Professional Documents
Culture Documents
Is Waiver of Informed Consent in Trauma Research Ethical
Uploaded by
Marwa AlaamriOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Is Waiver of Informed Consent in Trauma Research Ethical
Uploaded by
Marwa AlaamriCopyright:
Available Formats
ANALYTICAL MEMORANDUM To: Dr.
Nasser From: Marwah Alameri Date: October 30, 2012 Subject: Is waiver of informed consent in trauma research ethical?
Informed consent plays an imperative role for human protection in clinical research. It ensures protection of subjects autonomy and prevents their exposure to undue risk. It is obtained for treatment and for research enrollment (Largent, Wendler, Emanuel, & Miller, 2010). However, obtaining subjects consent is challenging under stressful conditions. In traumatic situations, treatment is never withdrawn if obtaining informed consent from a critically ill patient is infeasible or postponed while in quest of a surrogates consent (Coats, 2012). Therefore, trauma research with the absence of subject or surrogate consent is ethical as it can proceed only if informed consent is waived. To provide informed consent, individuals must be accurately and fully informed about the researchs purpose, methods, risks, benefits and other alternatives. The patient is expected to comprehend the information and its effect on his own medical condition; and make a voluntary decision whether or not to enrol (Health Insurance Portability and Accountability Act, 2002). Simply, such requirements are absent in traumatic situations. In such catastrophic conditions, patients are either unconscious, i.e. lack decision-making capacity, or conscious but with compromised mental status due to acute physical or mental illness. These situations pose an obvious challenge for emergency physician to obtain consent of patients (John, 2006). During sudden, life-threatening events like cardiac arrest, traumatic brain injury or shock states, the autonomy of the acutely ill or injured patient has already been removed by the devastating nature of the pathology involved. At such critical times, the patient is vulnerable, and his opinion of whether to accept or reject a potentially life-sustaining intervention cannot be concluded (Lemaire, 2007). In addition, it is not the physician or the institutional review boards (IRBs) that remove the patients autonomy in these critical circumstances, but the efforts made to save his life (Morrison, Horwitz, & Carrick, 2009). In fact, the Final Rule, a set of regulations outlining situations in which emergency research could be conducted in humans under an exception of informed consent, states that under such circumstances the focus must be on the preservation of life (FDA Final Rule, 21 C.F.R 50.24, 1996). On the same line, in most trauma research, the investigator doesnt have the luxury of time. Investigational agents are likely to be effective only if administered within a certain period of time from the onset of the acute life threatening condition. Therefore to obtain the patients consent at the spot is infeasible (Graham, Judy, Lois van, Ron, Tom, Jim, & Al, 2006). In addition, obtaining patients consent prior to enrolment in a trauma research means there shouldnt be clinical trials in this critical field of medicine. Hence, it will deprive current and future patients from participation. In fact this has resulted in little research conducted in trauma settings to improve survival outcomes and has played a major role in causing trauma to be the main cause of death in the United States for individuals between ages 1 and 45 years (Minio, Anderson, Fingerhut, Boudreault , & Warner, 2006). On the other hand, there is disproportionate representation of racial minorities and people of low socioeconomic status in trauma research. For that reason, they are potentially at risk of being exploited, not only because of their compromised neurological or medical
George
Washington
University
ANALYTICAL MEMORANDUM To: Dr. Nasser From: Marwah Alameri Date: October 30, 2012 Subject: Is waiver of informed consent in trauma research ethical?
status, but because they are easily influenced as a result of their socioeconomic condition (Emanuel, 2000). Therefore, researchers have an obligation to justify any proposed research study that utilizes this patient population. Furthermore, researchers also have an obligation to respect the autonomy of the potential patients, and they must consider the possibility that some ethnic groups might be reluctant to participate due to religious reasons. Additionally, waiver of informed consent contradicts the three basic ethical principles, beneficence, justice and respect for persons, of research of the Belmont report (The Belmont Report, 1979). On a related point, surrogate consent in patients incapable of expressing their views due to cognitive impairment is an alternative. Health Insurance and Probability Act (HIPPA) requires informed consent from the patient or his surrogate (Health Insurance Portability and Accountability Act, 2002). Moreover, the Final rule was created for situations where there is no existing or alternative treatment; however physicians during emergency research use investigative treatment though proven medicine exist (FDA Final Rule, 21 C.F.R 50.24, 1996). Therefore, extending the same waiver of consent to research settings should be prohibited due to the unknown dangers of implementing unproven treatment compared with an existing treatment, whose safety and efficacy has already been clinically proven. For those reasons, waiver of informed consent is considered unethical. Trauma research can proceed only if informed consent is waived or deferred. It can be argued that those who suffer most from the lack of advancement and innovation in trauma research are individuals from minority populations. These same vulnerable groups also tend to have worse outcomes when treated with current treatment modalities. It is in such cases that obtaining informed consent, a practice that was originally instituted to protect vulnerable populations, is probably one of the major reasons that such little trauma research exists to benefit these populations today. Additionally, deferment from abiding to the principles of the Belmont report during trauma research is justified. Title 45 codes of federal regulations 46, also known as the Common Rule and derived from the Belmont report, clearly outlines separate regulations for research involving foetuses, children, and prisons as requiring additional protections, but leaves it up to individual IRBs to determine whether additional protections are needed for other groups of individuals who might also have diminished autonomy (FDA Protection of Human Subject, 45 C.F.R 46, 2009). In addition, international guidelines identify a list of potentially exploitable vulnerable populations including patients in emergency situations, which is relevant to patients in trauma research (Druml, 2004). In life threatening situations, consenting for the incapacitated patients is uncommon, as the possible surrogates are rarely on the spot. In situations where the surrogate is available, one cannot seriously consider that during such stressful situations, the conditions ensuring a
George
Washington
University
ANALYTICAL MEMORANDUM To: Dr. Nasser From: Marwah Alameri Date: October 30, 2012 Subject: Is waiver of informed consent in trauma research ethical?
satisfactory informed consent are met. Furthermore, surrogates decisions might vary from that of patients. Newman and colleagues concluded from observational cohort study significant discrepancies in the willingness to participate in hypothetical critical research studies between the critically ill and their surrogates (Newman, Smart, Reese, Williams, & Moss, 2012). Finally, though the Final rule was created for situations where there is no existing or alternative treatment, given the relative scarcity of prospective randomized clinical trials for many strategies currently used in trauma research, it can be difficult to pin down a definitive gold standard treatment. Furthermore, in many cases, standards of management have failed to significantly reduce morbidity and mortality. In such scenarios, it might be unethical to continue with the standard of care if it will result in poor outcomes where a better, but yet to be proven, option potentially exists (Morrison, Horwitz, & Carrick, 2009). In fact, there are situations in which access to experimental treatments may be directly beneficial to research subjects. Annane and colleagues showed that there was a link between the waiver of consent approved by French Competent Authority and the completion of their landmark study on the use of low doses of corticosteroids in the treatment of septic shock (Annane, Sebille, Charpentier, Bollaert, Francois, Korach, & ... Troche, 2002). This study had an impact on the current guidelines for septic shock management. In conclusion, given the priority of preserving patients life, the narrow time frame of treatment administration, the inherited absence of patients autonomy, the infeasibility of applying the informed consent requirements and the need to advance research for the benefit of the society, wavier of informed consent is ethically justifiable in trauma research. References Annane, D. D., Sebille, V. V., Charpentier, C. C., Bollaert, P. E., Francois, B. B., Korach, J.M., & ... Troche, G. G. (2002). Effect of treatment with low doses of Hydrocortisone and Fludrocortisone on mortality in patients with septic shock. Journal- American Medical Association, 288, 862-884. Belmont Report (1979). The Belmont Report: Ethical principles and guidelines for the protection of human subjects of research. Retrieved from http://www.hhs.gov/ohrp/policy/belmont.html Coats, T. (2012). Ethical and practical issues in trauma care research. The British Journal of Surgery, 99 Suppl 16-7. Druml, C. Informed consent of incapable (ICU) patients in Europe: existing laws and the EU directive. (2004). Current Opinion in Critical Care, 10(6), 570-73.
George Washington University
ANALYTICAL MEMORANDUM To: Dr. Nasser From: Marwah Alameri Date: October 30, 2012 Subject: Is waiver of informed consent in trauma research ethical?
Emanuel et al, E. J. (2000). What makes clinical research ethical?. JAMA: Journal of the American Medical Association,283(20), 2701. Food and Drug Administration. (1996). 21 CFR 50.24. Guidance for Institutional Review Boards, Clinical Investigators and Sponsors. Retrieved from: http://www.fda.gov/downloads/RegulatoryInformation/Guidances/UCM249673.pdf Graham, N., Judy, P., Lois van, O., Ron, M., Tom, R., Jim, C., & Al, H. (2006). Review paper: Consent in resuscitation trials: Benefit or harm for patients and society?. Resuscitation, 70, 360-368. Health Insurance Portability and Accountability Privacy Rule. , 45 C.F.R. pt. 160 (2002). Retrieved from http://www.hhs.gov/ocr/privacy/hipaa/administrative/privacyrule/prdecember2000all8 parts.pdf John C., M. (2006). Informed consent and refusal of treatment: Challenges for emergency physicians. Emergency Medicine Clinics of North America, 24(Ethical Issues in Emergency Medicine), 605-618. Largent, E., Wendler, D., Emanuel, E., & Miller, F. (2010). Is emergency research without initial consent justified?: The consent substitute model. Archives of Internal Medicine, 170(8), 668-674. Lemaire, F. (2007). Emergency research: Only possible if consent is waived?. Current Opinion in Critical Care, 13(2), 122-125. Minio, A., Anderson, R., Fingerhut, L., Boudreault, M., & Warner, M. (2006). Deaths: injuries, 2002. National Vital Statistics Reports: The Centres for Disease Control and Prevention, National Centre for Health Statistics, National Vital Statistics System, 54(10), 1-124. Morrison, C., Horwitz, I. B., & Carrick, M. M. (2009). Ethical and legal issues in emergency research: Barriers to conducting prospective randomized trials in an emergency setting. Journal of Surgical Research, 157(1), 115-122. Newman, J. T., Smart, A., Reese, T. R., Williams, A., & Moss, M. (2012). Surrogate and
George Washington University
ANALYTICAL MEMORANDUM To: Dr. Nasser From: Marwah Alameri Date: October 30, 2012 Subject: Is waiver of informed consent in trauma research ethical?
patient discrepancy regarding consent for critical care research. Critical Care Medicine, 40(9), 2590-2594. Protection of Human Subjects, 45 C.F.R. pt. 46 (2009). Retrieved from http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.html
George Washington University
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- WEBSTER, J.G. Medical Instrumentation: Application and Design. New York: John Wiley & Sons, 1998Document2 pagesWEBSTER, J.G. Medical Instrumentation: Application and Design. New York: John Wiley & Sons, 1998Virgilio MagaldeNo ratings yet
- Farmakoterapi Sistem Pencernaan Diare Konstipasi HepatitisDocument77 pagesFarmakoterapi Sistem Pencernaan Diare Konstipasi HepatitisRefika FahruNo ratings yet
- CME Trunk, Abdomen, and Pressure Sore ReconstructionDocument15 pagesCME Trunk, Abdomen, and Pressure Sore ReconstructionVeronica TomaselloNo ratings yet
- Is Regenerative Medicine Right For Your Condition?: PRP InjectionsDocument2 pagesIs Regenerative Medicine Right For Your Condition?: PRP InjectionsSamuel AnkomaheneNo ratings yet
- NSG 117 PerfusionDocument55 pagesNSG 117 PerfusionAnonymous UJEyEsNo ratings yet
- Lesson Plan in MAPEH (Dagalea)Document4 pagesLesson Plan in MAPEH (Dagalea)Keziah LlenaresNo ratings yet
- Conjoined Twins: Bioethics, Medicine and The Law: ViewpointDocument2 pagesConjoined Twins: Bioethics, Medicine and The Law: ViewpointSulistyawati WrimunNo ratings yet
- Total Gastrectomy ConsentDocument18 pagesTotal Gastrectomy ConsentTanyaNganNo ratings yet
- Cytomegalovirus Infection: Dr. Hendra Purnasidha Bagaswoto, M.SC, Sp.A SMF Anak RSUP Dr. Soeradji Tirtonegoro KlatenDocument40 pagesCytomegalovirus Infection: Dr. Hendra Purnasidha Bagaswoto, M.SC, Sp.A SMF Anak RSUP Dr. Soeradji Tirtonegoro KlatenDonniehh Assassintilldeath NothinglastforeverNo ratings yet
- Lyons Et Al-2017-Periodontology 2000Document4 pagesLyons Et Al-2017-Periodontology 2000Julio César PlataNo ratings yet
- Patient Education and Counseling: Juliana Chen, Luke Gemming, Rhona Hanning, Margaret Allman-FarinelliDocument8 pagesPatient Education and Counseling: Juliana Chen, Luke Gemming, Rhona Hanning, Margaret Allman-FarinelliAlvaro PalominoNo ratings yet
- Drug Study Er MedsDocument12 pagesDrug Study Er MedsJerald S. OlaloNo ratings yet
- Productos Cataloguo Tappa PDFDocument10 pagesProductos Cataloguo Tappa PDFjavier jimenezNo ratings yet
- Physiotherapy For Cardiac SurgeryDocument15 pagesPhysiotherapy For Cardiac SurgeryMuruganNo ratings yet
- 0708 How Investments PatientSurveyDocument10 pages0708 How Investments PatientSurveyRishi jainNo ratings yet
- 03 Klasifikasi Penyakit Dan Keadaan Yang Mempengaruhi Jaringan PeriodontiumDocument16 pages03 Klasifikasi Penyakit Dan Keadaan Yang Mempengaruhi Jaringan PeriodontiumFloba Ika SianturiNo ratings yet
- Materi WS EWS 2018 - Dr. Habibi - ICU ADMISSION CRITERIADocument22 pagesMateri WS EWS 2018 - Dr. Habibi - ICU ADMISSION CRITERIAIndrati TRNo ratings yet
- Kochi Claim FormDocument4 pagesKochi Claim FormRadhika ShenoiNo ratings yet
- MCQ Anaethesia Posting Group 4 2014Document4 pagesMCQ Anaethesia Posting Group 4 2014Law YouNo ratings yet
- UltraMetabolism Guide PDFDocument108 pagesUltraMetabolism Guide PDFMihaela Cristina Munteanu100% (1)
- PCR Testing Centers in The PhilippinesDocument36 pagesPCR Testing Centers in The Philippineskhrayzie bhoneNo ratings yet
- Ichroma II Test Panels 210331 104829Document2 pagesIchroma II Test Panels 210331 104829Sinergy DiagnosticNo ratings yet
- A Textbook of General Practice - 2nd EditionDocument336 pagesA Textbook of General Practice - 2nd Editionstrahiltodorov100% (2)
- The Scoop On Brain Healt Dietary Supplement Products Containing Huperzine ADocument7 pagesThe Scoop On Brain Healt Dietary Supplement Products Containing Huperzine Avasilyi IvanenkoNo ratings yet
- Presentation Resuscitation - Power PointDocument45 pagesPresentation Resuscitation - Power PointRouquia ManzoorNo ratings yet
- 2020 Mcqs Endondontic EmergencyDocument17 pages2020 Mcqs Endondontic Emergencyareej alblowi100% (4)
- High-Risk Prenatal Client - Hiv - AidsDocument20 pagesHigh-Risk Prenatal Client - Hiv - AidsMichael Angelo SeñaNo ratings yet
- 2 - Thyroxine and Treatment of Hypothyroidism - 2019Document8 pages2 - Thyroxine and Treatment of Hypothyroidism - 2019Johanna Bustos NutricionistaNo ratings yet
- Genetic Disorders PDFDocument38 pagesGenetic Disorders PDFEllen Mae PrincipeNo ratings yet
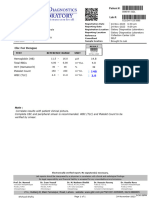
- NormaltestreportDocument1 pageNormaltestreportgalaxydiagnosticlabcclghNo ratings yet