Professional Documents
Culture Documents
Articlepdfs-Ajms v5.n4.2012 P 362-366
Uploaded by
Sergio SantosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Articlepdfs-Ajms v5.n4.2012 P 362-366
Uploaded by
Sergio SantosCopyright:
Available Formats
A l A m e e n J M e d S c i 2 0 1 2 ; 5 ( 4 ) : 3 6 2 - 3 6 6 US National Library of Medicine enlisted journal I S S N 0 9 7 4 - 1 1 4 3
ORIGINAL ARTICLE
CODEN: AAJMBG
Blood and bone marrow findings in tuberculosis in adults
-A cross sectional study
B.R. Hungund1*, S.S. Sangolli1, H.B. Bannur1, P.R. Malur1, G.S. Pilli1,
R.Y. Chavan1, S.R. Dafale1 and A.V. Joshi2
1
Department of Pathology, Jawaharlal Nehru Medical College, KLE University, Belgaum, Karnataka,
India and 2Department of Community Medicine, BIMS, Belgaum, Karnataka, India
Abstract: Background: Tuberculosis is a major public health problem in India. Hematolgical changes have
been studied with variable results. Aims and objectives: The present study was undertaken to know the
prevalence of blood and bone marrow changes in tuberculosis. Methods: The peripheral blood and bone
marrow changes were evaluated in hundred adult patients with tuberculosis, admitted at District Hospital,
Belgaum and KLES Hospital and MRC were. Results: The peripheral blood findings seen were anemia, raised
ESR, leukocytosis, neutrophilia, lymphocytosis, eosinophilia, leucopenia, thrombocytosis and thrombocytopenia. The bone marrow changes seen were hypercellularity , myeloid hyperplasia , erythroid hyperplasia with
megaloblastic changes and reactive plasmacytosis. Another interesting finding in bonemarrow was presence of
granulomas which were seen in 5% of cases of which 1 case showed positivity for acid fast bacilli on Zeihl
Neelsen stain. Conclusion: The varied hematological findings observed in tuberculosis should prompt us to
consider tuberculosis as one of the differential diagnosis in patients with hematological findings.
Keywords: Tuberculosis; Blood, Bone marrow; Granuloma., Acid fast bacilli
Introduction
Tuberculosis is a chronic bacterial infection
caused by Mycobacterium tuberculosis. This
ancient infection has plagued humans through
ages. Its elimination has remained extremely
difficult as long as poverty, over population, HIV
infection exists in large portions of earth [1]. It is
an index of social organization and standard of
living in the community [2]. Tuberculosis can
affect any organ. Lung is usual site involved. The
extra pulmonary sites involved are lymph nodes,
pleura, genitourinary tract, bones, joints,
meninges, peritoneum[3]. Today as a result of
hematogenous dissemination in HIV infection,
extra pulmonary is seen more commonly than in
the past.
Hematopoietic system is another organ seriously
affected by tuberculosis. It exerts a dazzling
variety of hematological effects involving both
cell lines and plasma components. The
hematological changes sometimes act as useful
factors providing a clue to diagnosis, assessing
the prognosis, indicating the complication of
underlying infection as well as therapy and
response to therapy [1]. The ease of availability
of blood investigations, simplicity and relative
safety of procedures, the relative low cost
factors in these investigations prompted us to
study the blood and bone marrow changes,
which may help in diagnosis and follow up of
patients with tuberculosis.
Material and Methods
This prospective study was conducted in the
department of pathology, Jawaharlal Nehru
medical college, Belgaum. The study included
100 patients more than 16years of age
admitted with the diagnosis of District
hospital and KLE societys Hospital &
Medical Research centre Belgaum from April
1st 2004 to March 31st 2005. Patients, less than
16years, with signs and symptoms of drug
toxicity due to antitubercular drugs and
having primary hematological diseases were
excluded from the study. Pertinent
information regarding the history of illness
was collected according to the questionnaire
by personal interview. A thorough clinical
examination was done and the findings were
complemented by findings in case records.
The peripheral blood was evaluated for
2012. Al Ameen Charitable Fund Trust, Bangalore
362
Al Ameen J Med Sci; Volume 5, No.4, 2012
hemoglobin, total white blood cell count,
differential count, platelet count, reticulocyte
count, peripheral smear examination and
erythrocyte sedimentation rate. Bone marrow
aspiration and trephine biopsy was performed on
all the patients. Bone marrow aspiration smears
were stained with Wrights stain and trephine
biopsy slides were stained with H&E stain. The
bone marrow aspiration and trephine biopsy
slides were also stained with Zeihl-Neelsen (ZN)
stain and screened for acid fast bacilli. For
evaluation of peripheral blood and bone marrow
findings criteria outlined by Dacie and Lewis
were used. Ethical clearance was obtained from
the institutional Ethical committee and informed
consent was obtained from all patients
participating in the study.
Results
The hundred cases were evaluated out to know
the prevalence of blood and bone marrow
Hungund BR et al
changes in tuberculosis. Out of the 100 cases,
83(83%) cases presented with pulmonary
manifestations and 17(17%) presented with
extra pulmonary manifestations. 28(28%)
cases were HIV seropositive. The peak
incidence was seen in the age group of 26 to
35years (32%). Anemia was seen in most of
the patients ie in 96(96%) cases. Majority of
them mild anemia of normocytic hypochromic
type. The WBC abnormalities included
leucocytosis in 34(34%) cases, leucopenia in
3(3%) cases, neutrophilia in 35 (35%) cases,
lymphocytosis in 6(6%) cases, lymphocytopenia in 2(2%) cases and eosinophilia in
5(5%) cases. Platelet count was normal in
majority ie in 89(89%) cases. 8(8%) cases
showed thrombocytosis and 3(3%) cases
showed thrombocytopenia. ESR was raised in
all the cases. An ESR of greater than
100mm\1hour was seen in 23(23%) cases.
[Table1].
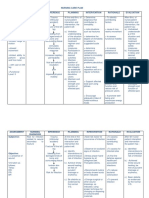
Table-1: Peripheral Blood Findings in Tuberculosis
Peripheral Blood Findings
No. of Cases
Red Blood cells
No anemia(Normal Hb ie >135g/L in males &>125g/L in females)
Mild anemia(Hb<Normal100g/L)
Moderate anemia(<100g/L & >70g/L)
Severe anemia( 70g/L)
04
50
37
09
04.00
50.00
37.00
09.00
White Blood Cells
Normal count
Leukocytosis
Leukopenia
Neutrophilia
Lymphocytosis
Lymphocytopenia
Eosinophilia
63
34
03
35
06
02
05
63.00
34.00
03.00
35.00
06.00
02.00
05.00
Platelets
Normal
Thrombocytosis
Thrombocytopenia
89
08
03
89.00
08.00
03.00
Erythrocyte Sedimentation rate
Increased
<100 mm/1hour
>100mm/1hour
100
77
23
100.00
77.00
23.00
2012. Al Ameen Charitable Fund Trust, Bangalore
363
Al Ameen J Med Sci; Volume 5, No.4, 2012
Fig-1: Bone marrow biopsy Granuloma showing
aggregation epitheloid cells (H&E; x400)
Bone marrow changes-Majority of the patients
had normocellular bone marrow. Hypercellularity of the marrow was seen in 46 (46%)
cases. 2(cases) showed hypocellularity.
Myeloid and erythroid hyperplasia was seen in
14(14%)cases and 10(10%) cases respectively.
Megaloblastic reaction was seen in 8(8%)
cases. Megakaryocytes were normal in all the
cases. Reactive plasmacytosis was seen in
Hungund BR et al
Fig-2: Bone marrow biopsy Acid fast bacilli
(arrow) in necrotic background. (ZN stain; x1000)
46(46%) cases. Granulomas [Fig1] were seen in
bone marrow biopsy in 5(5%) cases of which in
2(2%) cases they were illformed. ZN stain
revealed positivity in only one case. [Fig2] Perls
stain for iron revealed normal iron stores in
84(84%)cases, increased iron
stores
in
12(12%)cases and decreased iron stores in
only 4(4%)cases.[Table2]
Table-2: Bone Marrow Findings in Tuberculosis
Bone Marrow Findings
No. of Cases
Cellularity
Normocellular
Hypercellular
Hypocellular
52
46
02
52.00
46.00
02.00
M : E Ratio
Normal
Myeloid hyperplasia
Erythroid hyperplasia
74
14
12
74.00
14.00
12.00
Erythroid Series
Normoblastic
Megaloblastic
92
08
92.0
08.00
Myeloid Series
Normal maturation
Giant Metamyelocytes
92
08
92.00
08.00
Megakaryocytes
Normal
Increased
Depressed
100
---
100.00
---
Plasmacytosis
46
46.00
Granulomas
5.00
ZN Stain (AFB Positive)
1.00
Iron Stores
Normal
Increased
Decreased
84
12
04
84.00
12.00
04.00
2012. Al Ameen Charitable Fund Trust, Bangalore
364
Al Ameen J Med Sci; Volume 5, No.4, 2012
Hungund BR et al
Discussion
Hematological studies have been studied by
various authors in the past with varied results.
The prevalence of anemia in our study was
similar to that reported by previous studies [47]. A blunted erytropoietic response of the
bone marrow, release of TNF- and other
cytokines by tuberculosis activated monocytes
suppressing the erythropoietic production,
block in the reticuloendotheial transfer of iron
in to the nucleus of developing red cell are
also postulated as cause for anemia [1,8-9].
The occurrence of leucocytosis, neutrophilia,
lymphocytosis was similar to other studies
and are thought to be the immune responses
to tuberculosis [5,8,10-11]. The prevalence of
cytopenias was seen in lesser percentage of
cases as compared to studies done on patients
with disseminated military tuberculosis
[6,8,11]. The prevalence of thrombocytopenia
and throbocytosis was similar to earlier
studies [6,8,10]. Thrombocytosis is postulated
to be due to increased thrombopoietic factors
as a inflammatory response [1]. Varied
mechanisms like drugs immune mechanisms,
bone
marrow fibrosis,
granulomatous
involvement
of
bone
marrow
and
hypersplenism have all been put forward as
possible causal factors for thrombocytopenia
[1]. Raised ESR, which is one of the
indicators of severity of disease and a
prognostic tool, was in agreement with
previous studies [5,12].
The bone marrow findings in our study were
consistent with previous studies [6,8].
Involvement of bone marrow as suggested by
finding of granuloma and\or of acid fast bacilli in
the bone marrow were rare but interesting
findings in our study, which is consistent with
literature [13-14]. However bone marrow culture
and other molecular techniques like polymerase
chain reaction would have perhaps improved the
yield. Though varied results have been shown in
earlier studies regarding the bone marrow iron
stores, normal or increased stores are seen in
majority. Our study is in agreement with their
results. However the other iron related
measurements were not done in our study.
Literature reveals decreased serum iron, total iron
binding capacity, trasnferrin saturation and
increase in serum ferritin in patients with
tuberculosis. These abnormalities result from
redistribution of iron as a acute phase reaction.
Though the total iron stores are normal, iron is
unavailable for normal hematopoiesis and excess
non-hemic-iron is visible in the bone marrow [1].
Conclusion
Tuberculosis is one of the common infections in
this part of country affecting the most productive
age group. Hematological investigations are one
of the commonly performed investigations in
clinical practice. The varied hematological
findings observed in tuberculosis should prompt
us to consider tuberculosis as one of the
differential
diagnosis
in
patients
with
hematological findings.
Acknowledgement
I acknowledge the help of the technical staff of Department
of Pathology JNMC Belgaum during the conduct of the
study.
References
1.
2.
3.
4.
Schlossberg David. Tuberculosis and nontuberculous Mycobacterial infections. 4th Ed.
Philadelphia, Pennsyvania, United States of
America: W.B. Saunders Company; 1999.
Murray CJL, Styblok, Rouillon A. Tuberculosis in
developing countries: Burden, intervention and
cost. Bulletin International Union. Tuber Lung Dis
1990; 65:6-24.
Braunwald E, Fauci AS, Kasper DL, Hauser SL,
Longo DL, Jameson JL. Harrisons Principles of
Internal Medicine. 15th ed. International Edition:
McGraw Hill Companies Inc; 2001.
Glasser RM, Walker RI, Herion JC, Hill C. The
significance of hematological abnormalities in
5.
6.
7.
8.
patients with tuberculosis. Arch Intern Med, 1970;
125:691-695.
Morris CDW, Bird AR, Nell H. The haematological
and biochemical changes in severe pulmonary
tuberculosis. Q J Med, 1989; 272:1151-1159.
Lombard EH, Mansvelt EPG. Haematological changes
associated with miliary tuberculosis of bone marrow.
Tuber Lung Dis, 1993; 74:131-135.
Chakraborti AK, Dutta AK, Dasgupta B, Ganguli D,
Ghosal AG. Haematological changes in disseminated
tuberculosis. Indian Journal of Tuberculosis, 1995;
42:165-168.
Singh KJ, Ahluwalia G, Sharma SK, Saxena R,
Choudhary VP, Anant M. Significance of
hematological manifestations in patients with
2012. Al Ameen Charitable Fund Trust, Bangalore
365
Al Ameen J Med Sci; Volume 5, No.4, 2012
tuberculosis. J Assoc Physicians India, 2001;
49:788-794.
9. Ebrahim O, Folb PI, Robson SC, Jacobs P. Blunted
erythropoietin response to anemia in tuberculosis.
Eur J Haematol, 1995; 55:251-254.
10. Olaniyi JA, Akeuova YA. Haematological profile
in patients with pulmonary tuberculosis in Idaban
Nigeria. Afr J Med Sci, 2003; 32(3):239-242.
11. Maartens G, Willcox PA, Benator SR. Miliary
tuberculosis: Rapid diagnosis, haematologic
abnormalities, and outcome in 109 treated adults.
Am J Med 1990; 89:291-296.
Hungund BR et al
12. Deodhare SG. General Pathology and Pathology of
Systems. 6th Ed. Mumbai: Popular Prakashan Pvt. Ltd;
2002.
13. Rosenber MJ, Rumans LW. Survival of a patient with
pancytopenia and disseminated coagulation associated
with miliary tuberculosis. Chest 1978; 73:536-539.
14. Koley KC, Singh HP, Karnani I, Rao MKK. Bone
marrow in the diagnosis of fever of unknown origin: A
report of 5 cases. Indian Journal of Tuberculosis 1991;
38:163-165.
*All correspondences to: Dr Bhagyashri R Hungund, A-13/4, JNMC Staff Qtrs, Nehru Nagar, Belgaum-590010 Karnataka, India. E-mail:
drbhagyashri78_h@yahoo.co.in
2012. Al Ameen Charitable Fund Trust, Bangalore
366
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Project Report: Submitted in Partial Fulfilment of The Requirement For Post Graduate Diploma in ManagementDocument9 pagesProject Report: Submitted in Partial Fulfilment of The Requirement For Post Graduate Diploma in ManagementPiyush RajNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Agencies WebsitesDocument4 pagesAgencies WebsitesWWMTNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- How To Read A Chest X RayDocument20 pagesHow To Read A Chest X RayJasvin Sidhu100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Scott Stewarts Surviving Schizophrenia Story PDFDocument113 pagesScott Stewarts Surviving Schizophrenia Story PDFscott stewartNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Discovery 2020Document6 pagesDiscovery 2020BusinessTech100% (1)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- NR328 Sim Pre-Brief - Madison Cooper & Johnny ParkerDocument3 pagesNR328 Sim Pre-Brief - Madison Cooper & Johnny ParkerJohn MixerNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Post-Mortem ExaminationDocument7 pagesPost-Mortem ExaminationLeninRickyNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- WNSSP Estimulacion SensorialDocument3 pagesWNSSP Estimulacion Sensoriallgomezb11100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Kavita Priya Labetalol in Pih - IDocument58 pagesKavita Priya Labetalol in Pih - IKavita PriyaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- CPR PDFDocument37 pagesCPR PDFArdhi AgustjikNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- SMBG En2Document44 pagesSMBG En2Andreea GherasimNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- ST Jude at Work Pledge CardsDocument1 pageST Jude at Work Pledge CardsJamieNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- APA - DSM5 - Level 1 Measure Child Age 11 To 17 PDFDocument3 pagesAPA - DSM5 - Level 1 Measure Child Age 11 To 17 PDFdavidhoracioNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- YASASII - Nursing ManualDocument20 pagesYASASII - Nursing ManualSalma Alsheikh AbdullahNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- 46.5. Professional Services, Inc. v. CA (2008)Document10 pages46.5. Professional Services, Inc. v. CA (2008)Iñigo Mathay RojasNo ratings yet
- Hair Loss Treatment - PRP Hair Fall Treatment E-BookDocument26 pagesHair Loss Treatment - PRP Hair Fall Treatment E-BookolivaclinicNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Peripheral NeuropathiesDocument18 pagesPeripheral Neuropathiesjoanna gurtizaNo ratings yet
- Rhino-FESS Carny Procedure-Guide en 42042Document64 pagesRhino-FESS Carny Procedure-Guide en 42042Rijal SaputroNo ratings yet
- How To Guide For Measurement For ImprovementDocument20 pagesHow To Guide For Measurement For Improvementhamood1044No ratings yet
- Thyroid Eye DiseaseDocument32 pagesThyroid Eye Disease-Yohanes Firmansyah-No ratings yet
- Apollo Hospitals - Presentation (ETOP)Document24 pagesApollo Hospitals - Presentation (ETOP)p_sonera0% (1)
- Process RecordingDocument10 pagesProcess Recordingapi-318733585No ratings yet
- Goal Management Training in Adults With ADHD An Intervention StudyDocument9 pagesGoal Management Training in Adults With ADHD An Intervention StudyalilaNo ratings yet
- Nursing Practice 1Document4 pagesNursing Practice 1Nurul IzzahNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Early Onset Strep DiseaseDocument26 pagesEarly Onset Strep DiseaseKez FevNo ratings yet
- Anil Degaonkar, Nikhil Bhamare, Mandar Tilak Arterio-Enteric Fistula A Case ReportDocument6 pagesAnil Degaonkar, Nikhil Bhamare, Mandar Tilak Arterio-Enteric Fistula A Case ReportDr. Krishna N. SharmaNo ratings yet
- Pedia Notes PrintDocument6 pagesPedia Notes PrintDre Valdez100% (5)
- Estimating Glomerular Filtration RateDocument7 pagesEstimating Glomerular Filtration RateShirin SyailandiraNo ratings yet
- Nursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveDocument2 pagesNursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveDat boiNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Acteon Surgery Clinical BookletDocument56 pagesActeon Surgery Clinical BookletJTDentalGroupNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)