Professional Documents
Culture Documents
Obstetrics Gynecology Physical Therapy Assessment
Obstetrics Gynecology Physical Therapy Assessment
Uploaded by
chri23Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Obstetrics Gynecology Physical Therapy Assessment
Obstetrics Gynecology Physical Therapy Assessment
Uploaded by
chri23Copyright:
Available Formats
OBG PT ASSESSMENT
Sagar Naik, PT
Obstetrics & Gynecology PT Assessment
Sagar Naik,
PT
Acknowledgement: Dr. Prerana Maam
The obstetric woman may attend the physiotherapy throughout the year. Physiotherapist may have to monitor them and screen them in regular intervals.
Subjective Examination:
General Details Name Age Address Marital status - Duration of marriage - Consanguinity marriage Chief Complains (Present problems of the woman) Period of amenorrhea Nausea, vomiting Musculoskeletal Problems - Low backache - Radiating pain - Numbness or tingling sensations - Cramps Frequency of micturition Weakness Blood pressure Headache, epigastric pain Swelling in both the limbs Obstetric History Gravida & Parity Multiple pregnancies (duration between pregnancies) Number of living children (Boys & Girls, Twins) History of previous deliveries - Full-term normal delivery - Low section cesarean section - Episiotomy
ph y
sio
4a
ll.. .
OBG PT ASSESSMENT
Sagar Naik, PT
Health status of previous baby (any congenital abnormalities) History of previous abortions - Still born or death after birth - Spontaneous abortion or Induced abortion Details about menstruation History of any diseases during pregnancy (pelvic inflammatory disease) History of rubella or cytomegalovirus, toxoplasmosis infection History of dizziness while sudden change of position from lying to sitting or standing (postural hypotension) Any trauma during pregnancy Any itching over the perineal area (piles) Place of delivery Details about anesthesia (postnatally) Type of labour (induced or spontaneous) History of breast-feeding (postnatally) History for Genitourinary System Any burning sensations during micturition Retention of urine Polyuria or Oligouria (Diabetes symptoms) History of Incontinence Dribbling of urine during coughing, or other activities Feeling of something descending down per vaginum History for Gastrointestinal System Loss of appetite Loss of weight Constipation Heartburn Piles Pain History Onset of symptoms Duration of symptoms Type & location of pain Aggravating and Relieving factors Ask similar symptoms felt during previous pregnancies Past History Any history of Tuberculosis Bronchial Asthma Blood Pressure Diabetes Mellitus Hyperthyroidism or Hypothyroidism
ph y
sio
4a
ll.. .
OBG PT ASSESSMENT
Sagar Naik, PT
ph y
Drug History Any drugs taken during pregnancy Allergic to any drugs History about contraceptive measures taken Any Rh compatibility injections taken during previous pregnancy Family History History of twin pregnancy in family History of congenital defects present in any family member Socio-economic History Occupation of the client & her husband Number of family members (any help can be obtained for household activities during pregnancy) Cast and economic status of the client Medical & Surgical History Any surgical procedure done during delivery or during previous deliveries Psychological History Any emotional disturbances Anxiety or depression Any stress to the client during pregnancy Knowledge about the pregnancy and physiological changes, which occur during pregnancy
sio
Objective Examination: On Observation:
General condition Ectomorph Endomorph Mesomorph Edema (over leg & foot)
4a
ll.. .
Cardiac Problems HIV Anemia (sickle cell anemia, thalassemia) Any history of seizures or convulsions Autoimmune disorders like myasthenia gravis Personal History Any addiction smoking or alcoholism Sleeping habits Lifestyle of the client
OBG PT ASSESSMENT
Sagar Naik, PT
On Palpation:
ph y
sio
On Examination:
Tenderness Temperature variation of skin Spasm Scar (healed or unhealed) Swelling
Vital Signs Blood Pressure Heart Rate Pulse Respiratory Rate Abdominal Girth & Symphysis Fundal Height (SFH) Weight Range of Motion Within the permissible range Ballistic movements should be avoided End range pressure should be avoided Hypermobility of joints due to laxity of ligaments
4a
Trophic changes Pregnancy related changes - On face, cloasma gravidarum or pregnancy mask (around cheek, forehead and eyes) - On abdomen, linea nigra (midline from xiphisternum to symphysis pubis) - Striae gravidarum (abdominal walls below umbilicus, thighs and breast) Nail bed Pallor (anemia) Conjunctiva & Tongue Pallor (anemia) Yellowish (jaundice) Scar (postnatally during LSCS) Posture in lying, sitting, & standing Rounded shoulders Increased cervical lordosis (forward head posture) Increased lumbar lordosis Hyper extended knees Weight shifted posteriorly to ankle Gait Wide Base Of Support (BOS)
ll.. .
OBG PT ASSESSMENT
Sagar Naik, PT
ph y
Restricted trunk movements If edema present then restricted range at that joint Manual Muscle Testing Abdominal muscles Gluteal muscles Emphasis Perineal muscles Edema Assessment Girth measurement Volumetric measurement Diastasis Recti Assessment Hook lying position Slowly actively raise the head and shoulders off the floor, reaching her hands toward the knees, until the spine of the scapulae leaves the floor Place fingers of one hand horizontally across the midline of the abdomen at the umbilicus If separation exists, fingers will sink into the gap The number of fingers that can be placed between the rectus muscle bellies measures diastasis Less than 2 fingers or 2 cms is normal; more than 2 fingers or 2 cms is abnormal Instruct client to performed a self-diastasis test Sacroiliac Dysfunction Assessment Approximation test Gapping test Sacroiliac Rocking Test (SI Strain) Patricks Test (FABER test) Incontinence Assessment (Pelvic Floor Muscle Strength) Perinometry Pervaginal Examination - Examination is done by inserting two fingers (index & middle) wearing sterile gloves - Ask client to squeeze fingers as much as possible & strength of perineal muscles is checked
sio
4a
ll.. .
OBG PT ASSESSMENT
Sagar Naik, PT
Grades
Grade 1 (Trace) Grade 2 (Weak) Grade 3 (Moderate) Grade 4 (Strong)
Description
Contraction held less than 1 second
ph y
sio
Pad Test - First ask client to void urine and bear pre-weight sanitary pad after drinking 1000 ml of liquid - Ask to rest for 45 minutes and then do exercise for 30 minutes, which includes walking, climbing, coughing, jumping, etc - Pad is again test and weight. Resulting weight would be in grams of urine loss - 1 gram increase is normal to compensate possible discharge and sweating Biofeedback Ask client to cough and check for any dribbling of urine is present or not Exercise Tolerance Testing 6 minute walk test 3 step test Functional Assessment Gait Assessment
4a
ll.. .
Contraction held for 1-3 seconds or fingers not elevated Contraction held for 4-6 seconds and fingers elevated; repeat 3 times Contraction held for 7-9 seconds and fingers elevated; repeat 3 times Rapid contraction with elevation of Grade 5 fingers for 7-9 seconds; repeat 4 (Unmistakably Strong) times
You might also like
- Physiotherapy in Obstetrics and GynaecologyDocument493 pagesPhysiotherapy in Obstetrics and GynaecologyShanu Gal84% (19)
- Cerebral Palsy AssessmentDocument6 pagesCerebral Palsy AssessmentFEROZNAZIM100% (2)
- Neurological Physiotherapy Evaluation FormDocument6 pagesNeurological Physiotherapy Evaluation FormAsif Khan100% (4)
- Physiotherapy Management of Vascular DisordersDocument55 pagesPhysiotherapy Management of Vascular DisordersAkheel AhammedNo ratings yet
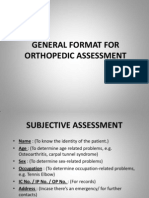
- General Format For Orthopedic AssessmentDocument27 pagesGeneral Format For Orthopedic AssessmentMegha Patani100% (7)
- Icu and PhysiotherapyDocument81 pagesIcu and PhysiotherapyLakshmi Prasanna100% (2)
- Physiotherapy in Alopecia AreataDocument21 pagesPhysiotherapy in Alopecia AreataAngel100% (2)
- Traumatic Brain Injury Physiotherapy AssessmentDocument20 pagesTraumatic Brain Injury Physiotherapy AssessmentNithin Nair100% (1)
- Cardiorespiratory AssessmentDocument7 pagesCardiorespiratory AssessmentHanna SofiaNo ratings yet
- Nonequilibrium Coordination TestsDocument1 pageNonequilibrium Coordination TestsElibmasac100% (5)
- Intervertebral Disc ProlapseDocument18 pagesIntervertebral Disc Prolapsemeto67% (3)
- Physiotherapy in General Surgical ConditionDocument7 pagesPhysiotherapy in General Surgical Conditionprofpt98100% (8)
- Obstretics AssessmentDocument6 pagesObstretics AssessmentToli kkakrNo ratings yet
- Assessment Form CPDocument13 pagesAssessment Form CPvmsvino100% (2)
- Post Thoracotomy Physiotherapy ManagementDocument25 pagesPost Thoracotomy Physiotherapy ManagementSiva Shanmugam100% (5)
- Vertebrobasilar SyndromeDocument14 pagesVertebrobasilar SyndromeHitesh RohitNo ratings yet
- Polio Physiotherapy NotesDocument6 pagesPolio Physiotherapy NotesyigoNo ratings yet
- 6 Minute Walk TestDocument12 pages6 Minute Walk TestAnanth NagarajNo ratings yet
- Cerebral Palsy AssessmentDocument8 pagesCerebral Palsy Assessmentrajalaxmi gopalakrishnanNo ratings yet
- Determinants RESISTED EX'SDocument24 pagesDeterminants RESISTED EX'Svenkata ramakrishnaiahNo ratings yet
- Faradic Foot BathDocument9 pagesFaradic Foot BathApoorv100% (2)
- Brachial Plexus InjuriesDocument32 pagesBrachial Plexus InjuriesFatima yasin50% (2)
- Functional Re-Education by Kusum-Wps OfficeDocument19 pagesFunctional Re-Education by Kusum-Wps OfficeKusum deep0% (1)
- PepDocument8 pagesPepUdayakrishnan P Kanhangad100% (1)
- IVDP: Inter Vertebral Disc ProlapseDocument34 pagesIVDP: Inter Vertebral Disc ProlapseShibinNo ratings yet
- Motor Relearning Programme: Prepared by Mohammad Bin Afsar JanDocument11 pagesMotor Relearning Programme: Prepared by Mohammad Bin Afsar Jankashmala afzal100% (1)
- Clinical Decision Making in Electrotherapeutics and Safety ConsiderationsDocument87 pagesClinical Decision Making in Electrotherapeutics and Safety Considerationsmayuri zanwar100% (1)
- Mat ActivitiesDocument20 pagesMat Activitiesmuthuu60% (5)
- Role of Physiotherapy in Management of Burns-HshDocument25 pagesRole of Physiotherapy in Management of Burns-HshChristopher Chibueze Igbo100% (1)
- Tendon Transfers - RehabilitationDocument4 pagesTendon Transfers - RehabilitationPankaj Malik100% (4)
- Erb's PalsyDocument18 pagesErb's PalsyMegha PataniNo ratings yet
- Muscle Plasticity in Response To Electrical StimulationDocument20 pagesMuscle Plasticity in Response To Electrical StimulationJanani Iyer100% (1)
- Cerebral Palsy Assessment ImportantDocument7 pagesCerebral Palsy Assessment Importantabra_arr100% (2)
- Chest Wall DeformitiesDocument25 pagesChest Wall DeformitiesRaghu NadhNo ratings yet
- Physiotherapy in Abdominal SurgeryDocument32 pagesPhysiotherapy in Abdominal SurgeryHUZAIFA YAMAANNo ratings yet
- Complications of Bed Rest 1Document4 pagesComplications of Bed Rest 1Geetha Bhavani100% (2)
- Spinal Cord Injury - Physical Therapy ManagementDocument86 pagesSpinal Cord Injury - Physical Therapy Managementphysiovipin96% (70)
- Supraspinatus TendinitisDocument23 pagesSupraspinatus TendinitisTafzz Sailo0% (1)
- DefinitionsDocument4 pagesDefinitionsKarthikeyan Guru67% (3)
- Extension Services and Mobile UnitsDocument27 pagesExtension Services and Mobile UnitsNaveen Kumar100% (2)
- Functional Reeducation Techniques: Presenter by Arambam Meiteileima Chanu 1 Year, MPT (Neuro)Document38 pagesFunctional Reeducation Techniques: Presenter by Arambam Meiteileima Chanu 1 Year, MPT (Neuro)deepuphysio94% (18)
- Rebox CurrentsDocument38 pagesRebox CurrentsProtantagonist75% (4)
- Capsular and Noncapsular MovementsDocument13 pagesCapsular and Noncapsular MovementsNoor DeenNo ratings yet
- Vojta TherapyDocument4 pagesVojta TherapyPrashu Jain100% (1)
- Mastectomy and Physiotherapy Management Final YearDocument24 pagesMastectomy and Physiotherapy Management Final YearNithin Nair57% (7)
- Faradic Foot BathDocument1 pageFaradic Foot BathJohn Ribu Parampil70% (10)
- ORTHOPAEDIC ASSESSMENT FORM - YoburajDocument3 pagesORTHOPAEDIC ASSESSMENT FORM - Yoburajsundar_kumar0No ratings yet
- Lec 9 Trick MovementsDocument19 pagesLec 9 Trick MovementsBhargav69% (13)
- Role of WHO and WCPTDocument36 pagesRole of WHO and WCPTsonali tushamer100% (1)
- Health Problems of Pregnant and Lactating WomanDocument45 pagesHealth Problems of Pregnant and Lactating WomanSuraj Sahu100% (1)
- Management Acute Abdomen: Briand Pollah Digestive RSUD JayapuraDocument54 pagesManagement Acute Abdomen: Briand Pollah Digestive RSUD JayapuraMuhammad MuhammadNo ratings yet
- POSTNATAL Assessment and CareDocument26 pagesPOSTNATAL Assessment and Careshruti sriNo ratings yet
- Antenatal Care: by DR Maimuna A GelleDocument28 pagesAntenatal Care: by DR Maimuna A GelleMahad Maxamed AxmedNo ratings yet
- Orthopedic History and Physical ExamDocument28 pagesOrthopedic History and Physical ExamAgriya Shresth100% (1)
- Lec.2 Assessment and History TakingDocument36 pagesLec.2 Assessment and History TakingDana AbabnehNo ratings yet
- L03 - History Taking & Physical ExaminationDocument34 pagesL03 - History Taking & Physical ExaminationLemi teshomeNo ratings yet
- Pedia PPT1Document52 pagesPedia PPT1Jan Mikhail FrascoNo ratings yet
- Slide 1 - The History and Physical ExamDocument38 pagesSlide 1 - The History and Physical ExamCWT2010No ratings yet
- OB HX and PEDocument37 pagesOB HX and PEdenekeNo ratings yet
- Uterine AnomaliesDocument24 pagesUterine AnomaliesAnaNo ratings yet