Professional Documents
Culture Documents
Cholelithiasis Brief Discussion
Cholelithiasis Brief Discussion
Uploaded by
Akatsuki KisameOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cholelithiasis Brief Discussion
Cholelithiasis Brief Discussion
Uploaded by
Akatsuki KisameCopyright:
Available Formats
CHOLELITHIASIS
DEFINITION Calculi, or gallstones, usually form in the gallbladder from the solid constituents of bile and vary greatly in size, shape, and composition. - Smeltzer, S.C., Bare, B.G. Brunner & suddarths Textbook of Mecial-Surgical Nursing !0th Edition. Stones on the gallbladder or biliary tree are referred to collectively as cholelithiasis. Most patients have multiple stones, sometimes several dozen. Most gallstones (80%) are cholesterol gallstones, which form when bile becomes oversaturated with cholesterol. Pigment gallstones, accounting for the remaining 20% of gallstones are composed of bilirubin and bile substances other than cholesterol. - McConnell, T. H., The Nature of Disease Pathology for the Health Professions. 2007 Gallstones are hard, pebble-like deposits that form inside the gallbladder. Gallstones may be as small as a grain of sand or as large as a golf ball, depending on how long they have been forming. - http://www.nlm.nih.gov/medlineplus/ency/article/000273.htm ANATOMY AND PHYSIOLOGY Gastroinstestinal Tract The gastrointestinal tract (GIT) consists of a hollow muscular tube starting from the oral cavity, where food enters the mouth, continuing through the pharynx, esophagus, stomach and intestines to the rectum and anus, where food is expelled. There are various accessory organs that assist the tract by secreting enzymes to help break down food into its component nutrients. Thus the salivary glands, liver, pancreas and gall bladder have important functions in the digestive system. Food is propelled along the length of the GIT by peristaltic movements of the muscular walls. The primary purpose of the gastrointestinal tract is to break down food into nutrients, which can be absorbed into the body to provide energy. Focus: GALLBLADDER The gallbladder (or cholecyst, sometimes gall bladder) is a small organ whose function in the body is to harbor bile and aid in the digestive process. Anatomy The cystic duct connects the gall bladder to the common hepatic duct to form the common bile duct. The common bile romero duct then joins the pancreatic duct, and enters through the hepatopancreatic ampulla at the major duodenal papilla. The fundus of the gallbladder is the part farthest from the duct, located by the lower border of the liver. It is at the same level as the transpyloric plane. Microscopic anatomy The different layers of the gallbladder are as follows: The gallbladder has a simple columnar epithelial lining characterized by recesses called Aschoff's recesses, which are pouches inside the lining. Under the epithelium there is a layer of connective tissue (lamina propria). Beneath the connective tissue is a wall of smooth muscle (muscularis externa) that contracts in response to cholecystokinin, a peptide hormone secreted by the duodenum. There is essentially no submucosa separating the connective tissue from serosa and adventitia. Size and Location of the Gallbladder The gallbladder is a hollow, pear-shaped sac from 7 to 10 cm (3-4 inches) long and 3 cm broad at its widest point. It consists of a fundus, body and neck. It can hold 30 to 50 ml of bile. It lies on the undersurface of the livers right lobe and is attached there by areolar connective tissue. Structure of the Gallbladder Serous, muscular, and mucous layers compose the wall of the gallbladder. The mucosal lining is arranged in folds called rugae, similar in structure to those of the stomach. Function of the Gallbladder The gallbladder stores bile that enters it by way of the hepatic and cystic ducts. During this time the gallbladder concentrates bile fivefold to tenfold. Then later, when digestion occurs in the stomach and intestines, the gallbladder contracts, ejecting the concentrated bile into the duodenum. Jaundice a yellow discoloration of the skin and mucosa, results when obstruction of bile flow into the duodenum occurs. Bile is thereby denied its normal exit from the body in the feces. Instead, it is absorbed into the blood, and an excess of bile pigments with a yellow hue enters the blood and is deposited in the tissues. The gallbladder stores about 50 mL (1.7 US fluid ounces / 1.8 Imperial fluid ounces) of bile, which is released when food containing fat enters the digestive tract, stimulating the secretion of cholecystokinin (CCK). The bile, produced in the liver, emulsifies fats and neutralizes acids in partly digested food. After being stored in the gallbladder the bile becomes more concentrated than when it left the liver, increasing its potency and intensifying its effect on fats. Most digestion occurs in the duodenum.
ETIOLOGY Predisposing Factors Age (40 and above) Gender Justification Most internal functions decline as one ages. Inevitably resulting in organ degeneration which also affects the body's metabolism of lipids. Gallstones is more frequent on women especially who had have had multiple pregnancies or who are taking oral contraceptives. Increase level of Estrogen reduces the synthesis of bile acid in women. Female sex hormones have long been suspected to have a side effect of gallstone formation by altering respective bile constituents (mainly the FAT metabolism). People who have disease of the terminal ileum or who have undergone resection of the terminal ileum deplete their bile salt pool and run a greater risk of developing cholesterol gallstones. Cholesterol stones are common in Northern Europe and in North and South America. Most clinicians have an impression that gallbladder disease characterizes some families. Indeed, the younger sisters of women with gallstone prove to have bile more highly saturated with cholesterol than the younger sisters of women without gallstones, all of which suggests that Cholelithiasis does run in families. Inflammation or infection in the biliary structures may provide a focus for stone formation or may alter the solubility of the constituents, fostering the development of a stone. In cirrhosis, at least two fifths of patients have gallstones. One possible mechanism behind the appearance of pigment softness, so far unproven, is the excretion of unconjugated bilirubin directly into the bile, something that might happen in patient with hemolysis or in the cirrhotic with his high incidence of pigment stones, currently estimated at 27 %. Brown pigment gallstones form when there is stasis of bile (decreased flow), for example, when there are narrow, obstructed bile ducts. Justification Excessive intake of high fat or cholesterol food such as pork meat, animal skin (e.g. chicharon and chicken skin) can result to an increase in cholesterol level in the body, making it hard for the liver to make bile enough to metabolized the all cholesterol present. Excess cholesterol present builds up and increases the cholesterol serum level. Normal Liver function would then try to compensate and excrete excess cholesterol to the bile plus the body would reabsorb water from the bile making it more concentrated. Supersaturation of Cholesterol along with other constituents of the bile (bilirubin, lecithin etc.) builds up microcrystals. When microcrystals aggregate it would result to Gallstones. Weight loss is associated with an increased risk of gallstones because weight loss increases bile cholesterol supersaturation, enhances cholesterol crystal nucleation, and decreases gallbladder contractility. Obesity is a major risk factor for gallstones, especially in women. A large clinical study showed that being even moderately overweight increases the risk for developing gallstones. The most likely reason is that obesity tends to reduce the amount of bile salts in bile, resulting in more cholesterol. Obesity also decreases gallbladder emptying. Altered physiology of the biliary system during pregnancy may play a role in accelerating the formation of stones in susceptible women. The contraceptive pill not only promotes thromobphlebitis but points to an endocrine background of gallstones by the risk of gallstones in young women taking the pill. This is largely as a result of increased cholesterol secretion into the bile and a decrease in chenodeoxycholic acid content, along with impaired emptying of the gallbladder brought about by estrogen. Starvation decreases gallbladder movement causing the bile to become overconcentrated with cholesterol. The liver also secretes extra cholesterol into bile adding to the supersaturation causing stone formation. Also, fasting persons have a diminished bile salt pool and lithogenic bile.Gallbladder stasis plays a key role in permitting stone formation. Defective or infrequent gallbladder emptying occurs in the settings of prolonged fasting, rapid weight loss, pregnancy, and spinal cord injury. Drugs that lower the serum level of cholesterol, notably clofibrate, are associated with an increased incidence of gallstones. Clofibrate presumably increases the secretion of cholesterol into the bile and apparently also decreases bile acid synthesis, so increasing the cholesterol saturation of the bile. Clinical reflection of these physiologic abnormalities has been found in the overwhelming association between clofibrate therapy and gallstones.
Ileal Disease/Resection Race Genetics
Inflammation and infection of the gallbladderHemolytic Disease and Hepatic Cirrhosis Bile stasis Precipitating Factors Faulty Diet
Weight Loss Obesity
Pregnancy Treatment with estrogen/ contraceptives
Frequent Starvation and Prolonged parenteral nutrition
Clofibrate use and other Antilipemic drugs
SYMPTOMATOLOGY
SIGNS AND SYMPTOMS Jaundice
JUSTIFICATION Jaundice results from an abnormally high accumulation of bilirubin in the blood as a result of which there is a yellowish discoloration to the skin and deep tissues. Jaundice becomes evident when the serum bilirubin level rises above 2.0 to 2.5 mg/dL. Bilirubin together with cholesterol is normally absorbed in the intestines and is usually excreted within the feces. The bile gives the stool its brown to black color. Obstruction in the bile flow lessens and may hinder the absorption of bile in the intestines making the stool pale in color. Normally urine are not dark in color, excess bilirubin are excreted by the kidneys as a compensatory mechanism to balance the bile level in the body. Prutitus is the most common presenting symptom in persons with cholestasis, probably related to an elevation in plasma bile acids Due to the gallstones and microcrystals present inside the gall bladder, the gallbladder can't contract properly which creates pain in the epigastric area (right side of the abdominal area), often with reffered pain, above the waist , the right shoulder and the right scapula or the midscapular region. -A gallstone produces visceral pain by obstructing the cystic duct or ampulla of Vater, resulting in distention of the gallbladder or biliary tree Less or absence of bile acid in the doudenum means less or no digestion of fats.
Pale Stool
Dark Urine Pruritus or generalized itching
Pain
Epigastric Distress Nausea & Vomiting Fullness Indigestion Increased bilirubin in the blood Vitamin deficiencies
When gallstones obstruct the bile going to the intestine, bilirubin tends to return the bodys circulation. Obstruction of bile flow also interferes with absorption of the fat-soluble vitamins A, D, E & K. Therefore the patient may exhibit deficiencies of these vitamins if biliary obstruction has been prolonged
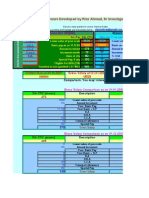
SCHEMATIC DIAGRAM
Predisposing Factors: Advanced Age Gender Ileal Resection/Disease Race Genetics
Precipitating Factors: Obesity/ Overweight Pregnancy/ Contraception Frequent Starvation, total parenteral nutrition Clofibrate Use Diet/ Weight loss
(Cholesterol Stones)
Decreased level of Bile Acids
Increased levels of fat in the blood stream
Synthesis of cholesterol in the liver
Excretion of cholesterol to the bile
Ratio of bile salts & lecithin with cholesterol is no longer within the area of solubility
Cholesterol concentration > solubility capacity of the bile
No formation of mixed miccelles
Lithogenic bile/ supersaturated bile (creamy)
Mucoprecipitates of organic& inorganic calcium salts become nucleation sites
Nucleation and production of cholesterol monohydrate crystals
Large Cholesterol Stones
Extrusion of stones from Gallbladder
Impaction at cystic and bile duct
Distention of biliary tree and fundus of gallbladder
Bile not excreted to doudenum Backflow of bile and goes to the circulation
Forceful contractions of gallbladder
levels of bilirubin/bile pigments in the circulation
Spasm of smooth muscle in the ducts
conversion of bilirubin to urobilinogen in the intestines
Fat not emulsified
No absorption of fat in the intestines
PAIN
Renal secretion of bilirubin
excretion of urobilinogen in stool
Obstructiv e Jaundice Pruritus
Grayish stool
Dark urine
Nausea and Vomiting Fullnes Indigestion Vit. ADEK defeciences
DIAGNOSTIC TESTS Laboratory Studies
The workup of cholelithiasis in pediatric patients is similar to that in adults. The goal is to demonstrate evidence of gall bladder or biliary tract disease. Liver function test (LFT) and CBC results are typically within reference ranges. Abnormalities suggest infection or obstruction, or both. All laboratory results in simple cholelithiasis should be within reference ranges. They are of use in identifying a more complex disease process, including biliary obstruction and cholecystitis. Imaging Studies
Use of kidney-ureter-bladder (KUB) plain radiography in these patients is often fruitless because many stones are not visible. However, it may be beneficial in identifying small-bowel obstruction or free air under the diaphragm. Ultrasonography of the right upper quadrant (RUQ) is the study of choice for these patients. Ultrasonography can be used to identify the location of the stone, gallbladder wall thickening, and pericholecystic fluid, and a sonographic Murphy sign aids in diagnosis of the disease process. Radionuclide scanning, such as scanning with iminodiacetic acid (IDA) derivatives (eg, hepatoiminodiacetic acid [HIDA], diisopropyl iminodiacetic acid [DISIDA], and para -isopropyliminodiacetic acid [PIPIDA] scanning), are also used to assess gall bladder function, its ability to harbor and concentrate bile, and perhaps more importantly, its motility response to cholecystokinin or a fatty meal by quantifying the ejection fraction. In children with suspected hepatobiliary complications, magnetic resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangiopancreatography (ERCP) can help delineate the anatomy of the extrahepatic and intrahepatic biliary tract, identify the presence of ductal stones, and provide a therapeutic mode of removing a stone or decompressing the biliary tract. ERCP in the pediatric population has been associated with the same frequency of success and complications as in adults. As a noninvasive alternative, the MRCP has demonstrated promise in the evaluation of choledocholithiasis but is less available at many institutions.
TREATMENT Medical Care
One option for nonsurgical management of gallstone disease is the use of ursodeoxycholic acid. One study demonstrated a 56% reduction in biliary pain after 3 months of therapy and a mean dissolution of gallstones in 59% of cases after 12 months of treatment with 10 mg/kg/d of ursodeoxycholic acid. The primary disadvantage with this approach is the incidence of recurrent gallstones, approximately 25% within 5 years. The nonsurgical option is currently only indicated for patients either unfit or unwilling to undergo surgical intervention and has not been recommended in the pediatric population. Extracorporeal shock-wave lithotripsy- repeated shock waves directed at the gallbladder or common bile duct to fragment the stones Intracorporeal shock-wave lithotripsy- fragmentation by ultrasound, pulsed laser, or hydraulic lithotripsy applied through an endoscope directly to the stones Surgical Care
Laparoscopic cholecystectomies are now being routinely performed through a small incision or puncture made through the abdominal wall in the umbilicus. Laparoscopic cholecystectomy with intraoperative cholangiography has demonstrated promise as an alternative to ERCP in patients with obstructive common bile duct stones (choledocholithiasis). Cholecystectomy gallbladder removal after the ligation oaf the cystic duct and artery Choledochostomy- incision into the common duct for stone removal Cholecystostomy- gallbladder is opened and the stone, bile, or purulent drainage is removed Diet
A decrease in the consumption of fatty foods and controlled reduction in weight Activity Leitzmann et al have demonstrated in a prospective cohort study that symptomatic gallstones in men were reduced by approximately 20% with increased exercise. This reduction may be extrapolated to the pediatric population.
MEDICATIONS Gallstone solubilizers These agents are indicated for the treatment of radiolucent noncalcified gallbladder stones. 1. Ursodiol (Actigall, Ursodamor, Ursofalk, Ursogal) Also called ursodeoxycholic acid. Indicated for radiolucent noncalcified gallbladder stones <20 mm in diameter when conditions preclude cholecystectomy. Suppresses hepatic cholesterol synthesis and secretion and also inhibits intestinal absorption. It appears to have little inhibitory effect on synthesis and secretion into bile of endogenous bile acids and does not appear to affect secretion of phospholipids into bile. After repeated doses, reaches steady-state bile concentrations in about 3 wk. Cholesterol is insoluble in aqueous media, but it can be solubilized in at least 2 different ways in the presence of dihydroxy bile acids. In addition to solubilizing cholesterol in micelles, ursodiol acts by dispersing cholesterol as liquid crystals in aqueous media. The overall effect of ursodiol is to increase the concentration level at which saturation of cholesterol occurs. The various actions of ursodiol combine to change the bile of patients with gallstones from cholesterol-precipitating to cholesterol-solubilizing bile, thus resulting in bile conducive to cholesterol stones dissolution. Although not approved by the FDA, ursodiol has been used in combination with chenodeoxycholic acid and in conjunction with extracorporeal shock-wave lithotripsy for the dissolution of gallstones. Available in 250-mg and 300-mg caps. An extemporaneous liquid formulation may be compounded for pediatric use. Anti-inflammatory agents These agents decrease inflammatory responses and systemically interfere with events leading to inflammation. Diclofenac (Voltaren, Cataflam) Designated chemically as 2-[(2,6-dichlorophenyl) amino] benzene acetic acid, monosodium salt, with an empirical formula of C14 H10 Cl2 NO2 NA. One of a series of phenylacetic acids that has demonstrated anti-inflammatory and analgesic properties in pharmacological studies. Believed to inhibit the enzyme cyclooxygenase, which is essential in the biosynthesis of prostaglandins. Can cause hepatotoxicity; hence, liver enzymes should be monitored in the first 8 wk of treatment. Rapidly absorbed; metabolism occurs in liver by demethylation, deacetylation, and glucuronide conjugation. Delayed-release, enteric-coated form is diclofenac sodium, and immediate release form is diclofenac potassium. Has relatively low risk for bleeding GI ulcers. Indomethacin (Indocin) Rapidly absorbed. Metabolism occurs in liver by demethylation, deacetylation, and glucuronide conjugation. Inhibits prostaglandin synthesis. Source: http://emedicine.medscape.com/article/927522-treatment http://emedicine.medscape.com/article/927522-diagnosis Nursing Management Nsg. Diagnoses:
1. Acute pain related to inflammation and distortion of tissues
2. Imbalanced nutrition: less than body requirements related to inability to ingest or absorb adequate nutrients 3. Deficient knowledge regarding pathophysiology, therepy choices, and self care needs related to lack of information, misinterpretation 4. Self-Care Deficit: bathing/hygiene and dressing/ grooming related to weakness 5. Activity Intolerance related to generalized weakness and pain 6. Anxiety related to change in health status Nursing Interventions Administer pain relievers as prescribed by the physician to promote comfort. Advice the client to have a nutritious diet and avoid excessive fats Post-op: remind the patient to cough hourly to prevent atelectasis Post op: instruct the patient to use a pillow to splint incision. To prevent bleeding, assess periodically for increased tenderness or rigidity of the abdomen and report it to the physician; instruct the patient and family to report change in color of stools
Monitor VS closely, inspect incision for bleeding When administering medications, teach the patient about its actions and possible side effects that are to be expected Instruct the patient to report immediately in case symptoms of jaundice, dark urine, pale stools, pruritus, or signs of infection Provide written and verbal instructions to the patent and family about managing pain and about signs and symptoms of intra-abdominal complications that should be reported such as loss of appetite, vomiting, temp elevation Emphasize the importance of keeping follow-up appointments
You might also like
- Hepatocellular Carcinoma: Hepatocellular Carcinoma (HCC, Also Called Malignant Hepatoma) Is The MostDocument10 pagesHepatocellular Carcinoma: Hepatocellular Carcinoma (HCC, Also Called Malignant Hepatoma) Is The MostNurul An NisaNo ratings yet
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Hepatitis B Is A Disease Caused by Hepatitis B Virus (HBV) WhichDocument12 pagesHepatitis B Is A Disease Caused by Hepatitis B Virus (HBV) Whichriel75% (4)
- Medicine Colloquium Exam - 2010 ADocument36 pagesMedicine Colloquium Exam - 2010 ARasha KhoumassiNo ratings yet
- NCP Cholecystectomy RevisedDocument7 pagesNCP Cholecystectomy RevisedMariquita Buenafe100% (4)
- Dave Jay S. Manriquez RN. Acute CholecystitisDocument11 pagesDave Jay S. Manriquez RN. Acute CholecystitisChilleMaeNo ratings yet
- Cholelithiasis: - Other Names: - Gallbladder Attack - Biliary Colic - Gallstone Attack - Bile Calculus - Biliary CalculusDocument101 pagesCholelithiasis: - Other Names: - Gallbladder Attack - Biliary Colic - Gallstone Attack - Bile Calculus - Biliary CalculusYvonne100% (1)
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Pathophysiology FinalDocument2 pagesPathophysiology FinallarissedeleonNo ratings yet
- CholelitiasisDocument42 pagesCholelitiasisEdwin YosuaNo ratings yet
- PAtho CholecystitisDocument2 pagesPAtho CholecystitisJanry-Mae Escobar TumanengNo ratings yet
- Chronic PyelonephritisDocument6 pagesChronic PyelonephritisKaustav JainNo ratings yet
- Pa Tho Irritable Bowel SyndromeDocument1 pagePa Tho Irritable Bowel Syndromekaye0403No ratings yet
- AppendicitisDocument57 pagesAppendicitisYessi KoruaNo ratings yet
- Benign Prostatic HyperplasiaDocument14 pagesBenign Prostatic HyperplasiaFatima Love Ariate-ArcasetasNo ratings yet
- Cholecystitis Litiasis EctomyDocument23 pagesCholecystitis Litiasis EctomyTimothy WilliamsNo ratings yet
- Cholelithiasis 0232Document118 pagesCholelithiasis 0232Kz LonerNo ratings yet
- Presentation 1Document71 pagesPresentation 1http_uglyNo ratings yet
- Malnutrition in Older AdultsDocument44 pagesMalnutrition in Older Adultsjohnjoe subaynoNo ratings yet
- Group 1 Family Case Study 1Document15 pagesGroup 1 Family Case Study 1Monique LeonardoNo ratings yet
- Gouty Arthritis: Presented By: Petit Ivy Mae B. NacarioDocument21 pagesGouty Arthritis: Presented By: Petit Ivy Mae B. NacarioMarivic DianoNo ratings yet
- Gallbladder HydropsDocument6 pagesGallbladder HydropsSaifulAnamNo ratings yet
- Bea-Case StudyDocument21 pagesBea-Case Studybea pegadNo ratings yet
- Acute PyelonephritisDocument16 pagesAcute PyelonephritisDilshan WickramanayakaNo ratings yet
- Case StudyDocument18 pagesCase StudyJonathan Delos ReyesNo ratings yet
- Danger Signs of PregnancyDocument3 pagesDanger Signs of PregnancyNesly Khyrozz LorenzoNo ratings yet
- Pathophysiology of Diabetes Mellitus Type II and NephrolithiasisDocument6 pagesPathophysiology of Diabetes Mellitus Type II and Nephrolithiasisdiane_mananganNo ratings yet
- CholelithiasisDocument3 pagesCholelithiasisMIlanSagittarius0% (1)
- Liver AbscessDocument6 pagesLiver AbscessKenneth SunicoNo ratings yet
- CHOLELITHIASISSDocument29 pagesCHOLELITHIASISSAngelica Mercado SirotNo ratings yet
- Pathophysiology of Acute CholecystitisDocument2 pagesPathophysiology of Acute CholecystitisKush KhannaNo ratings yet
- 11 NCP Pressure UlcerDocument6 pages11 NCP Pressure UlcerICa MarlinaNo ratings yet
- LECTURES Liver PathophysiologyDocument118 pagesLECTURES Liver PathophysiologyTarik100% (1)
- Reflection PaperDocument2 pagesReflection PapershanoiapowelllNo ratings yet
- Liver Case StudyDocument6 pagesLiver Case StudyGhulam MustafaNo ratings yet
- Kawasaki DiseaseDocument7 pagesKawasaki DiseaseRitamariaNo ratings yet
- NephrolithiasisDocument30 pagesNephrolithiasisHemakanen NairNo ratings yet
- Case 052: Biliary ColicDocument4 pagesCase 052: Biliary ColicZauzaNo ratings yet
- NON-ALCOHOLIC FATTY LIVEr DISEASE (NAFLD) - NASHDocument4 pagesNON-ALCOHOLIC FATTY LIVEr DISEASE (NAFLD) - NASHJason FooNo ratings yet
- GIT DiSEASES Dumping SyndromeDocument3 pagesGIT DiSEASES Dumping SyndromeLheidaniel MMM.No ratings yet
- Intestinal ObstructionDocument35 pagesIntestinal Obstructionwht89100% (1)
- Etiology, Pathophysiology, and Clinical Manifestations of CholecystitisDocument3 pagesEtiology, Pathophysiology, and Clinical Manifestations of CholecystitisGerriNo ratings yet
- Chronic PyelonephritisDocument5 pagesChronic PyelonephritisIsak ShatikaNo ratings yet
- Pathophysiology (Client Base) :: Predisposing Factors: Precipitating FactorsDocument1 pagePathophysiology (Client Base) :: Predisposing Factors: Precipitating Factorsleslie_macasaetNo ratings yet
- Complete Intestinal ObstructionDocument8 pagesComplete Intestinal ObstructionThuganamix100% (2)
- Gastric CancerDocument7 pagesGastric CancerMicah PingawanNo ratings yet
- Path o PhysiologyDocument9 pagesPath o PhysiologyKyle Ü D. CunanersNo ratings yet
- Liver AbscessDocument3 pagesLiver AbscessLyiuiu TranNo ratings yet
- Pathophysiology of HerniaDocument2 pagesPathophysiology of HerniaClaudia Narinda R. PNo ratings yet
- MEDIATRIXDocument67 pagesMEDIATRIXMaria Consuelo LingcasoNo ratings yet
- Mixed HemorrhoidsDocument4 pagesMixed HemorrhoidsHerne BalberdeNo ratings yet
- Grabe Ka FinalDocument57 pagesGrabe Ka FinalJoanne Bernadette AguilarNo ratings yet
- Anemia in PregnancyDocument13 pagesAnemia in PregnancyHerliyaNo ratings yet
- Anal Canal: Fissure in Ano HaemorrhoidsDocument37 pagesAnal Canal: Fissure in Ano Haemorrhoidsyash shrivastavaNo ratings yet
- Presentation PathophysiologyDocument11 pagesPresentation PathophysiologyJade DeopidoNo ratings yet
- Uremic EncephalopathyDocument12 pagesUremic EncephalopathyRAechelle_Marc_4102No ratings yet
- CroupDocument20 pagesCroupFariezuan HamidNo ratings yet
- Intestinal ObstructionDocument6 pagesIntestinal ObstructionCling Cruza0% (1)
- IV PathophysiologyDocument5 pagesIV PathophysiologyJanedear Pasal100% (1)
- A Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Cholelithiasis RLDocument29 pagesCholelithiasis RLPrincess Joanna Marie B DelfinoNo ratings yet
- Cholecystitis IntroductionDocument4 pagesCholecystitis IntroductionJechelle Ann Pabustan Martin-BoniquitNo ratings yet
- Case Stydy On CholithiasisDocument29 pagesCase Stydy On CholithiasisDaniel TalleyNo ratings yet
- Chronic Obstructive Pulmonary Disease: EmphysemaDocument11 pagesChronic Obstructive Pulmonary Disease: EmphysemarielNo ratings yet
- Thrombocytopenia Brief DiscussionDocument11 pagesThrombocytopenia Brief Discussionriel100% (3)
- Powerpoint: Gall Stone Disease and Related DisordersDocument70 pagesPowerpoint: Gall Stone Disease and Related Disordersj.doe.hex_8767% (3)
- Test Bank HepaticDocument75 pagesTest Bank HepaticDesiree ArquisolaNo ratings yet
- Daily Peanut and Peanut Butter Consumption Reduces Risk of GallstonesDocument6 pagesDaily Peanut and Peanut Butter Consumption Reduces Risk of Gallstonesdargen_121988No ratings yet
- 2020 Taiwan - Acute Pancreatitis GuidelineDocument10 pages2020 Taiwan - Acute Pancreatitis Guideline吳任爵No ratings yet
- Medicine Colloquium Exam - 2015 ADocument41 pagesMedicine Colloquium Exam - 2015 ArachaNo ratings yet
- Chole CystitisDocument43 pagesChole CystitisBheru LalNo ratings yet
- Ascites BY: Muhammad Javaid Iqbal PGR Paediatric Surgery Services Hospital LahoreDocument40 pagesAscites BY: Muhammad Javaid Iqbal PGR Paediatric Surgery Services Hospital LahoreJavaid KhanNo ratings yet
- Abdominal Pain During PregnancyDocument64 pagesAbdominal Pain During Pregnancykhadzx100% (2)
- Insignis Surgery 2 Gallbladder and Extrahepatic Biliary SystemDocument7 pagesInsignis Surgery 2 Gallbladder and Extrahepatic Biliary SystemPARADISE JanoNo ratings yet
- Cholecystectomy During The Weekend Increases Patients' Length of Hospital StayDocument7 pagesCholecystectomy During The Weekend Increases Patients' Length of Hospital StayRafael Silva PoloNo ratings yet
- 1 A PDFDocument51 pages1 A PDFMysheb SSNo ratings yet
- Open Cholecystectomy: By: Santoyo, Sarah Jane R. BSN 3-B Group 6-Operating RoomDocument6 pagesOpen Cholecystectomy: By: Santoyo, Sarah Jane R. BSN 3-B Group 6-Operating RoomJullie Anne SantoyoNo ratings yet
- Activity Intolerance CholecystectomyDocument2 pagesActivity Intolerance CholecystectomyPrincess Danica Purcia100% (3)
- Table e - Liver Anatomy Biliary SystemDocument11 pagesTable e - Liver Anatomy Biliary Systemapi-371971600No ratings yet
- Bile Duct Obstruction After CholecystectomyDocument3 pagesBile Duct Obstruction After Cholecystectomymercedes_hjNo ratings yet
- Chole Lithia SisDocument55 pagesChole Lithia Sisjaja_gatanNo ratings yet
- General Surgery II Exam PaperDocument2 pagesGeneral Surgery II Exam PaperSheikh Muhammad TabieshNo ratings yet
- Week2Handout - NDT - Liver, Gallbladder, and PancreasDocument7 pagesWeek2Handout - NDT - Liver, Gallbladder, and PancreasMegumi S.No ratings yet
- 12.fisiologi Sistem Hepatobilier PankreasDocument34 pages12.fisiologi Sistem Hepatobilier PankreasakreditasirsurNo ratings yet
- خارطة اختبار الترميز الطبيDocument3 pagesخارطة اختبار الترميز الطبيANFALNo ratings yet
- Gallstone DiseaseDocument14 pagesGallstone DiseaseSuryaAtmajayaNo ratings yet
- 4 Series CPTDocument13 pages4 Series CPTPraviiNo ratings yet
- Sample Health History 1Document6 pagesSample Health History 1Maria Elvira Abrogena DuadNo ratings yet
- A Case StudyDocument30 pagesA Case StudyJie BandelariaNo ratings yet
- 5. Chronic pancreatitis. СholelithiasisDocument58 pages5. Chronic pancreatitis. Сholelithiasischai rinNo ratings yet
- Gallstone Disease: Tad Kim, M.D. Connie Lee, M.DDocument35 pagesGallstone Disease: Tad Kim, M.D. Connie Lee, M.DWorapat ChNo ratings yet
- Understanding Medical Surgical Nursing - 0841-0841Document1 pageUnderstanding Medical Surgical Nursing - 0841-0841Anas TasyaNo ratings yet
- 4-Biliary InjuryDocument228 pages4-Biliary InjuryHamidHassanNo ratings yet