Professional Documents
Culture Documents
APACHEII
Uploaded by
Failasuf WibisonoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
APACHEII
Uploaded by
Failasuf WibisonoCopyright:
Available Formats
Table 2.
The APACHE II Severity of Disease Classification System
Physiologic Variable
Temperature rectal (C) Mean Arterial Pressure mm Hg Heart Rate (ventricular response) Respiratory Rate (non-ventilated or ventilated) Oxygenation: A-aDO2 or PaO2 (mm Hg) a. FIO2 0.5 record A-aDO2 b. FIO2 <0.5 record PaO2
High Abnormal Range +4 +3
41 160 180 50 500 39 to 40.9 130 to 159 140 to 179 35 to 49 350 to 499
+2
110 to 129 110 to 139
+1
38.5 to 38.9
0
36 to 38.4 70 to 109 70 to 109 12 to 24 <200 PO2>70
+1
34 to 35.9
+2
32 to 33.9 50 to 69 55 to 69 6 to 9
Low Abnormal Range +3 +4
30 to 31.9 40 to 54 29.9 49 39 5
Points
25 to 34 200 to 349
10 to 11
PO2 61 to 70 7.25 to 7.32 18 to 21.9 3 to 3.4 120 to 129 2.5 to 2.9 <0.6 20 to 29.9 1 to 2.9
PO2 55 to 60 7.15 to 7.24 15 to 17.9 111 to 119
PO2<55 <7.15 <15 110 <2.5 <20 <1
Arterial pH (preferred) 7.7 Serum HCO3 (venous mEq/l) 52 (not preferred, but may use if no ABGs) Serum Sodium (mEq/l) 180 Serum Potassium (mEq/l) 7 Serum Creatinine (mg/dl) 3.5 Double point score for acute renal failure Hematocrit (%) 60 White Blood Count (total/mm3) 40 (in 1000s) Glasgow Coma Score (GCS) Score = 15 minus actual GCS A. Total Acute Physiology Score (sum of 12 above points) B. Age points (years) 44 = 0; C. Chronic Health Points (see below)
7.6 to 7.69 41 to 51.9 160 to 179 6 to 6.9 2 to 3.4 155 to 159 1.5 to 1.9 50 to 59.9 20 to 39.9
7.5 to 7.59 32 to 40.9 150 to 154 5.5 to 5.9 46 to 49.9 15 to 19.9
7.33 to 7.49 22 to 31.9 130 to 149 3.5 to 5.4 0.6 to 1.4 30 to 45.9 3 to 14.9
45 to 54 = 2;
55 to 64 =3;
65 to 74 = 5;
75 = 6
Total APACHE II Score (add together the points from A+B+C)
Chronic Health Points: If the patient has a history of severe organ system insufficiency or is immunocompromised as defined below, assign points as follows: 5 points for nonoperative or emergency postoperative patients 2 points for elective postoperative patients Definitions: organ insufficiency or immunocompromised state must have been evident prior to this hospital admission and conform to the following criteria: Liver biopsy proven cirrhosis and documented portal hypertension; episodes of past upper GI bleeding attributed to portal hypertension; or prior episodes of hepatic failure/encephalopathy/coma. Cardiovascular New York Heart Association Class IV. Respiratory Chronic restrictive, obstructive, or vascular disease resulting in severe exercise restriction (i.e., unable to climb stairs or perform household duties; or documented chronic hypoxia, hypercapnia, secondary polycythemia, severe pulmonary hypertension (>40 mmHg), or respirator dependency. Renal receiving chronic dialysis. Immunocompromised the patient has received therapy that suppresses resistance to infection (e.g., immunosuppression, chemotherapy, radiation, long term or recent high dose steroids, or has a disease that is sufficiently advanced to suppress resistance to infection, e.g., leukemia, lymphoma, AIDS). 0 to 4 = ~4% death rate 5 to 9 = ~8% death rate
Adapted
10 to 14 = ~15% death rate 15 to 19 = ~25% death rate
Interpretation of Score: 20 to 24 = ~40% death rate 25 to 29 = ~55% death rate
30 to 34 = ~75% death rate Over 34 = ~85% death rate
from Crit Care Med 1985;13:818-829
You might also like
- Arterial Blood Gas Analysis - making it easyFrom EverandArterial Blood Gas Analysis - making it easyRating: 4.5 out of 5 stars4.5/5 (4)
- Blood Sample Normal Panic Values For Abgs: Clinical SignificanceDocument7 pagesBlood Sample Normal Panic Values For Abgs: Clinical SignificancegeonarcisoNo ratings yet
- Lab ValuesDocument6 pagesLab ValuesdnllkzaNo ratings yet
- Kay's Final FRCA NotesDocument10 pagesKay's Final FRCA Notesmyat2567% (6)
- Hypertention Urgency/emergencyDocument35 pagesHypertention Urgency/emergencyMohamad al-fazmi100% (1)
- VETS - Sheri Ross - Management of Chronic Kidney DiseaseDocument11 pagesVETS - Sheri Ross - Management of Chronic Kidney DiseaseFerrianto Diyan KusumaNo ratings yet
- Evaluation and Management of Suspected Sepsis and Septic by DR Gireesh Kumar K PDocument36 pagesEvaluation and Management of Suspected Sepsis and Septic by DR Gireesh Kumar K PSreekrishnan TrikkurNo ratings yet
- ICU Scoring Systems ExplainedDocument56 pagesICU Scoring Systems Explainedalfian sinaga100% (1)
- Essential Lists for Intercollegiate MRCS Anaesthetics and ITUDocument18 pagesEssential Lists for Intercollegiate MRCS Anaesthetics and ITUMahmoud Selim100% (1)
- Apache ScoreDocument10 pagesApache ScoreEffita PiscesianaNo ratings yet
- The APACHE II Severity of Disease Classification SystemDocument2 pagesThe APACHE II Severity of Disease Classification SystemFahmi Nur ZamanNo ratings yet
- APACHE II SCORE: ACUTE PHYSIOLOGY AND CHRONIC HEALTH EVALUATIONDocument21 pagesAPACHE II SCORE: ACUTE PHYSIOLOGY AND CHRONIC HEALTH EVALUATIONBedah Unsrat2021No ratings yet
- 210 25 Oct 2019 11 00 09Document49 pages210 25 Oct 2019 11 00 09Atul SharmaNo ratings yet
- Clinical Study: Development of Dengue Infection Severity ScoreDocument6 pagesClinical Study: Development of Dengue Infection Severity ScoreValencius SunandarNo ratings yet
- ABG TutorialDocument6 pagesABG TutorialdrazrinaNo ratings yet
- 2007 Esh Esc Guidelines SlidesetDocument72 pages2007 Esh Esc Guidelines SlidesetNevrez KoylanNo ratings yet
- APACHE II Severity of Disease Classification System ExplainedDocument2 pagesAPACHE II Severity of Disease Classification System ExplainedPipipNo ratings yet
- Sepsis Ve Septik ŞokDocument20 pagesSepsis Ve Septik Şokmohadese.hnprNo ratings yet
- HiperkolesterolDocument60 pagesHiperkolesterolAnonymous 1jCVqQuNo ratings yet
- Dengue Haemorrhagic Fever: Case ReportDocument37 pagesDengue Haemorrhagic Fever: Case ReportmhimiNo ratings yet
- CURB-65 A 7mmol (19mg/dl) BP 65: CURB-65, PSI, CPIS & AntibioticDocument3 pagesCURB-65 A 7mmol (19mg/dl) BP 65: CURB-65, PSI, CPIS & AntibioticfaberNo ratings yet
- ICU Outcome Scoring SystemsDocument15 pagesICU Outcome Scoring SystemsDrahmed AbdeljawwadNo ratings yet
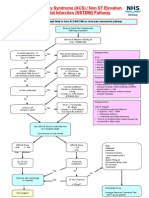
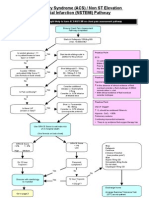
- Acs Nstemi PathwayDocument3 pagesAcs Nstemi PathwayAliey's SKeplek NgeNersNo ratings yet
- Lab Values and Vital SignsDocument4 pagesLab Values and Vital SignsWole Olaluwoye100% (1)
- NC CARDIO - RanggaDocument21 pagesNC CARDIO - RanggaRima KhairunnisaNo ratings yet
- Philippine Pediatric Society Guidelines on Screening and Managing Pediatric COVID-19 (39Document20 pagesPhilippine Pediatric Society Guidelines on Screening and Managing Pediatric COVID-19 (39Obree Mdn-RfnNo ratings yet
- The Lower Respiratory Tract Infection: Pneumonia: Ida Bagus Ngurah RaiDocument32 pagesThe Lower Respiratory Tract Infection: Pneumonia: Ida Bagus Ngurah RaiFelicia adeline ChristianNo ratings yet
- Diagnostic Criteria of Hepatorenal Syndrome (HRS)Document57 pagesDiagnostic Criteria of Hepatorenal Syndrome (HRS)shamsy100% (1)
- Pulmonary Embolism CHF NYHA IV HHD PH SevereDocument31 pagesPulmonary Embolism CHF NYHA IV HHD PH SevereNurfitrianti ArfahNo ratings yet
- COVID - 19 Diagnosis - Current Updates FinalDocument63 pagesCOVID - 19 Diagnosis - Current Updates FinalDr. Gurbilas P. SinghNo ratings yet
- Bài Giảng Cô Siripen (SXH Ngày 9.5.2018)Document64 pagesBài Giảng Cô Siripen (SXH Ngày 9.5.2018)Minh HoàngNo ratings yet
- Aetiology, Pathophysiology and Diagnosis of Dengue Infection: DR Lee Oi Wah Peg. Perubatan Ud54Document40 pagesAetiology, Pathophysiology and Diagnosis of Dengue Infection: DR Lee Oi Wah Peg. Perubatan Ud54EzraManzanoNo ratings yet
- Im Notes 1Document13 pagesIm Notes 1Celine VilloNo ratings yet
- COPD Case StudyDocument23 pagesCOPD Case StudyXinyun XuNo ratings yet
- STEMI anteroseptalDocument42 pagesSTEMI anteroseptalWarren LieNo ratings yet
- ACS NSTEMI Clinical PathwayDocument3 pagesACS NSTEMI Clinical PathwayXtiaRNo ratings yet
- Study ProtocolDocument18 pagesStudy ProtocolTirthesh PatelNo ratings yet
- Risk Factors For Severe COVID 19Document3 pagesRisk Factors For Severe COVID 19drsaleemNo ratings yet
- Brain Dump: Myotomes, Reflexes, Cranial Nerves, Lab ValuesDocument6 pagesBrain Dump: Myotomes, Reflexes, Cranial Nerves, Lab ValuesMarilia FarensenaNo ratings yet
- Hodgkin Lymphoma KlapperDocument17 pagesHodgkin Lymphoma KlapperAthika RodhyaNo ratings yet
- HLHDocument11 pagesHLHoomarNo ratings yet
- Cardiovascular Physical TherapyDocument41 pagesCardiovascular Physical TherapyNoelle Grace Ulep BaromanNo ratings yet
- Rheumatic Fever: Prof. A K M MohibullahDocument42 pagesRheumatic Fever: Prof. A K M MohibullahNavojit ChowdhuryNo ratings yet
- Exercise ECGDocument85 pagesExercise ECGLaeeq R MalikNo ratings yet
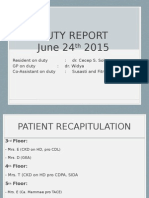
- Duty Report On Ward 24-06-15Document25 pagesDuty Report On Ward 24-06-15Annisa Rizki Ratih PratiwiNo ratings yet
- SOFA score: Organ failure assessment in ICU patientsDocument5 pagesSOFA score: Organ failure assessment in ICU patientsWiji LestariNo ratings yet
- SepsisDocument45 pagesSepsisFloriPuspaHumaniNo ratings yet
- CAP by DR SarmaDocument76 pagesCAP by DR SarmaTina ReisaNo ratings yet
- ABG Examples ABG exam questions for medical students and PACESDocument10 pagesABG Examples ABG exam questions for medical students and PACES8b8xppmgpcNo ratings yet
- How To Perform and Interpret An Exercise TestDocument48 pagesHow To Perform and Interpret An Exercise TestBilal AfridiNo ratings yet
- Acute Respiratory Distress SyndromeDocument10 pagesAcute Respiratory Distress Syndromealina abu rumiNo ratings yet
- Sepsis & SIRS: Wade Woelfle, MD, FAAEM UW ECC 2016 June 21,2016Document44 pagesSepsis & SIRS: Wade Woelfle, MD, FAAEM UW ECC 2016 June 21,2016Elavarasi GanesanNo ratings yet
- Understanding Sepsis & SIRSDocument44 pagesUnderstanding Sepsis & SIRSDaintyGarciaNo ratings yet
- Dengue FinalDocument24 pagesDengue FinalManju ManjunathNo ratings yet
- Case Presentation On Copd - Shaik NazmaDocument29 pagesCase Presentation On Copd - Shaik NazmaDeepikaNo ratings yet
- Pulmonary Emergency ٠٥٠٨٥٠Document167 pagesPulmonary Emergency ٠٥٠٨٥٠mbamuqabel1999No ratings yet
- Acute Myocardial Infarction With ST Segment ElevationDocument26 pagesAcute Myocardial Infarction With ST Segment ElevationJeane SuyantoNo ratings yet
- Covid 19/sars Cov 2Document33 pagesCovid 19/sars Cov 2Wazeed BashaNo ratings yet
- Epilogue PsDocument1 pageEpilogue PsHamid Paminto NugrohoNo ratings yet
- Ema v2n2Document1 pageEma v2n2Failasuf WibisonoNo ratings yet
- 114Document6 pages114Rajashekhar MuniswamyNo ratings yet
- Higher Algebra - Hall & KnightDocument593 pagesHigher Algebra - Hall & KnightRam Gollamudi100% (2)