare
with acute coronary syndromes in the underweight appear to be System and the integrated interventional
are at greater risk for stent throm- warranted, though prospective cardiovascular program at Brigham and
Women’s Hospital and the VA Boston
bosis (and recurrent ischemic confirmation of this strategy is Healthcare System — both in Boston.
events in general) than patients necessary. Routine prasugrel ad-
undergoing elective PCI.5 Even ministration in the emergency This article (10.1056/NEJMp0806848) was
complex PCI carries a much low- department for myocardial in- published on July 15, 2009, at NEJM.org.
er risk of future thrombotic events farction without ST-segment ele-
1. Meadows TA, Bhatt DL. Clinical aspects
if the patient does not have an vation appears premature. Using
of platelet inhibitors and thrombus forma-
acute coronary syndrome. There- prasugrel in initial medical man- tion. Circ Res 2007;100:1261-75.
fore, we should be cautious about agement for patients with acute 2. Bhatt DL. Intensifying platelet inhibition
— navigating between Scylla and Charybdis.
recommending prasugrel routine- coronary syndromes is currently
N Engl J Med 2007;357:2078-81.
ly after elective PCI. not warranted but is under study. 3. Wiviott SD, Braunwald E, McCabe CH, et
Prasugrel represents an advance Although routine use after com- al. Prasugrel versus clopidogrel in patients
with acute coronary syndromes. N Engl J
in antiplatelet therapy for acute plex elective PCI is appealing,
Med 2007;357:2001-15.
coronary syndromes. TRITON– this, too, should probably be 4. Curfman GD, Morrissey S, Jarcho JA, Dra-
TIMI 38 supports its use in pa- avoided until further study has zen JM. Drug-eluting coronary stents —
promise and uncertainty. N Engl J Med
tients with such syndromes when been completed.
2007;356:1059-60.
there is a very high probability Dr. Bhatt reports receiving honoraria, 5. Bavry AA, Bhatt DL. Appropriate use of
of PCI, such as in myocardial in- speaker’s fees, and consulting fees from a drug-eluting stents: balancing the reduction
number of pharmaceutical companies, in- in restenosis with the concern of late throm-
farction with ST-segment eleva-
cluding Eli Lilly, Daiichi Sankyo, Sanofi- bosis. Lancet 2008;371:2134-43. [Erratum,
tion or after coronary angiography Aventis, and Bristol-Myers Squibb, and do- Lancet 2008;372:536.]
in patients with non–ST-segment nating them to nonprofit organizations. Copyright © 2009 Massachusetts Medical Society.
Weighing Benefits and Risks — The FDA’s Review of Prasugrel
Ellis F. Unger, M.D.
T he Food and Drug Adminis-
tration (FDA) approved pras-
ugrel on July 10, 2009. Developed
The Trial to Assess Improve-
ment in Therapeutic Outcomes
by Optimizing Platelet Inhibition
vation myocardial infarction and
the other including patients with
ST-segment-elevation myocardial
by Eli Lilly and Daiichi Sankyo, with Prasugrel–Thrombolysis in infarction. The primary compos-
prasugrel is a thienopyridine that Myocardial Infarction (TRITON– ite end point included death from
inhibits platelet aggregation. It TIMI) 38 (ClinicalTrials.gov num- cardiovascular causes, nonfatal
was approved for the reduction of ber, NCT00097591) provided the myocardial infarction, and non-
thrombotic cardiovascular events principal evidence of prasugrel’s fatal stroke, as measured in an
in patients with acute coronary effectiveness3 and tested the hy- analysis of time to first event. A
syndrome (unstable angina or pothesis that prasugrel plus as- total of 13,608 patients were en-
myocardial infarction) who under pirin was more effective than rolled in the trial; the results
go percutaneous coronary inter- clopidogrel plus aspirin for the showed that 9.4% of patients had
vention (PCI). The FDA grappled treatment of patients with an an end-point event with prasug-
with a number of complex issues acute coronary syndrome who rel vs. 11.5% with clopidogrel,
during the review process,1 and were undergoing PCI. Randomiza- P<0.001; this was an 18.8% reduc-
the application was presented to tion was stratified according to tion in the composite end point
the Cardiovascular and Renal presentation, with one stratum overall. The difference was driven
Drugs Advisory Committee on including patients with unstable primarily by a reduction in the
February 3, 2009.2 angina and non–ST-segment-ele- rate of nonfatal myocardial infarc-
942 n engl j med 361;10 nejm.org september 3, 2009
Downloaded from www.nejm.org at UNIVERSITE RENE DESCARTES on September 3, 2009 .
Copyright © 2009 Massachusetts Medical Society. All rights reserved.
You might also like
- Lessons Learned From The Dog GenomeDocument11 pagesLessons Learned From The Dog GenomebellonicoNo ratings yet
- Narrativa Analysis Catherine - Kohler - Riessman PDFDocument9 pagesNarrativa Analysis Catherine - Kohler - Riessman PDFJéssica FigueiredoNo ratings yet
- CURE TrialDocument9 pagesCURE TrialCristina PazmiñoNo ratings yet
- Editorial 2Document4 pagesEditorial 2david1086No ratings yet
- Combined Therapy With Clopidogrel and Aspirin Significantly Increases The Bleeding Time Through A Synergistic Antiplatelet ActionDocument6 pagesCombined Therapy With Clopidogrel and Aspirin Significantly Increases The Bleeding Time Through A Synergistic Antiplatelet ActionAnjas DwikaNo ratings yet
- Anti Platelet PreopDocument6 pagesAnti Platelet Preopbrigde_xNo ratings yet
- Br. J. Anaesth. 2007 Chassot 316 28Document13 pagesBr. J. Anaesth. 2007 Chassot 316 28Rhahima SyafrilNo ratings yet
- Novel Antiplatelet Strategies in Acute Coronary Syndromes: Marc S. Sabatine, MD, MPHDocument8 pagesNovel Antiplatelet Strategies in Acute Coronary Syndromes: Marc S. Sabatine, MD, MPHNagatzulNo ratings yet
- Jaha 117 007288Document4 pagesJaha 117 007288Alberto PolimeniNo ratings yet
- Evidencia Clinica de Antiagregantes Plaquetarios y Ima 2015Document11 pagesEvidencia Clinica de Antiagregantes Plaquetarios y Ima 2015Edgar PazNo ratings yet
- Antiplatelet Therapy: New Antiplatelet Drugs in PerspectiveDocument4 pagesAntiplatelet Therapy: New Antiplatelet Drugs in Perspectivegeo_mmsNo ratings yet
- White 2012 Champion PooledDocument13 pagesWhite 2012 Champion PooledRadu CiprianNo ratings yet
- GI Bleeding in Patients Receiving Antiplatelets and Anticoagulant TherapyDocument11 pagesGI Bleeding in Patients Receiving Antiplatelets and Anticoagulant TherapyTony LeeNo ratings yet
- Antiplatelt Before During and Post PCIDocument8 pagesAntiplatelt Before During and Post PCIVivekanandGuptaNo ratings yet
- Circulationaha.119.039253.PDF J 3Document3 pagesCirculationaha.119.039253.PDF J 3Yuni IndrianiNo ratings yet
- Advances in Atherosclerosis, Atrial Fibrillation, and Valvular DiseaseDocument2 pagesAdvances in Atherosclerosis, Atrial Fibrillation, and Valvular DiseaseLuis AlbertoNo ratings yet
- Prasugrel Versus Clopidogrel in Patients With Acute Coronary SyndromesDocument15 pagesPrasugrel Versus Clopidogrel in Patients With Acute Coronary SyndromesDito LopezNo ratings yet
- Pharmacology Before, During and After Percutaneous Coronary InterventioDocument8 pagesPharmacology Before, During and After Percutaneous Coronary InterventiosamuelNo ratings yet
- Furtado 2016Document10 pagesFurtado 2016zzzzNo ratings yet
- Cardioembolic Stroke: Everything Has Changed: J David SpenceDocument8 pagesCardioembolic Stroke: Everything Has Changed: J David SpenceWaoNo ratings yet
- Nejmoa 010746Document9 pagesNejmoa 010746Mmle BlaséNo ratings yet
- 0718 4026 Rchcir 70 03 0291Document9 pages0718 4026 Rchcir 70 03 0291Erick ToHuNo ratings yet
- Manejo Perioperatorio de Pacientes Usuarios de Antiagregantes PlaquetariosDocument9 pagesManejo Perioperatorio de Pacientes Usuarios de Antiagregantes PlaquetariosErick ToHuNo ratings yet
- Cit0110 Feature WilliamsDocument3 pagesCit0110 Feature WilliamsVidaOpinaldoNo ratings yet
- Combining Antiplatelet and Anticoagulant Therapy in Cardiovascular Disease - 2020 - AHADocument7 pagesCombining Antiplatelet and Anticoagulant Therapy in Cardiovascular Disease - 2020 - AHADrHellenNo ratings yet
- Thrombosis Research: Regular ArticleDocument4 pagesThrombosis Research: Regular ArticleDavy JonesNo ratings yet
- Optimal Duration of Dual Antiplatelet Therapy Post PCIDocument5 pagesOptimal Duration of Dual Antiplatelet Therapy Post PCIvinaNo ratings yet
- Nejmc 0909586Document4 pagesNejmc 0909586theboy14juneNo ratings yet
- Pharmacology Before, During and After Percutaneous Coronary InterventionDocument8 pagesPharmacology Before, During and After Percutaneous Coronary InterventionSharan SahotaNo ratings yet
- 1 s2.0 S0735109716003995 MainDocument2 pages1 s2.0 S0735109716003995 MaintopanNo ratings yet
- 1 s2.0 S0735109719300956 MainDocument9 pages1 s2.0 S0735109719300956 MainAlberto PolimeniNo ratings yet
- 309 Novel Anti-Platelet Agents and AnticoagulantsDocument13 pages309 Novel Anti-Platelet Agents and AnticoagulantsPhani NadellaNo ratings yet
- What Are Optimal P2Y12 Inhibitor and Schedule of Administration in Patients With Acute Coronary Syndrome?Document10 pagesWhat Are Optimal P2Y12 Inhibitor and Schedule of Administration in Patients With Acute Coronary Syndrome?david1086No ratings yet
- NEJM 2017 Comentario Braunwald2017Document2 pagesNEJM 2017 Comentario Braunwald2017Francisca Javiera Yáñez VidalNo ratings yet
- Stroke 1998 Gorelick 1737Document9 pagesStroke 1998 Gorelick 1737mochamad rizaNo ratings yet
- Clinical Relevance of Clopidogrel-Proton Pump Inhibitors InteractionDocument6 pagesClinical Relevance of Clopidogrel-Proton Pump Inhibitors InteractionLivia Maria RaduNo ratings yet
- Antiplatelet Therapy in Older Adults With Non-ST-Segment Elevation Acute Coronary Syndrome: Considering Risks and BenefitsDocument6 pagesAntiplatelet Therapy in Older Adults With Non-ST-Segment Elevation Acute Coronary Syndrome: Considering Risks and BenefitsJicko Street HooligansNo ratings yet
- Sinti Tulo 6Document1 pageSinti Tulo 6Sandra Milena Ospina HernandezNo ratings yet
- Cardiology: Nature ReviewsDocument15 pagesCardiology: Nature ReviewsluonganhsiNo ratings yet
- Platelet Glycoprotein Iib/Iiia Inhibition With Coronary Stenting For Acute Myocardial InfarctionDocument9 pagesPlatelet Glycoprotein Iib/Iiia Inhibition With Coronary Stenting For Acute Myocardial InfarctionJanuar RezkyNo ratings yet
- Adding CABG To The Dual Antiplatelet Salad: Editorial CommentDocument3 pagesAdding CABG To The Dual Antiplatelet Salad: Editorial CommentVassili CrispiNo ratings yet
- CYP450 System and Not BeingDocument5 pagesCYP450 System and Not BeingArfa'i LaksamanaNo ratings yet
- Myocard InfarctionDocument10 pagesMyocard InfarctionFelicia HoseaNo ratings yet
- Endoscopy Findings in Patients On Dual Antiplatelet Therapy Following Percutaneous Coronary InterventionDocument9 pagesEndoscopy Findings in Patients On Dual Antiplatelet Therapy Following Percutaneous Coronary InterventionsunhaolanNo ratings yet
- Duration of Dual Antiplatelet Therapy in Acute Coronary SyndromeDocument8 pagesDuration of Dual Antiplatelet Therapy in Acute Coronary SyndromeCaro GasparNo ratings yet
- Clopidogrel Withdrawal: Is There A "Rebound" Phenomenon?: Thrombosis and Haemostasis February 2011Document11 pagesClopidogrel Withdrawal: Is There A "Rebound" Phenomenon?: Thrombosis and Haemostasis February 2011Jhonatan Efrain Lopez CarbajalNo ratings yet
- DabigatranDocument12 pagesDabigatranAdityaSaskaraNo ratings yet
- Evidence-Based College of Chest Physicians: American New Antithrombotic DrugsDocument25 pagesEvidence-Based College of Chest Physicians: American New Antithrombotic DrugsDiego Fernando Escobar GarciaNo ratings yet
- Ticagrelor PDFDocument7 pagesTicagrelor PDFNurul Masyithah100% (1)
- Variability of Residual Platelet Function Despite Clopidogrel Treatment in Patients With Peripheral Arterial Occlusive DiseaseDocument6 pagesVariability of Residual Platelet Function Despite Clopidogrel Treatment in Patients With Peripheral Arterial Occlusive DiseaseGono GenieNo ratings yet
- Antithrombotic Therapy After Revascularization in Patients With Peripheral Arterial Disease: What Is Here, What Is NextDocument12 pagesAntithrombotic Therapy After Revascularization in Patients With Peripheral Arterial Disease: What Is Here, What Is NextenviNo ratings yet
- 389 FullDocument4 pages389 FullJassiel AzisNo ratings yet
- Prologhed TherapyDocument5 pagesProloghed TherapyNagatzulNo ratings yet
- PIIS0002914920313473Document9 pagesPIIS0002914920313473Luis Rafael Suárez U.No ratings yet
- 1 s2.0 S0002870316000156 MainDocument9 pages1 s2.0 S0002870316000156 MainSaid Qadaru ANo ratings yet
- Anticoagulation and Antiplatelet Therapy in Acute Coronary Syndromes (CCJM 2014)Document12 pagesAnticoagulation and Antiplatelet Therapy in Acute Coronary Syndromes (CCJM 2014)Luis Gerardo Alcalá GonzálezNo ratings yet
- Fondaparinux in Acute Coronary Syndromes CA5068 Admin OnlyDocument9 pagesFondaparinux in Acute Coronary Syndromes CA5068 Admin OnlynaeamzNo ratings yet
- Version of Record:: ManuscriptDocument23 pagesVersion of Record:: Manuscriptmiko balisiNo ratings yet
- Disminucion de Lípidos en Sindrome Coronario Agudo. Nicholls S 2018Document2 pagesDisminucion de Lípidos en Sindrome Coronario Agudo. Nicholls S 2018Tony Miguel Saba SabaNo ratings yet
- 2008.-Bleeding Risks With Pasugre.....Document3 pages2008.-Bleeding Risks With Pasugre.....tristan9454No ratings yet
- 1 s2.0 S0735109716003983 MainDocument11 pages1 s2.0 S0735109716003983 MaintopanNo ratings yet
- The Evolution of Radionanotargeting towards Clinical Precision Oncology: A Festschrift in Honor of Kalevi KairemoFrom EverandThe Evolution of Radionanotargeting towards Clinical Precision Oncology: A Festschrift in Honor of Kalevi KairemoNo ratings yet
- Prasugrel Stemi Subgroup AnalysisDocument2 pagesPrasugrel Stemi Subgroup Analysistristan9454No ratings yet
- Stroke Prevention in Atrial Fibrillation....Document3 pagesStroke Prevention in Atrial Fibrillation....tristan9454No ratings yet
- 2008.-Bleeding Risks With Pasugre.....Document3 pages2008.-Bleeding Risks With Pasugre.....tristan9454No ratings yet
- Cutaneous Blodd Filled Vesicles On IdraparinuxDocument1 pageCutaneous Blodd Filled Vesicles On Idraparinuxtristan9454No ratings yet
- 2004 OligosaccharidesDocument11 pages2004 Oligosaccharidestristan9454No ratings yet
- 2006.-Abciximab Associated Thrombocytopenia...Document5 pages2006.-Abciximab Associated Thrombocytopenia...tristan9454No ratings yet
- 2005.-Immune Thrombocytopenia Caused by Glycoprotein....Document9 pages2005.-Immune Thrombocytopenia Caused by Glycoprotein....tristan9454No ratings yet
- 2009.-First Report of Tirofiban-Induced Anemia (Found in Combination With Severe ThrombocytopeniaDocument3 pages2009.-First Report of Tirofiban-Induced Anemia (Found in Combination With Severe Thrombocytopeniatristan9454No ratings yet
- Ijcpd-15-S103 MetanalysisDocument11 pagesIjcpd-15-S103 MetanalysisGabriela ZuritaNo ratings yet
- Pyeongtaek City Foreigner GuideDocument54 pagesPyeongtaek City Foreigner Guidejoelbuxton100% (2)
- Book 1Document50 pagesBook 1Varudhini PatkiNo ratings yet
- ICTAPP 23 36 FinalVersionDocument7 pagesICTAPP 23 36 FinalVersionzobiNo ratings yet
- Full Length Research Article: ISSN: 2230-9926Document5 pagesFull Length Research Article: ISSN: 2230-9926Nisarg SutharNo ratings yet
- 675 MSDSDocument4 pages675 MSDSAhmed Emad AhmedNo ratings yet
- Research PaperDocument4 pagesResearch Paperapi-611611708No ratings yet
- Total Health Chapter 1,2 Review GameDocument123 pagesTotal Health Chapter 1,2 Review GameAlicia HigdonNo ratings yet
- CARE EMB Brief 1 - WebDocument5 pagesCARE EMB Brief 1 - WebbeckianoNo ratings yet
- Empowering Parents: AutismDocument10 pagesEmpowering Parents: AutismSuellen Concessio FernandesNo ratings yet
- 01-10-13 EditionDocument28 pages01-10-13 EditionSan Mateo Daily JournalNo ratings yet
- Nota Bene For My ReviewersDocument4 pagesNota Bene For My ReviewersYomadoNo ratings yet
- 1123 s12 in 22Document4 pages1123 s12 in 22mstudy123456No ratings yet
- Essay For TBIDocument7 pagesEssay For TBINatalie DrubachNo ratings yet
- Formula, Good or Not For The Babies ?: Written By: Rakhmah Sari Indah C. - XII P7 /28Document4 pagesFormula, Good or Not For The Babies ?: Written By: Rakhmah Sari Indah C. - XII P7 /28Inda KecilNo ratings yet
- Home Care Catalogue UK Edition 4 Web PDFDocument60 pagesHome Care Catalogue UK Edition 4 Web PDFmanuales tecnicosNo ratings yet
- Vha Class III ListingDocument2,575 pagesVha Class III ListingpvenkyNo ratings yet
- Teva AR 2017 - PharmaceuticalIndustriesLtdDocument805 pagesTeva AR 2017 - PharmaceuticalIndustriesLtdBhushanNo ratings yet
- Communication and Nutrional EducationDocument11 pagesCommunication and Nutrional EducationSabrina PanjaitanNo ratings yet
- Blended Learning 1 (Week 5)Document6 pagesBlended Learning 1 (Week 5)nurul syazwaniNo ratings yet
- Daftar Obat Untuk Formularium KlinikDocument42 pagesDaftar Obat Untuk Formularium KlinikRianda LeeNo ratings yet
- Table of Specification For Second Periodical Test in Mapeh IvDocument4 pagesTable of Specification For Second Periodical Test in Mapeh IvJENNIFER SERVONo ratings yet
- Daftar PustakaDocument5 pagesDaftar PustakaR Handi BramantoNo ratings yet
- Contractor Safety Rules PDFDocument10 pagesContractor Safety Rules PDFKEERTHI INDUSTRIESNo ratings yet
- From Sanity To Not Guilty by Reason of Insanity .The Legal FrameworkDocument18 pagesFrom Sanity To Not Guilty by Reason of Insanity .The Legal FrameworkPrecious OzigiNo ratings yet
- Lightner Witmer and The First 100 Years of Clinical PsychologyDocument4 pagesLightner Witmer and The First 100 Years of Clinical PsychologyjuaromerNo ratings yet
- NHRA-PPR - Drug Price List - 06-10-2016Document595 pagesNHRA-PPR - Drug Price List - 06-10-2016Um AbdullaNo ratings yet
- Contribution - 2019 - She Ji The Journal of Design Economics and InnovationDocument1 pageContribution - 2019 - She Ji The Journal of Design Economics and InnovationnitakuriNo ratings yet