Professional Documents
Culture Documents
OSA Part 3
Uploaded by
Suprit SnOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
OSA Part 3
Uploaded by
Suprit SnCopyright:
Available Formats
Dr.
Supreet Singh Nayyar, AFMC 2012
SLEEP DISORDERED BREATHING (PART 3) Treatment
for more topics, visit www.nayyarENT.com
Non-Surgical therapy for OSAHS
Address co-existent, predisposing conditions Obesity Documented reduction in symptom after weight reduction Degree of improvement has no linear correlation with weight Few may not benefit if co-existent craniofacial abnormalities Life style modification Avoid tobacco /smoking Dietary modification Sleep deprivation Avoiding agents affecting sleep Treat hypothyroidism Mechanical devices (positive airway pressure) Body posture modification Sleeping with head and trunk elevated to 30-60 degree angle to horizontal reduces OSA Lateral decubitus is also effective in reducing episodes (sleep ball) Pharmacological therapy Protriptyline Non-sedating tricyclic antidepressant Increasing tone of airway muscle Statistically significant improvement Side effects : dry mouth, urinary hesitancy, constipation, confusion, ataxia Dose: 30 mg/day Agents with uncertain limited role Serotonin agonists Affects dilators
www.nayyarENT.com
1
Dr. Supreet Singh Nayyar, AFMC 2012
Busiprone Data insufficient Stimulants Amphetamines CVS complication Insufficient data
Continuous Positive Airway Pressure (CPAP)
Indications Mild OSA with EDS Moderate to severe OSA Co-morbidities Many consider it to be mainstay of OSA treatment Mechanism: Acts as pneumatic splint Equipment: Machine provides fixed pressure or vary pressure depending on the presence of apnoeas (Auto CPAP) Mask is nasal or full face, kept in place by Velcro straps Port of exhalation Newer machine small and light so portable Humidifier also available as an optional mode Compliance By 3 years 25-40% stop using CPAP Treatment failure Cost factor o Regular service and maintenance o Change of mask Side effects Claustrophobia Nasal stuffiness Skin abrasions, nasal bridge abrasions Leaks are uncomfortable for eyes Air swallowing if pressure more than esophageal sphincter pressure Pulmonary baro trauma ( very rare) Treatment Failure
www.nayyarENT.com
2
Dr. Supreet Singh Nayyar, AFMC 2012
Surgical management
SURGICAL TREATMENT OPTIONS
Nasal Surgery
1. 2. 3. 4. 5.
Nasal septoplasty Inferior turbinectomy Adenoidectomy Nasal tumor or polyp excision Nasal valve reconstruction
Palatal Surgery
1. 2. 3. 4. 5. 6.
Uvulopalatopharyngoplasty Uvulopalatal flap Tonsillectomy Transpalatal advancement pharyngoplasty Laser-assisted uvulopalatoplasty Palatal radiofrequency
Hypopharyngeal Surgery
1. 2. 3. 4. 5. 6. 7.
Maxillomandibular osteotomy and advancement Mandibular osteotomy with genioglossus advancement Hyoid myotomy and suspension Tongue base radiofrequency Partial glossectomy Lingual tonsillectomy Repose tongue suspension
for more topics, visit www.nayyarENT.com
www.nayyarENT.com
Dr. Supreet Singh Nayyar, AFMC 2012
Indications for surgery
Uvulopalatopharyngoplasty(UPPP) First described by Ikematsu(1950), Fugita popularized in 1985 Principle: Stiffen the soft palate by scarring Increase space behind soft palate Consists of Tonsillectomy Reorientation of the anterior and posterior tonsillar pillars Excision of the uvula and posterior rim of the soft palate. Complications: Nasal regurgitation Swallowing & voice problems Severe post op pain Hemorrhage Laryngospasm
www.nayyarENT.com
Dr. Supreet Singh Nayyar, AFMC 2012
Pulmonary edema, hypoxia Not satisfied post surgery 75-95% short term success Long term 45% Modification: Preserve uvula
Laser-assisted Uvulopalatoplasty(LAUP) Described by Kamami in France in 1993 Principle Stiffen the soft palate Prevent palatal flutter Surgery Local anesthesia on soft palate B/l vertical incision in soft palate followed by partial vaporization of
www.nayyarENT.com
5
Dr. Supreet Singh Nayyar, AFMC 2012
uvula with CO2 Laser Various modification done Complications Low Globus like symptom common Post operative pain
Uvulopalatoplasty
Reversible uvulopalatal flap A, Preoperative palate anatomy B, Uvula is grasped with a forceps and reflected back toward the softhard palate junction; note the muscular crease. C, The mucosa of the oral aspect of the uvula and soft palate in a diamond shape is removed with cold knife dissection; the uvular tip is amputated and the uvular muscle thinned, if necessary D, Trimmed and sutured flap, with the shaded area indicating the location of the tissue before it is repositioned. E, Postoperative appearance, with closure up on the soft palate
Radiofrequency tissue volume reduction/Thermal ablation(RFTVR)
Principle Similar to diathermy Lower temperature, lower current and voltage
www.nayyarENT.com
6
Dr. Supreet Singh Nayyar, AFMC 2012
Insulated probe delivering radiofrequency energy at a frequency of 465 KHz Thermal injury to specific submucosal sites in soft palate causing fibrosis and contraction Introduced into the base-of-tongue tissue under local anesthesia Advantage Day care, LA Less post operative pain Significant improvement reported Good for multi level obstruction Low relapse rate
Mandibular osteotomy and genioglossal advancement
Intraoral approach To enlarge the retrolingual area. The genial tubercle, which is the anterior attachment of the genioglossus muscle, is mobilized by osteotomy The segment is advanced and rotated to allow bony overlap to lock the inner (lingual) surface of the mandible and the geniotubercle at the outer (labial) surface The fragment is fixed at the inferior aspect of the osteotomy with a titanium screw
www.nayyarENT.com
Dr. Supreet Singh Nayyar, AFMC 2012
Other Procedures
Palatal: Z-pharyngoplasty, palatal implants Tongue base RFTVR Laser midline glossectomy to enlarge the retrolingual airway excision of approximately 2.5 5 cm of midline tongue tissue intraoral approach may also require lingual tonsillectomy reduction of the aryepiglottic folds partial epiglottectomy usually combined with a tracheotomy for airway protection Tongue suspension suture Hypoglossal nerve stimulation Lingualplasty. Same procedure as the LMG (laser midline glossectomy) Except that additional tongue tissue is extirpated posteriorly and laterally to the portion removed by LMG Epiglottis epiglottectomy Temporary tracheostomy
Repose tongue suspension.
Intraoral incision is made in the frenulum Titanium screw is placed at the lingual cortex of the geniotubercle of the mandible Permanent suture is passed through the paramedian tongue musculature along the length of the tongue, through the tongue base, and then back through the length of the tongue musculature Then anchored to the screw, pulling the tongue base anteriorly
Hyoid myotomy and suspension
Addresses retrolingual area Can alleviate obstruction caused by redundant lateral pharyngeal tissue or a retrodisplaced epiglottis Horizontal cervical incision over the hyoid bone is preferred Dissection is carried down to the suprahyoid musculature www.nayyarENT.com
8
Dr. Supreet Singh Nayyar, AFMC 2012
Midline hyoid bone is isolated and then advanced over the thyroid ala Secured with two medial and two lateral permanent sutures
Maxillomandibular osteotomy and advancement
Improves retropalatal collapse by stabilizing the superior pharyngeal muscles and widening the nasopharyngeal inlet Also improves retrolingual obstruction by placing the genioglossus muscle under tension, thereby providing more room in the oral cavity for soft tissues and also stabilizing the lateral pharyngeal wall Outer-table cranial bone graft may be necessary, along with arch bar placement (or orthodontic banding) before the osteotomies Usually performed if previous upper airway procedures have not completely relieved the sleep-related obstruction.
Clinical Outcomes
Overall success rate for UPPP 40% With multilevel surgical strategy have achieved 60% when applying strict response criteria 80% have been reported when applying commonly accepted measures of improvement However, the results may be reduced in morbidly obese patients www.nayyarENT.com
9
Dr. Supreet Singh Nayyar, AFMC 2012
Johnson and Chinn achieved a mean reduction of 44.1 points on the RDI (from a preoperative value of 58.7 to a mean postoperative value of 10.5) in patients undergoing UPPP and genioglossal advancement without HM When defining success as a RDI of less than 10, seven out of nine patients (78%) were successfully treated Troell and colleagues[57] reported that seven of 11 patients (63.6%) who underwent a palatopharyngoplasty combined with genioglossus advancement and HM were cured,
with cure defined as a postoperative RDI of less than 10, with resolution of EDS
Oral Appliances
Two basic types of appliances
Mandibular advancement devices Popular Positioning the lower jaw and tongue downward and forward The airway passage is increased Comfortable More effective Tongue repositioners Pulling only the tongue forward and not the entire lower jaw. Teeth, jaw muscles and joints are less affected Less studied A period of consistent nightly wear is required Patient motivation and cooperation essential
for more topics, visit www.nayyarENT.com
www.nayyarENT.com
10
You might also like
- Auditory Processing DisordersDocument3 pagesAuditory Processing DisordersSuprit SnNo ratings yet
- Anaesthesia in Ophthalmology 001Document37 pagesAnaesthesia in Ophthalmology 001pranab2506No ratings yet
- Care of The Surgical Patient-2015 RevisionDocument55 pagesCare of The Surgical Patient-2015 RevisionGilberto Gonzalez100% (1)
- Deep Neck Spaces PDFDocument15 pagesDeep Neck Spaces PDFSuprit SnNo ratings yet
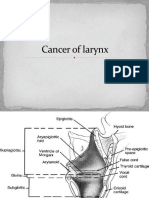
- Cancer of LarynxDocument46 pagesCancer of LarynxVIDYANo ratings yet
- Anaesthesia in Obese PatientsDocument72 pagesAnaesthesia in Obese PatientsPraveen RamasamyNo ratings yet
- Pregnancy TestDocument10 pagesPregnancy TestquerokeropiNo ratings yet
- Epi Brochure (Calalang)Document2 pagesEpi Brochure (Calalang)Nickaela CalalangNo ratings yet
- Obstructive Sleep ApneaDocument49 pagesObstructive Sleep ApneaFiryal BalushiNo ratings yet
- Anaesthesia For Cataract Surgery and Its ComplicationDocument28 pagesAnaesthesia For Cataract Surgery and Its Complicationbala16690No ratings yet
- Adult and Paediatric Oral/nasal-Pharyngeal SuctioningDocument13 pagesAdult and Paediatric Oral/nasal-Pharyngeal SuctioningRuby Dela RamaNo ratings yet
- Surgical Management of Obstructive Sleep Apnea in AdultsDocument30 pagesSurgical Management of Obstructive Sleep Apnea in AdultsJustine NyangaresiNo ratings yet
- Cholesteatoma Part 5 Congenital Cholesteatoma PDFDocument4 pagesCholesteatoma Part 5 Congenital Cholesteatoma PDFSuprit Sn100% (1)
- Organ DonationDocument44 pagesOrgan DonationKlause Kenze Kabil50% (2)
- Maxillary Carcinoma, Nasal Cavity and Paranasal Sinus Malignancy PDFDocument18 pagesMaxillary Carcinoma, Nasal Cavity and Paranasal Sinus Malignancy PDFSuprit Sn100% (2)
- Genioplasty Oral SurgeryDocument45 pagesGenioplasty Oral SurgeryFourthMolar.com100% (2)
- Drooling PDFDocument2 pagesDrooling PDFSuprit SnNo ratings yet
- Difficult AirwayDocument77 pagesDifficult AirwayParvathy R Nair100% (1)
- Drowning - Gary WilliamsDocument48 pagesDrowning - Gary WilliamsFitri Amelia RizkiNo ratings yet
- My Lecture NEMEC Temporal Bone CourseDocument37 pagesMy Lecture NEMEC Temporal Bone CourseAileen Delos Santos-GarciaNo ratings yet
- CSF RhinorrhoeaDocument12 pagesCSF RhinorrhoeaSuprit Sn100% (5)
- Approaches To The SphenoidDocument8 pagesApproaches To The SphenoidSuprit Sn100% (1)
- Functional Endoscopic Sinus Surgery - Overview, Preparation, TechniqueDocument10 pagesFunctional Endoscopic Sinus Surgery - Overview, Preparation, TechniqueHendra SusantoNo ratings yet
- Laryngeal Electromyography Emg Lemg PDFDocument3 pagesLaryngeal Electromyography Emg Lemg PDFSuprit Sn50% (2)
- EPISTAXISDocument25 pagesEPISTAXISSuprit Sn78% (9)
- Postlaryngectomy voice rehabilitation with voice prosthesesFrom EverandPostlaryngectomy voice rehabilitation with voice prosthesesNo ratings yet
- Meatoplasty in CWD PDFDocument7 pagesMeatoplasty in CWD PDFSuprit Sn100% (1)
- PART 4 Coran Pediatric Surgery, 7th Ed PDFDocument593 pagesPART 4 Coran Pediatric Surgery, 7th Ed PDFMaria TudorieNo ratings yet
- OverviewDocument3 pagesOverviewAngela MertesNo ratings yet
- Mandibular Advancement Device & Rapid Maxillary ExpansionDocument35 pagesMandibular Advancement Device & Rapid Maxillary Expansion이상하No ratings yet
- Medical and Surgical ProcedureDocument13 pagesMedical and Surgical Procedureprathamesh patilNo ratings yet
- Septoplasty 111003152845 Phpapp01Document40 pagesSeptoplasty 111003152845 Phpapp01kennitaharyatiNo ratings yet
- Functional Endoscopic Sinus SurgeryDocument3 pagesFunctional Endoscopic Sinus SurgeryDanielicah CruzNo ratings yet
- Gagging: Dr. Sajda A. ElhagDocument41 pagesGagging: Dr. Sajda A. ElhagmarwaNo ratings yet
- Mandibular Positioning Techniques To Improve Sleep Quality in OSA PatientsDocument37 pagesMandibular Positioning Techniques To Improve Sleep Quality in OSA PatientsDR NASIMNo ratings yet
- Fibreoptic IntubationDocument45 pagesFibreoptic IntubationArmaanjeet SinghNo ratings yet
- Hoarseness and Benign Vocal Fold Mucosal DisordersDocument72 pagesHoarseness and Benign Vocal Fold Mucosal DisordersmdNo ratings yet
- Postoperative Care of Oral and Maxillofa PDFDocument10 pagesPostoperative Care of Oral and Maxillofa PDFMashood AhmedNo ratings yet
- Ambulatory and Fast Tracking Anaesthesia: Presentor: Dr. Kumar Moderator: DR - PradeepDocument48 pagesAmbulatory and Fast Tracking Anaesthesia: Presentor: Dr. Kumar Moderator: DR - PradeephidayatiNo ratings yet
- Uvulo Palatal Flap PIIS1043181015000342Document7 pagesUvulo Palatal Flap PIIS1043181015000342barbiemeNo ratings yet
- Surgery and Perioperative Care: AnaestheticsDocument146 pagesSurgery and Perioperative Care: Anaestheticsjames.a.blairNo ratings yet
- Drooling 9905Document24 pagesDrooling 9905Tushar KhuranaNo ratings yet
- ObstructiveSleepApnea DR - BugnnahDocument40 pagesObstructiveSleepApnea DR - BugnnahDr.Sherif BugnahNo ratings yet
- Anesthesia For Maxillofacial ProcedureDocument90 pagesAnesthesia For Maxillofacial ProcedureAnirban Roy100% (1)
- Miringotomi, TimpanoplastiDocument2 pagesMiringotomi, Timpanoplastinad0% (1)
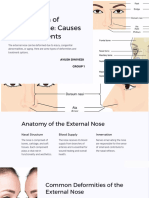
- Introduction-To-Rhinoplasty PPT Ayush DwivediDocument14 pagesIntroduction-To-Rhinoplasty PPT Ayush Dwivedijqpwzcg8xrNo ratings yet
- UntitledDocument25 pagesUntitledmohammed SamarNo ratings yet
- GAG ReflexDocument4 pagesGAG Reflexdrgayen6042No ratings yet
- Comprehensive Management of Cleft: Presented By: Dewi Nur Khotimah G99142036 Aprillio Bagas Sriwisnu G99152099Document32 pagesComprehensive Management of Cleft: Presented By: Dewi Nur Khotimah G99142036 Aprillio Bagas Sriwisnu G99152099Pramitha YustiaNo ratings yet
- Case Selection, Diagnosis & Treament Plan For Dental ImplantDocument57 pagesCase Selection, Diagnosis & Treament Plan For Dental ImplantChirag PatelNo ratings yet
- And After The Procedure) : 1. Polysomnography / Sleep TestDocument9 pagesAnd After The Procedure) : 1. Polysomnography / Sleep Testkaren carpioNo ratings yet
- ENT - Adult Septo-Turbs InfoDocument2 pagesENT - Adult Septo-Turbs InfoBayuLesmonoNo ratings yet
- Post Burn Contracture NeckDocument17 pagesPost Burn Contracture NeckcardiacanesthesiaNo ratings yet
- Surgical Treatment in MeniereDocument4 pagesSurgical Treatment in MeniereSyazana SaadNo ratings yet
- General Principles of Periodontal SurgeryDocument10 pagesGeneral Principles of Periodontal SurgeryPurwana NasirNo ratings yet
- Imp in Compromised CndnsDocument34 pagesImp in Compromised CndnsswatiNo ratings yet
- Anesthesia For Maxillofacial ProcedureDocument90 pagesAnesthesia For Maxillofacial ProcedureShalini Thakur Dubey0% (2)
- Modified 2021 FALL WITH ANSWERDocument8 pagesModified 2021 FALL WITH ANSWERyasser farhanNo ratings yet
- pRESENTASI TURBINATESDocument50 pagespRESENTASI TURBINATESPeter SalimNo ratings yet
- Airway Management LectureDocument113 pagesAirway Management LectureAnita Krisnawaty NainggolanNo ratings yet
- Airway Management in TransportDocument46 pagesAirway Management in TransportArtha PutuNo ratings yet
- Medically Compromised Patients in Prosthodontics - 818 (Autosaved)Document22 pagesMedically Compromised Patients in Prosthodontics - 818 (Autosaved)Suraj ShahNo ratings yet
- Upper Airway Hypoglossal Nerve Stimulation - 2019 - Atlas of The Oral and MaxiDocument6 pagesUpper Airway Hypoglossal Nerve Stimulation - 2019 - Atlas of The Oral and Maxilaljadeff12No ratings yet
- Tutorial 2 - Intra-Op ManagementDocument4 pagesTutorial 2 - Intra-Op ManagementSNo ratings yet
- Surgical Approaches To Temporomandibular JointDocument8 pagesSurgical Approaches To Temporomandibular Jointmishu00No ratings yet
- Surgical Maxillomandibular AdvancementDocument6 pagesSurgical Maxillomandibular Advancementdrzana78No ratings yet
- Tonsillectomy and Pharyngoplasty: Tissue-Preserving TechniquesDocument6 pagesTonsillectomy and Pharyngoplasty: Tissue-Preserving Techniqueslaljadeff12No ratings yet
- General Anesthesia: IntubationDocument44 pagesGeneral Anesthesia: IntubationMiezu CosminNo ratings yet
- Maxillofascial Surgery AnesthesiaDocument62 pagesMaxillofascial Surgery AnesthesiaHossam atefNo ratings yet
- Posterior Tongue Tie - : Case History #3Document5 pagesPosterior Tongue Tie - : Case History #3Галина НестероваNo ratings yet
- Oral Manifestations of Denture AbuseDocument53 pagesOral Manifestations of Denture AbuseBharanija100% (2)
- Asian Rhinoplasty (Noselift) - Cosmetic Surgery in The PhilippinesDocument1 pageAsian Rhinoplasty (Noselift) - Cosmetic Surgery in The Philippinesdalemd29No ratings yet
- Exercício Vad DR Andre Ferreira Training Cediva Denia November 2023Document5 pagesExercício Vad DR Andre Ferreira Training Cediva Denia November 2023cedivadeniaNo ratings yet
- Dental Sleep Practice ArticleDocument3 pagesDental Sleep Practice ArticleJet AimeNo ratings yet
- Snoring, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandSnoring, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Inferior Turbinate Hypertrophy PDFDocument3 pagesInferior Turbinate Hypertrophy PDFSuprit SnNo ratings yet
- LPR by Dr. SS NayyarDocument45 pagesLPR by Dr. SS NayyarSuprit Sn100% (1)
- Laryngo Tracheo Bronchial Foreign Bodies .PPT With Voice Over and Case Presentation of Use of Optical Grabbing ForcepsDocument46 pagesLaryngo Tracheo Bronchial Foreign Bodies .PPT With Voice Over and Case Presentation of Use of Optical Grabbing ForcepsSuprit Sn100% (1)
- Nasopharyngeal Carcinoma PDFDocument11 pagesNasopharyngeal Carcinoma PDFSuprit SnNo ratings yet
- Dural Venous Sinuses PDFDocument3 pagesDural Venous Sinuses PDFSuprit SnNo ratings yet
- Differential Diagnosis Mass Nasal Cavity PDFDocument2 pagesDifferential Diagnosis Mass Nasal Cavity PDFSuprit SnNo ratings yet
- Cysts of Maxilla PDFDocument1 pageCysts of Maxilla PDFSuprit SnNo ratings yet
- Facial Pain PDFDocument4 pagesFacial Pain PDFSuprit SnNo ratings yet
- Cholesteatoma Part 2 Relevant Anatomy PDFDocument3 pagesCholesteatoma Part 2 Relevant Anatomy PDFSuprit SnNo ratings yet
- Computer Aided Facial AssessmentDocument2 pagesComputer Aided Facial AssessmentSuprit Sn100% (1)
- Consumer Protection Act in Medicine PDFDocument3 pagesConsumer Protection Act in Medicine PDFSuprit SnNo ratings yet
- Cochlear ImplantationDocument11 pagesCochlear ImplantationSuprit Sn100% (3)
- Cholesteatoma Part 9 - Reconstruction of The Mastoid Cavity PDFDocument4 pagesCholesteatoma Part 9 - Reconstruction of The Mastoid Cavity PDFSuprit SnNo ratings yet
- Cricoarytenoid Joint DislocationDocument3 pagesCricoarytenoid Joint DislocationSuprit Sn100% (1)
- Thyroid StormDocument3 pagesThyroid StormSuprit SnNo ratings yet
- Chevalier JacksonDocument3 pagesChevalier JacksonSuprit SnNo ratings yet
- Cervical OesophagotomyDocument4 pagesCervical OesophagotomySuprit SnNo ratings yet
- Chemoprevention Head Neck MalignanciesDocument3 pagesChemoprevention Head Neck MalignanciesSuprit Sn100% (2)
- Assr, Vemp, VNG, OaeDocument8 pagesAssr, Vemp, VNG, OaeSuprit Sn100% (1)
- Capno GraphyDocument2 pagesCapno GraphySuprit SnNo ratings yet
- D - Guideline On Number of Embryos To Transfer During IVF ICSI - Stakeholder ReviewDocument135 pagesD - Guideline On Number of Embryos To Transfer During IVF ICSI - Stakeholder Reviewshobhitbhargava39No ratings yet
- The Relevance of Attachment Theory For PDocument52 pagesThe Relevance of Attachment Theory For PVeera Balaji KumarNo ratings yet
- Basic PhotographyDocument3 pagesBasic Photographyapi-461238862No ratings yet
- Part B - Health Facility Briefing & Design 55Document15 pagesPart B - Health Facility Briefing & Design 55Mudita PiseNo ratings yet
- AMG Curs 3Document2 pagesAMG Curs 3Maria PalNo ratings yet
- Irna - Existing RS Type DDocument17 pagesIrna - Existing RS Type DUcrit TralalaNo ratings yet
- In Favour of An Investigation of The Relationship Between Vitamin B12 Deficiency and HIV InfectionDocument3 pagesIn Favour of An Investigation of The Relationship Between Vitamin B12 Deficiency and HIV InfectionPJ 123No ratings yet
- Read The Passage and Answer The Questions: by An Old Age"Document1 pageRead The Passage and Answer The Questions: by An Old Age"Hesen Gozelov100% (1)
- Classification, Pathophysiology, Diagnosis and Management of DiabetesDocument19 pagesClassification, Pathophysiology, Diagnosis and Management of DiabeteswakhidrizkaNo ratings yet
- QP 04Document15 pagesQP 04zakwanmustafaNo ratings yet
- The Kaohsiung J of Med Scie - 2013 - Tsai - Pyoderma Gangrenosum Intractable Leg Ulcers in Sjogren S SyndromeDocument2 pagesThe Kaohsiung J of Med Scie - 2013 - Tsai - Pyoderma Gangrenosum Intractable Leg Ulcers in Sjogren S SyndromeAsad KakarNo ratings yet
- Spinal Cord InjuryDocument28 pagesSpinal Cord InjuryLouie John AbilaNo ratings yet
- S2-Epid - Main Disese (3) - Influenza - Student - 2023Document48 pagesS2-Epid - Main Disese (3) - Influenza - Student - 2023Syahrul SanmasNo ratings yet
- Community Health Nursing I (Individual and Family) : Prepared By: Mrs. Lavinia T. Malabuyoc, MAN, R.NDocument48 pagesCommunity Health Nursing I (Individual and Family) : Prepared By: Mrs. Lavinia T. Malabuyoc, MAN, R.NLerma Pagcaliwangan100% (1)
- Allergic Rhinitis in ChildrenDocument7 pagesAllergic Rhinitis in ChildrenTina MorleyNo ratings yet
- Guideline of Urolithiasis PDFDocument34 pagesGuideline of Urolithiasis PDFMelia IndasariNo ratings yet
- Ocular Features in A Large Cohort of Indians With.5Document7 pagesOcular Features in A Large Cohort of Indians With.5Sushma NNo ratings yet
- Biomedical Waste Management Colour Coding For BeginnersDocument3 pagesBiomedical Waste Management Colour Coding For BeginnersMotherterrasa VocationalNo ratings yet
- Impaction Case-history-NAGARAJ TANNERUDocument8 pagesImpaction Case-history-NAGARAJ TANNERUmedicmayaNo ratings yet
- 2020 09 - OCME Overdose ReportDocument10 pages2020 09 - OCME Overdose ReportJoe EskenaziNo ratings yet
- Questions From The Section On General and Special VirologyDocument21 pagesQuestions From The Section On General and Special VirologytiffylolaNo ratings yet
- ECG Taking Checklist-Ez VersionDocument2 pagesECG Taking Checklist-Ez VersionKeisha Bartolata100% (1)
- Glossary and Acronyms of FreedivingDocument2 pagesGlossary and Acronyms of FreedivingIvo XNo ratings yet
- Referensi Referat ObgynDocument10 pagesReferensi Referat ObgynFaradiba NoviandiniNo ratings yet
- pedCAT BrochureDocument12 pagespedCAT BrochureVinti Singh100% (1)