Professional Documents
Culture Documents
Nursing Care Plan
Uploaded by
Jam AbantaoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Care Plan
Uploaded by
Jam AbantaoCopyright:
Available Formats
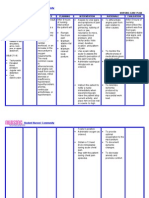
NURSING CARE PLAN Nursing Diagnosis # 1: Ineffective cerebral Tissue Perfusion related to interruption of arterial blood flow as evidenced
by presence of mass in the left parietal lobe, numbness of the right face including right side of the neck, right arm, and right side of the trunk and right side extremities. Goal: To increase and maintain normal level of oxygen. Expected Outcome: At the end of 8 hours nursing intervention, the client will be able to: 1. Verbalize understanding of condition, therapy regimen, side effects of medications, and when to contact healthcare provider. 2. Demonstrate behaviors/lifestyle changes to improve circulation (e.g., cessation of smoking, relaxation techniques, exercise/dietary program). 3. Demonstrate increased perfusion as individually appropriate (e.g., skin warm/dry, peripheral pulses present/strong, vital signs within clients normal range, alert/oriented, balanced intake/output, absence of edema, free of pain/discomfort). Interventions Evaluation Promotive: 1. Assessed the patients health condition. Rationale: to provide baseline data. 2. Monitored vital signs especially blood pressure, heart rate, respiratory rate and temperature every hour. Rationale: to note if there are any relevant changes. 3. Reviewed results of diagnostic studies (e.g., ultrasound/ CT/other imaging scans, CBC, Crea Profile, and other laboratory - Patient was seen awake, conscious,
coherent and oriented to time, place and person. - 0700H:60bpm/37.2C/ 130/90mmHg/19cpm - 0800H:72bpm/ 37.2C/ 20cpm - 0900H:68bpm/ 36.8C/ 20cpm - 1000H:70bpm/ 120/80mmHg/18cpm - 1100H:64bpm/ 110/80mmHg/20cpm - 1200H:66bpm/ 120/80mmHg/19cpm
130/80mmHg/ 110/70mmHg/ 36.6C/ 37.0C/ 37.0C/
examinations.) Rationale: to determine location/severity of condition. -
- 1300H:72bpm/ 37.1C/120/80mmHg/20cpm - 1400H:68bpm/ 37.2C/110/70mmHg/20cpm CT Scan of the brain (Feb.16,11) showed that there is no evidence of an acute intracranial hemorrhage, pneumocephalus along the left frontal convexity. - ECG(Feb.2,11) Mild Mitral Regurgitation - Ultrasound of the neck with color Doppler (Feb.10,11) showed that there has complex mass in right thyroid lobe with 10cm x 6cm x 4cm firm, non-movable mass. - CBC(Feb.23,11) high WBC 11.27x10^3/uL (4.4-11); high Segmenters 86% (40-70); low Lymphocytes 10% (22-43);low Osmolality 270mOsm/kg H2 (275-295); high cholesterol 243.56 mg/dL (<200); high HDL cholesterol 63.45 mg/dL (40-60); high ALDL 157.08 mg/dL (0-100); High alkaline phosphate 112 u/L (35-105); high fasting blood sugar 149.79 mg/dL (70110) Numbness in the right face including right side of the neck, right arm, and right side of the trunk and right side extremities. According to the husband, Lagi na lang siyang nagagalit kahit walang dahilan. Lagi nalang galit at iritable. Patient had 1 episode of blackout PTA admission.
4. Determined presence of visual, sensory/motor changes, headache, dizziness, altered mental status, personality changes. 5. Noted history of syncope, brief/intermittent periods of confusion/blackout. Rationale: Suggestive of a transient ischemic attack (TIA). 6. Assisted with treatment of underlying conditions (e.g., surgical reperfusion procedures, medications, fluid replacement/rehydration, nutrients, treatment of sepsis, etc.), as indicated.
Rationale: to improve tissue perfusion/organ function. 7. Encouraged use of relaxation activities, exercises/techniques. 8. Established/ encouraged regular exercise program. Rationale: to decrease tension level 9. Measured intake and output accurately. Rationale: to determine if there is possible occurrence of fluid overload. Preventive: 10. Reviewed specific dietary changes/restrictions with client (e.g., reduction of cholesterol and triglycerides, high or low protein intake). 11. Identified necessary changes in lifestyle and assisted client to incorporate disease management into ADLs. 12. Elevated HOB (e.g., 30 degrees) and maintain head/neck in midline or neutral position Rationale: to promote circulation/venous drainage and to decrease blood flow for Patient verbalized understanding that she needs assistance when walking or transferring from one place to another. Low fat, low salt with Diabetic Specified plus 1 banana per meal. Intake of 890 mL and Output of 6 urine and no stool. Patient has a regular schedule with physical therapy every AM. Patient was seen listening to music. 1) PNSS1L x 10hours 25 gtts/min 2) PLRS1L x 10hours 25 gtts/min
possible increase intracranial pressure. Curative: 13. Assisted in administer medications (e.g., antihypertensive agents, steroids/diuretics [may be used to decrease edema], anticoagulants). Maintained on HOB 30 until 1400H.
Patient was able to tolerate the medications given.
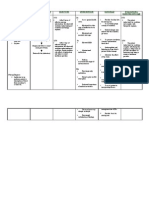
NURSING CARE PLAN Nursing Diagnosis # 2: Impaired physical Mobility may be related to neuromuscular involvement as evidenced by numbness of the right leg. Goal: To strengthen the affected area. ( right leg ) Expected Outcome: At the end of 8 hours nursing intervention, the client will be able to: 1. Verbalize understanding of situation and individual treatment regimen and safety measures. 2. Demonstrate techniques/behaviors that enable resumption of activities. 3. Maintain or increase strength and function of affected and/or compensatory body part. Interventions Evaluation Promotive: 1. Noted decreased motor agility/essential tremor related to age. 2. Determined degree of perceptual/cognitive impairment and ability to follow directions. 3. Assessed nutritional status and clients report of energy level. 4. Assessed degree of pain, listening to clients description. Patient cannot move her right leg and cannot dangle her right foot. the patient was able to recalled 3/3 words given, oriented to three spheres and was able to follow different directions given. The patient has a good appetite and can consume all the food served. No pain was reported.
5. Noted emotional/behavioral responses to problems of immobility. Feelings of frustration/powerlessness may impede attainment of goals. 6. Supported affected body parts/joints using
Patient was seen determined to move her affected leg.
pillows/rolls, foot supports/shoes, air mattress, water bed, and so forth. Rationale: to maintain position of function and reduce risk of pressure ulcers. 7. Scheduled activities with adequate rest periods during the day. Rationale: to reduce fatigue. 8. Encouraged participation in self-care, occupational/diversional/recreational activities. Rationale: Enhances self-concept and sense of independence. 9. Encouraged adequate intake of fluids/nutritious foods. Rationale: Promotes well-being and maximizes energy production. 10. Instructed to perform passive ROM in the -
One pillow was placed under the affected leg.
Patient was able to rest and there was no discomforts noted.
Patient reported that she was able to do passive ROM to the affected side alone.
Showed compliance to the diet prescribed. (Low fat, low salt with Diabetic Specified plus 1 banana per meal)
During the last day that the patient was handled by the student nurses, the affected
affected area.
leg was able to move from side to side, up and down. She was able to dangled her foot without difficulties. The patient used the side rails, which was kept up, to turn from sides.
Preventive: 1. Instructed in use of side rails, overhead trapeze, roller pads. Rationale: for position changes/transfers.
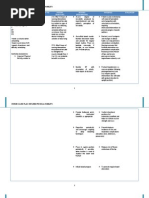
NURSING CARE PLAN Nursing Diagnosis # 3: Risk for Fall related to decrease muscle strength in the lower extremity (right leg). Goal: To prevent falls. Expected Outcome: At the end of 8 hours nursing intervention, the client will be able to: 1. Verbalize understanding of individual risk factors that contribute to possibility of falls. 2. Demonstrate behaviours, lifestyle changes to reduce risk factors and protect self from injury. 3. Modify environment as indicated to enhance safety. 4. Be free of injury. Interventions Promotive: 1. Observe individuals general health status. Rationale: noticing factors that might affect safety, such as chronic or debilitating conditions, use of multiple medications, recent trauma. 2. Assess muscle strength, gross and fine motor coordination. 3. Review history of past or current physical injuries (e.g., musculoskeletal injuries; orthopedic surgery) altering coordination, gait, and balance. All other muscle areas are 5/5, except for the lower leg 3/5. S/P Left parietal craniotomy tumor - Patient Evaluation was seen awake, conscious,
coherent and oriented to time, place and person.
excision under image guidance.
4. Review history of prior falls associated with immobility, weakness, prolonged bedrest, sedentary lifestyle (changes in body due to disuse). Rationale: unsafe environment to predict current risk for falls. 5. Evaluate use/misuse/failure to use assistive aids, when indicated. Rationale: Client may have assistive device, but is at high risk for falls while adjusting to altered body state and use of unfamiliar device; or might refuse to use devices for various reasons (e.g., waiting for help; perception of weakness) 6. Kept side rails up. 7. Instructed patient to call for assistance if needed. No fall noted. Patient verbalized understanding about the importance of having an assistance when moving. Patient was trying to stand from the wheelchair to transfer to bed alone. No history of fall.
You might also like
- NCPDocument4 pagesNCPDaniel Garraton0% (1)
- NCP CHFDocument10 pagesNCP CHFMykel Jake VasquezNo ratings yet
- NCP Ineffective Tissue Perfusion and Self Care DeficitDocument5 pagesNCP Ineffective Tissue Perfusion and Self Care DeficitFrances Anne Pasiliao100% (3)
- Risk For Decreased Cardiac OutputDocument3 pagesRisk For Decreased Cardiac OutputSid Artemis FriasNo ratings yet
- Ineffective Tissue PerfusionDocument2 pagesIneffective Tissue PerfusionDiane ReyNo ratings yet
- Self Care DeficitDocument4 pagesSelf Care DeficitEllaine RamirezNo ratings yet
- 14 Cerebrovascular Accident Nursing Care PlansDocument5 pages14 Cerebrovascular Accident Nursing Care PlansNickesha Mckenzie75% (4)
- CVA Activity IntoleranceDocument1 pageCVA Activity IntoleranceNursesLabs.com75% (4)
- Week 10 Drug Card - Hydrochlorothiazide (HCTZ)Document2 pagesWeek 10 Drug Card - Hydrochlorothiazide (HCTZ)RCurry09No ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanJayalakshmi David50% (2)
- Impaired Tissue IntegrityDocument2 pagesImpaired Tissue IntegrityJacoJone11100% (1)
- NCP For CHF 3 Activity IntoleranceDocument2 pagesNCP For CHF 3 Activity IntoleranceAngelyn ArdinesNo ratings yet
- NCP-Ineffective Cerebral Tissue PerfusionDocument9 pagesNCP-Ineffective Cerebral Tissue PerfusionKarel LuNo ratings yet
- Concept Map of Nasal ObstructionDocument2 pagesConcept Map of Nasal ObstructionChad Viajar100% (1)
- NCP Heart FailureDocument11 pagesNCP Heart FailureaZhermAine100% (1)
- Ncp-Ineffective Airway ClearanceDocument3 pagesNcp-Ineffective Airway Clearancelouanne0550% (2)
- NCP AnginaDocument3 pagesNCP AnginaShie LA100% (1)
- 1 Ineffective Breathing PatternDocument8 pages1 Ineffective Breathing PatternNoel MontemayorNo ratings yet
- NCP Inffective Tissue PerfusionDocument3 pagesNCP Inffective Tissue PerfusionPaul Cubacub0% (1)
- ANDAYA, Kristine Alexis L. BSN218 Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument3 pagesANDAYA, Kristine Alexis L. BSN218 Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationAlexis TineNo ratings yet
- End of Life - Hospice CareDocument9 pagesEnd of Life - Hospice Caremardsz100% (1)
- NCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPDocument2 pagesNCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPpa3kmedina100% (1)
- Impaired Verbal CommunicationDocument6 pagesImpaired Verbal CommunicationLaura Sansonetti100% (1)
- NCP Impaired Gas Exhange CHEST INJURYDocument4 pagesNCP Impaired Gas Exhange CHEST INJURYMa. Elaine Carla Tating100% (2)
- NCP AneurysmDocument4 pagesNCP AneurysmJanielle Christine Monsalud100% (1)
- Nursing Care PlanDocument12 pagesNursing Care Plankeishaaa29100% (6)
- NCP IschemicDocument19 pagesNCP IschemicChristina Espiña EjercitoNo ratings yet
- Postoperative Care PlanDocument4 pagesPostoperative Care Plannittin006100% (1)
- Stroke Nursing Care PlanDocument1 pageStroke Nursing Care PlanTracy PearlNo ratings yet
- Ineffective Tissue PerfusionDocument1 pageIneffective Tissue PerfusionEm Castillo50% (2)
- Decrease Cardiac OutputDocument6 pagesDecrease Cardiac OutputGerardeanne ReposarNo ratings yet
- Nursing Care PlanDocument10 pagesNursing Care PlanZerica Andaca83% (6)
- Ncp-Ineffective Tissue Perfusion (Aortic Stenosis)Document2 pagesNcp-Ineffective Tissue Perfusion (Aortic Stenosis)Daniel Vergara Arce67% (3)
- NCP - Tissue Perfusion (Cerebral)Document2 pagesNCP - Tissue Perfusion (Cerebral)moodlayers50% (6)
- Nursing Care Plan: by The Wife During InterviewDocument3 pagesNursing Care Plan: by The Wife During InterviewJayson SamonteNo ratings yet
- Risk For Impaired SwallowingDocument3 pagesRisk For Impaired SwallowingCalimlim Kim100% (1)
- NCPDocument3 pagesNCPJezza RequilmeNo ratings yet
- NCP - Patient With Endotracheal TubeDocument1 pageNCP - Patient With Endotracheal TubeSelwynVillamorPatenteNo ratings yet
- Nursing Care PlanDocument22 pagesNursing Care PlanjamNo ratings yet
- Cva NCPDocument2 pagesCva NCPAkima Mulok0% (1)
- NCP LocDocument2 pagesNCP LocMel RodolfoNo ratings yet
- Cues Nursing Diagnosis Scientific Rationale Goals Nursing Interventions Rationale EvaluationDocument3 pagesCues Nursing Diagnosis Scientific Rationale Goals Nursing Interventions Rationale EvaluationIngrid Nicolas100% (1)
- 20Document24 pages20Jeremee John Pingco50% (2)
- NCP LymphedemaDocument1 pageNCP Lymphedemayasira50% (2)
- NCP Tissue PerfusionDocument4 pagesNCP Tissue PerfusionLisa Tandog100% (1)
- NCP Acute PainDocument3 pagesNCP Acute PainDyanne BNo ratings yet
- NCPDocument8 pagesNCPJose Benit DelacruzNo ratings yet
- Activity Intolerance NCPDocument7 pagesActivity Intolerance NCPMariquita BuenafeNo ratings yet
- NCPDocument17 pagesNCPShayne Jessemae AlmarioNo ratings yet
- Assessment Needs Nursing Diagnos IS Goal/Obj Ective Intervention Rationale EvaluationDocument10 pagesAssessment Needs Nursing Diagnos IS Goal/Obj Ective Intervention Rationale EvaluationApol Pen67% (3)
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument4 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationJhoizel VenusNo ratings yet
- NCP OsteomyelitisDocument3 pagesNCP OsteomyelitisClariss Alota100% (2)
- NCP For FractureDocument2 pagesNCP For FractureArnie Jude Carido100% (1)
- Nursing Care Plan - MergedDocument13 pagesNursing Care Plan - MergedJuls Flares SycaycoNo ratings yet
- CS NCPDocument3 pagesCS NCPAllan VillanuevaNo ratings yet
- PT Protocol - Part3-IcuDocument12 pagesPT Protocol - Part3-IcuBlake BoggenpoelNo ratings yet
- Conceptmaptext For EpDocument9 pagesConceptmaptext For Epapi-272402391No ratings yet
- DIABETES Nursing ManagementDocument11 pagesDIABETES Nursing ManagementKaloy KamaoNo ratings yet
- LCPDDocument7 pagesLCPDakoismeNo ratings yet
- NCP For Impaired MobilityDocument4 pagesNCP For Impaired MobilityBettinaFernandoNo ratings yet
- Final For Net English M Oh FW 040222Document466 pagesFinal For Net English M Oh FW 040222Abdullah100% (1)
- Project #1-Caregiver's BrochureDocument2 pagesProject #1-Caregiver's BrochureswarnaNo ratings yet
- Antenatal and Intrapartum CareDocument22 pagesAntenatal and Intrapartum Caresanjay vigneshNo ratings yet
- Health FinancingDocument3 pagesHealth Financingtokobuttwer2No ratings yet
- Math and You Chapter 4 PDFDocument50 pagesMath and You Chapter 4 PDFChelsea RoseNo ratings yet
- Soal Utbk New 1Document8 pagesSoal Utbk New 1aldoilham80No ratings yet
- Presentation 4Document26 pagesPresentation 4sai projectNo ratings yet
- Preston Test 3Document4 pagesPreston Test 3Aleksandra StasiakNo ratings yet
- 1st Aid WorkbookDocument114 pages1st Aid WorkbookMichele De BiaggioNo ratings yet
- International Immunopharmacology: Hyun Jee Han, Chinekwu Nwagwu, Obumneme Anyim, Chinedu Ekweremadu, San KimDocument11 pagesInternational Immunopharmacology: Hyun Jee Han, Chinekwu Nwagwu, Obumneme Anyim, Chinedu Ekweremadu, San KimyoshefarieNo ratings yet
- Sample Email For Leave Request To ManagerDocument19 pagesSample Email For Leave Request To Managersaikiran eligetiNo ratings yet
- Teori Dekubitus - 1 PDFDocument9 pagesTeori Dekubitus - 1 PDFRudianto AhmadNo ratings yet
- ANNEX B - LGU Information SheetDocument2 pagesANNEX B - LGU Information SheetToni Quitalig GamezNo ratings yet
- Comparison of Cyclooxygenase (Cox-1 and Cox-2) EnzymesDocument11 pagesComparison of Cyclooxygenase (Cox-1 and Cox-2) EnzymesCyberLifeNo ratings yet
- Differences Between DSM 5 and DSMDocument3 pagesDifferences Between DSM 5 and DSMmomina sarwarNo ratings yet
- Acute Inflammation of Abdominal TigerDocument100 pagesAcute Inflammation of Abdominal TigerJu Lie AnnNo ratings yet
- JMSCR Vol - 07 - Issue - 08 - Page 294-297 - August: Use of Polyetylene Glycolenema in Patients On Hemodialysis PatientsDocument4 pagesJMSCR Vol - 07 - Issue - 08 - Page 294-297 - August: Use of Polyetylene Glycolenema in Patients On Hemodialysis PatientsJaydeep VayedaNo ratings yet
- Constipation in ChildhoodDocument10 pagesConstipation in Childhoodadkhiatul muslihatinNo ratings yet
- Bacote BOP ComplaintDocument160 pagesBacote BOP ComplaintEthan BrownNo ratings yet
- YH Neonatal Paediatric Hyperammonaemia GuidelineDocument9 pagesYH Neonatal Paediatric Hyperammonaemia GuidelineTrishenth FonsekaNo ratings yet
- PAPER 3 - Ergonomic Risk Assessment at WorkplaceDocument54 pagesPAPER 3 - Ergonomic Risk Assessment at WorkplaceSanjiv KumarNo ratings yet
- Pediatric Pain Management: Avni M. Bhalakia M.D. St. Barnabas HospitalDocument57 pagesPediatric Pain Management: Avni M. Bhalakia M.D. St. Barnabas HospitalNurul HasanNo ratings yet
- Nails in Nutritional DefinciesDocument5 pagesNails in Nutritional DefinciesstcerieNo ratings yet
- PN Comprehensive Practice A Anad B Questions and Answers VerifiedDocument8 pagesPN Comprehensive Practice A Anad B Questions and Answers Verifiedianshirow834No ratings yet
- Community Health Nursing Study GuideDocument9 pagesCommunity Health Nursing Study Guidejanedoe48792% (13)
- MM Scope EvolutionDocument53 pagesMM Scope EvolutionSai RevanthNo ratings yet
- Prescription of CRRT: A Pathway To Optimize Therapy: Review Open AccessDocument10 pagesPrescription of CRRT: A Pathway To Optimize Therapy: Review Open AccessMaritza Soto LimoNo ratings yet
- VPT 411 Veterinary Chemotherapy Tanuvas Lecture NotesDocument94 pagesVPT 411 Veterinary Chemotherapy Tanuvas Lecture NotesSunil100% (41)
- Results of HSRC Study On South African Healthcare Workers Mental Health and Covid 19Document64 pagesResults of HSRC Study On South African Healthcare Workers Mental Health and Covid 19Laura Lopez GonzalezNo ratings yet
- Interview: Patient HistoryDocument8 pagesInterview: Patient HistoryquelspectacleNo ratings yet