Professional Documents
Culture Documents
On Conflicting Principles of Medically-Assisted-Suicide
On Conflicting Principles of Medically-Assisted-Suicide
Uploaded by
dfsustentoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
On Conflicting Principles of Medically-Assisted-Suicide
On Conflicting Principles of Medically-Assisted-Suicide
Uploaded by
dfsustentoCopyright:
Available Formats
On Conflicting Principles
Running head: ON CONFLICTING PRINCIPLES OF MEDICALLY-ASSISTED -SUICIDE
On Conflicting Principles of Medically-Assisted-Suicide Daniel Francis D. Sustento, R.N. University of San Agustin Offshore Extension Program
On Conflicting Principles
Abstract Early in the actual practise of medicine, health team members pledge an oath expressed in Latin as Primum non nocere which means first, do no harm with accompanying principle of promoting good. Though made centuries ago, this is still open to varied conflicting interpretations especially on death issues. It is a theme subject to a lot of controversies especially in the medical field. Is it morally right for medical personnel to acknowledge living relatives request to put an end to the suffering of the patient? Will they be convicted even if they only willed the good effect of the act? And is putting clients agony to rest reason enough for medical professionals to proceed with assisted-suicide?
On Conflicting Principles
Medically-assisted-suicide One of the most divisive issues that continually haunts the medical field is euthanasia. Described by Arthur (1981) in his book Morality and Moral Controversies as the act of exterminating individuals who are either terminally ill, suffering tremendously or severely retarded (p. 161). Furthermore, gaining paramount attention is the issue regarding medically-assisted-suicide where physicians along with other members of the health team participate in hastening of the clients death may it be the decision of the patients themselves or the immediate family members. Clinical Encounter Shortly after graduation from college I entered the portals of a certain medical institution that served as my second home for approximately two years. I already readied myself that its going to be one bumpy ride but I was caught off guard for I was about to experience more than what I had expected. Early on the experience it was just like schooling again. Getting to know superiors, colleagues and other members of the healthcare team, facing the strain of schedule shiftings especially the dreaded graveyard duty hours, learning the ropes of nurse-patient-interaction and more. And as I delved deeper into the field all of those became customary but I know there is more to Nursing than just these and I was not mistaken. There are certain points in the experience where everything seemed to warp. I came across situations that warrant grave decision making and decisive action with restricted crucial options bounded with so little time. I can still vividly remember one of those moments. I didnt take part in it actually; it just so happened that I was in that inopportune circumstance at that ill-fated time. A client was admitted to the emergency department after arriving by rescue unit. According to the paramedic, the client was heavily injured from a head-on vehicular collision. No overt bleeding was noted only a large contusion in right upper region of the head. As expected, the client was unconscious and was in a fairly odd position. Both of his extremities were extended.
On Conflicting Principles
Examination revealed unequal pupil diameter, labored breathing with periods of apnea (cessation of breathing), declining oxygen levels, increasing abdominal girth that suggests concealed bleeding in the abdominal cavity and a blood pressure of sixty over forty. He was submitted to further diagnostic analyses to confirm the gravity of his condition. He was placed in a long tube that took images of his brain. The test showed that blood is slowly sneaking into the area of the brain that controls his respiration. This is a moribund sign. It could only mean that if the client will not undergo operation to evacuate the clot and stop the bleeding, he will die in a matter of hours. Since this was an emergency condition, no informed consent was obtained and the client was wheeled to the operating theatre. The surgery went well with minor complications but this was not a guarantee that he may survive. He was then placed in the Intensive Care Unit for close monitoring. Various tubes were attached to his frail body. One for fluids and medications, another for blood transfusion, one for stomach secretions conduit, two for drainage of blood from the operative site and a fairly large tube that is attached to an apparatus that maintains his respiration. The room was filled with blipping sounds as his vitals were measured every so often by various equipments attached to him apart from the mentioned tubes. When the clients immediate family members arrived in the hospital they were immediately confronted by the attending physician regarding the prognosis. He told them that the client has a very slim chance of continued existence and if by any miracle the patient survives, he will be in a persistent vegetative state with no chance of regaining his mental faculties. They were given the option of whether to continue the medical treatment or not, to withhold resuscitative efforts to keep the client alive in the event of cardiac arrest and/or theyll give the doctor full authority to inject a substance that will bring to halt clients heart beat. It took the family ten long days to decide on the matter and as each day passed, the client was slowly waning. It was such a tough decision to make especially when the odds are at their peaks and that family members were holding on to that trifle hope of survival.
On Conflicting Principles
Finally, after a long test of emotional battery, the family decided to hand out the concern to whatever the physician deemed necessary. A full written document was made duly signed by the members involved stating that the family has given the physician the right to administer a drug that will lead to the death of the client and that he will not be indicted for whatever consequence that may arise from that course of action. And from there everything went smoothly. The doctor injected the substance directly into the patients vein and the once regularly beeping noises of the room finally had come to a still. Morality check One does not simply rely on spur-of-the-moment emotion to decide whether a certain act is evil or not and to determine the next course of action. Then, are there guidelines that weigh the morality of a deed and direct its performance? According to Levine (1991), the most comprehensive source is a theory of ethics a broad set or moral principles that are used in measuring human conduct (p. xv). Lets take an ardent look at the following principles and theories and their take on the mentioned situation: The twofold effect, teleological, deontological and natural law theories. The principle of double effect Performance of a certain action is usually accompanied by outcomes. A number may have good effects while some generate bad results. Obviously, actions that result in good consequence may be done and otherwise if it will cause evil effect. But what if a deed engenders two both bad and good? Are we suppose to execute it or not? On the eve of the universitys biannual swimming competition, participants were busy practising, testing the waters as they usually say. Two competitors were fighting it out to determine who has the greater edge in winning the title. In the heat of the battle, no one noticed that the other opponent was constantly bleeding due to a cut in the brow because he accidentally banged his head against the lane when he reached the 2nd lap.
On Conflicting Principles
When the swimmer came out of the water, a medic went over him directly pressing an ice cap over his head. He cleansed the wound with an antiseptic solution that surely pained the individual for he was grimacing every time the solution touches his wound. The medic wasnt budged by what he saw since he knew that the medication will prevent the development of infection. According to the book Moral Principles of Nursing by Hayes, Hayes & Kelly (1964): The science of ethics lays down certain conditions which must be fulfilled to justify an action that has both a good and a bad effect. These conditions are the following: 1. The action must be in itself morally good or at least morally indifferent. 2. The good effect of the action must not come from an evil effect but must come from the action itself directly. 3. The good must be willed, and the evil merely allowed. 4. The good effect must be at least equivalent in importance to the evil effect. In other words, there must be sufficient reason to permit the evil effect. In the circumstance stated earlier, the performance of applying an antiseptic solution is inherently good and that the good effect (prevention of infection) does not directly come from the evil effect which is pain. Further, the medic only willed the avoidance of infection and not the causation of discomfort and that ultimately, the good effect far outweighs the bad. Relative to my experience, the act clearly infringes the principle of twofold effect. The action which is to assist in the clients suicide is neither morally good nor morally indifferent. It is apparently evil. The good effect of freeing the client from unnecessary suffering, on the other hand, results from killing and so therefore not permissible. We certainly should not do evil in order to gain good.
On Conflicting Principles
Teleological Theories Teleology comes from the Greek word telos which means end or purpose. Theories under this category simply advocate that the end or purpose determines the morality of an act. Foremost principle typified under teleology is ultilitarianism. Jeremy Bentham, one of the major proponents of ultilitarianism, avowed that human beings should be guided by the tenet greatest good for the greater number of people (Levine, 1991). He further delineated that pleasure is good and pain evil. And so therefore, a deed is considered good if it brings about pleasant, pleasurable consequences and that an action is evil if it results in bad, painful outcomes. Ultilitarianism is highly practical and sensitive as Joseph Fletcher puts it a man should not piously follow moral rules but rather be guided by compassion towards the needs of the individual. Conversely, this theory opposes the verdict of the twofold effect. The act of assisting the client to his own death, though glum as it may sound, is justified for it did not only conclude the individuals pain and unnecessary suffering but also has put to end monetary struggle and the unfathomable misery of family members as they watch their beloved slowly waning right before their very eyes. Deontological Theories Deon. A Greek term signifying duty is basic to all theories supporting Deontology. It indicates that the wrongness and rightness of an action stems from its conformity to moral law and not merely on the basis of whether or not it results in either bad or good consequences. A major proponent of deontological theory is Emmanuel Kant, a German philosopher and scientist, who purported that an action, for it to be good, must correspond with the ultimate duty of man to abide by what he called the moral law.
On Conflicting Principles
Moral law according to Kant is one that can serve as a guide for peoples behaviour, something that a person can impose on himself and not just simply commanded by the state or societal norms. He simplified this by suggesting that every individual has equal worth and that they should be treated as such. Then again, in sync with the condition formerly presented, deontological theory refutes the morality of assisted-suicide. Individuals have parallel significance and that includes life. Life in itself is absolute. It does not stand in accord with the value of either good or evil and therefore, to put it out means going against Kantian Moral Law and is considered entirely evil. Natural Law Theory Natural Law, whose foundations were first built by St. Thomas Aquinas, regards norms or rules inherent in human beings as the bases of determining the morality of an act. According to this theory, an action can be considered good if it corresponds to the nature of man which can only be determined through the exercise of reason alone. For example, a nurse steals the valuables of a client admitted to undergo emergency procedure. The act, by virtue of human reason, is wrong and it goes in contradiction with the natural law therefore making the deed immoral. Intrinsic to human beings is the natural law and so therefore it is universal. It does not stand with regard to culture, demography and the like. Consequently, actions divergent of the natural law, including taking away another persons life, are and will forever be morally wrong. Finally, no human authority has the power to dispense, alter, abrogate any precept of the natural law (Hayes, Hayes & Kelly, 1964). Viewpoint 1: Inviolability of Human Life One cannot own anything until he is already alive. Life is a prerequisite to ownership. Therefore no man owns his life. The owner of human life is not man but God, who gave life to man (Hayes et al., 1964).
On Conflicting Principles
Ownership. Such an absolute term that implies possession, right, power and sovereignty over almost anything and everything imaginable yet the very word that has always been misconstrued since the beginning. When God gave man his life, along with it comes dominion dominion over beasts of the jungle, monsters of the ocean, fierce creatures of the sky and tame and gentle living things that walk the earth. That same authority vested him the right to life and so it follows that he has deep obligation to conserve it until God himself sees fitting to take it back. However man, in his limited intellect, sees it in a different paradigm. To be a custodian of life means the utmost power not only to guard but at the same time to regulate it whether or not it is of worth to sustain or otherwise. Basic to this contention is the inviolability of human life stating that no man has the right to take away the life of others least his own. Viewpoint 2: Philosophical and theological perspectives Philosophically, reason alone will suggest that mere infliction of harm more so imposing death to a person tarnishes the pride and honour of the profession and if we are to embrace the concept of divinity, religion shall direct us to the law intricately etched in the two stone tablets handed down to Moses by God depicting Thou shall not kill. This is perceptibly a fixed contravention of the sacredness of human life by members of the medical profession. Viewpoint 3: Slayer versus Healer Consistent with medical law, professionals in the field of medicine are called to preserve and maintain life and further, have sworn under Hippocratic Oath total defiance of any request to end their clients lives.
On Conflicting Principles
10
In addition, according Levine (1991): Physicians provide medical treatments to the sick to make them well, or as well as they can become. Treatment designed to bring on death, by definition, does not heal and is therefore fundamentally inconsistent with the physicians role. Therefore divergence from the idea mentioned above, in whatever ways deemed possible, makes them no less than criminals overruling what they were called for and persons who either insinuate or decide to seize the matter on their hands up to the extent of taking another individuals life is guilty of repudiating its worthiness. Ultimately, medical teams decision to participate in an act to directly eliminate a patients life spoils the very nature of the field with which it has been founded to do no harm. Viewpoint 4: Effect on the client Various rights affect the command of things especially in the clinical area. An individual is entitled to self-determination and autonomy to decide including the option to refuse medical care and other life-sustaining measures. This principle however has its pitfall. Keen analysis supports that this too encompasses the individuals right to take away his/her life. Therefore, health team members contribution to the act condones the actual performance of suicide making the client feel that indeed his or her life is meaningless and is without worth. Viewpoint 5: Awareness of the public In our value-laden society, increasing awareness of physician-assisted-suicide threatens the principles and ideals being upheld by a profession long been considered noble. Though to particulars this may receive a profound acceptance, this too shall be meted with strongly-raised eyebrows and be considered immoral to the appeal of the general population. How can they earn respect if they, themselves, do not know how to revere the divinity of human life? Further, how can they be of help if early in the process they are already being feared?
On Conflicting Principles
11
Try as they may, they can never hide from this inconvenient truth for they already are convicted in the eyes of the people that once their hands had been tainted with blood of those whom they assisted to die. Merit of Respect In the field of healthcare, as Ruth Macklin placed it, the kinds of rights that should be exercised by the relatives of clients who cannot decide for themselves and the people who are obligated to impose it are not clearly delineated (Levine, 1991). Reason enough for ethical dilemmas to arise especially if standpoints of the healthcare team and that of the family are incongruous. However in the situation presented, the position of both parties was mutual so conflict was unlikely to happen. To each his own. Every person is entitled to his individual preference. And in the context of rudimentary ethical principles, respect takes precedence over the others and thus, all that was left for me to do, though against my own personal belief, was to accept the decision of the physician and the clients family members. Wrapping it up In the light of the ideologies and theories mentioned above, it is suggested that in order to continually uphold the nobility of the profession in the event moral confusion and conflicting principles, the health team should take pause and reflect on the very foundation of their profession saving lives. They should also keep in mind that by justifying deeds that are distinctively iniquitous, they legitimize them.
On Conflicting Principles
12
REFERENCES
Arthur, J. (Ed.). (1981). Morality and Moral Controversies (4th ed.). New Jersey: Prentice-Hall, Incorporated. Baumrind, D. (1985). Research using intentional deception: Ethical issues revisited. American Psychologist, 40(2), 165-174. Dyck, A. (1973). An Alternative to the Ethic of Euthanasia. New York: Springer-Verlag. Levine, C. (1991). Taking sides: Clashing views on controversial bioethical issues. Connecticut: The Dushkin Publishing Group, Inc. Orentlicher, D. (1989). Physician participation in assisted suicide. Journal of the American Medical Association, 262(13), 1844-1845. Rachels, J. (1975). Active and passive euthanasia. The New England Journal of Medicine, 292(2), 78-80. Rev. Hayes, E.F., Rev. Msgr. Hayes, P.F., & Kelly, D.E., R.N. (1964). Moral principles of nursing: A compendium of principles, spiritual aids, and concise answers regarding Roman Catholic patients, personnel, and problems. New York: Macmillan Company. Wanzer, S.H., Federman, D.D., Edelstein, S.J., et al. (1989) The physicians responsibility toward hopelessly ill patients: A second look. The New England Journal of Medicine, 320(13), 846-848.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Home Health Services Coverage and Limitations Handbook - AdoptionDocument104 pagesHome Health Services Coverage and Limitations Handbook - AdoptionRad EkkawiNo ratings yet
- Textbook For Mrcog 1 by Richa Saxena 9385891286Document5 pagesTextbook For Mrcog 1 by Richa Saxena 9385891286DrMuhammad Hassan50% (2)
- LOPADocument84 pagesLOPAM100% (4)
- Final Sop Manual-1-1Document62 pagesFinal Sop Manual-1-1Dianne JoyNo ratings yet
- Big Blue Miller 700Document98 pagesBig Blue Miller 700Juan Eduardo JeRico100% (1)
- 1 Fee Structure For Regular Students 22 23Document1 page1 Fee Structure For Regular Students 22 23Haseeb BuzdarNo ratings yet
- Harga Jual - XLSX - Sheet1Document13 pagesHarga Jual - XLSX - Sheet1HADI PRAYITNONo ratings yet
- Tle9 Agricrop q2 m1 Handlingmaterialsequipment v2Document32 pagesTle9 Agricrop q2 m1 Handlingmaterialsequipment v2Bernadeth Torres LibradoNo ratings yet
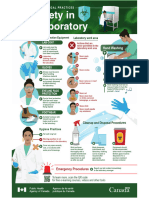
- Biosafety in The LaboratoryDocument1 pageBiosafety in The LaboratoryALFARO CHAT CARMINA ROSARIONo ratings yet
- Awareness On Comprehensive Sexuality Education Among Junior High School Teacherstowards The Designing of Teacher'S Training ModulesDocument9 pagesAwareness On Comprehensive Sexuality Education Among Junior High School Teacherstowards The Designing of Teacher'S Training ModulesJulia Mar Antonete Tamayo AcedoNo ratings yet
- Labrep. 1Document6 pagesLabrep. 1Joy MananganNo ratings yet
- Lingual-Keys For SuccessDocument8 pagesLingual-Keys For SuccessGoutam NookalaNo ratings yet
- Promissory Note Promissory Note: Mauban District Hospital Mauban District HospitalDocument2 pagesPromissory Note Promissory Note: Mauban District Hospital Mauban District HospitalKC PalattaoNo ratings yet
- Light 27 Web FinalDocument28 pagesLight 27 Web FinalrafilhouseNo ratings yet
- Atlanticare TQM Implementation Case StudyDocument16 pagesAtlanticare TQM Implementation Case Study6132 PRINCE KUMARNo ratings yet
- Inpharmation February 2013Document16 pagesInpharmation February 2013ChemistixNo ratings yet
- Material Safety Data Sheet: I. General InformationDocument7 pagesMaterial Safety Data Sheet: I. General InformationPemalang HockNo ratings yet
- Working at Height TrainingDocument47 pagesWorking at Height TrainingthinkpadNo ratings yet
- Oral Hygiene InstructionsDocument20 pagesOral Hygiene Instructionsapi-307943695No ratings yet
- DBL Group TPWL Water Reuse System at Industrial ScaleDocument15 pagesDBL Group TPWL Water Reuse System at Industrial ScaleNavid ZamanNo ratings yet
- Chapter 2: Gerontological NursingDocument14 pagesChapter 2: Gerontological Nursingaznknight323100% (1)
- Elder AbuseDocument18 pagesElder Abusehermione1402No ratings yet
- Ten Personality Disorders - Neel Burton MDDocument11 pagesTen Personality Disorders - Neel Burton MDcgarciNo ratings yet
- Safety Campaign-Bypassing Safety Control-Feb 2022Document4 pagesSafety Campaign-Bypassing Safety Control-Feb 2022HSE99 BHDCNo ratings yet
- GHMC ABC VetDocument2 pagesGHMC ABC VetApril SamaNo ratings yet
- 58 - Towards A Philosophy of Public HealthDocument7 pages58 - Towards A Philosophy of Public HealthprabowoNo ratings yet
- HEARTDocument11 pagesHEART1NC21IS038 POLATHALA MOUNIKANo ratings yet
- Assignment On Decision Making ProcessDocument23 pagesAssignment On Decision Making ProcessMuhammad SaeedNo ratings yet
- Thesis Topics For Construction Project ManagementDocument7 pagesThesis Topics For Construction Project Managementbsqbr7px100% (1)
- Vitamin K: Adjunct To Vitamin DDocument7 pagesVitamin K: Adjunct To Vitamin DBeena WalvekarNo ratings yet