Professional Documents
Culture Documents
Decreased Cardiac Output
Uploaded by
Cristina L. JaysonOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Decreased Cardiac Output
Uploaded by
Cristina L. JaysonCopyright:
Available Formats
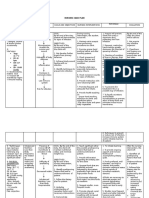
Nursing Care Plans Problem: Decreased Cardiac Output Nursing Diagnosis: Decreased cardiac output related to fluid imbalances
affecting circulating volume myocardial workload and systemic vascular resistance (SVR) alterations in rate, rhythm, cardiac conduction (electrolyte imbalances, hypoxia) accumulation of toxins (urea), soft-tissue calcification (deposition of calcium phosphate) Taxonomy: Activity-Exercise Pattern Cause Analysis: Loss of excretory renal function that may lead to decreased phosphate excretion and calcium absorption causes tissue calcifications. Decreased excretion of nitrogenous wastes accumulate urea in the system. Decreased sodium reabsorption in tubule affects fluid balances. Losses of nonexcretory renal function of the kidney will lead to failure to produce erythropoietin. Thus leads to anemia. In order to pump more blood into the body, the heart muscle requires more oxygenated blood to meet own needs. Calcifications of the involuntary muscles affects contractility thus affects volume of blood ejected per minute (p884,1435, 1441 Medical-Surgical Nursing by Black et.al) Cues Goal Nursing Intervention Rationale Evaluation increased heart rate dysrhythmias changes in BP (hypotension/hyper tension) extra heart sounds Diminished peripheral pulses Diaphoresis Chest pain Edema
STO: After 2 hrs of effective nursing intervention, patient would be able to become knowledgeable and knowledgeable about the diagnostic tests he will undergo. LTO: After 8 hrs of effective nursing interventions, patient would be able to maintain cardiac output as evidenced by BP and heart rate within patients normal range; peripheral pulses strong and equal with prompt capillary refill time.
Independent Auscultate heart and lung sounds. Evaluate presence of peripheral edema/vascular congestion and reports of dyspnea. Assess presence/degree of hypertension: monitor BP; note postural changes, e.g., sitting, lying, standing. S3/S4 heart sounds with muffled tones, tachycardia, irregular heart rate, tachypnea, dyspnea, crackles, wheezes, and edema/jugular distension suggest HF. Significant hypertension can occur because of disturbances in the reninangiotensin-aldosterone system (caused by renal dysfunction). Although hypertension is common, orthostatic hypotension may occur because of intravascular fluid deficit, response to effects of antihypertensive medications, or uremic pericardial tamponade. Although hypertension and chronic HF may cause MI, approximately half of CRF patients on dialysis develop pericarditis, potentiating risk of pericardial effusion/tamponade. Presence of sudden hypotension, paradoxic pulse, narrow pulse pressure,
Investigate reports of chest pain, noting location, radiation, severity (010 scale), and whether or not it is intensified by deep inspiration and supine position. Evaluate heart sounds (note friction rub), BP, peripheral pulses, capillary refill, vascular congestion, temperature, and
sensorium/mentation.
diminished/absent peripheral pulses, marked jugular distension, pallor, and a rapid mental deterioration indicate tamponade, which is a medical emergency. Weakness can be attributed to HF and anemia.
Assess activity level, response to activity. Collaborative Monitor laboratory/diagnostic studies, e.g.: Electrolytes (potassium, sodium, calcium, magnesium), BUN/Cr; Chest x-rays.
Imbalances can alter electrical conduction and cardiac function. Useful in identifying developing cardiac failure or soft-tissue calcification. Reduces systemic vascular resistance and/or renin release to decrease myocardial workload and aid in prevention of HF and/or MI. Reduction of uremic toxins and correction of electrolyte imbalances and fluid overload may limit/prevent cardiac manifestations, including hypertension and pericardial effusion. Accumulation of fluid within pericardial sac can compromise cardiac filling and myocardial contractility, impairing cardiac output and potentiating risk of cardiac arrest.
Administer antihypertensive drugs, e.g., prazosin (Minipress), captopril (Capoten), clonidine (Catapres), hydralazine (Apresoline). Prepare for dialysis.
Assist with pericardiocentesis as indicated.
You might also like
- HAAD ReviewerDocument35 pagesHAAD ReviewerSydRey92% (24)
- Case Presentation On Antepartum Hypertention IDocument18 pagesCase Presentation On Antepartum Hypertention IJoule PeirreNo ratings yet
- Nursing Care Plan (Compartment Sydnrome)Document6 pagesNursing Care Plan (Compartment Sydnrome)Zyiv BalogalNo ratings yet
- Nursing Interventions for SchizophreniaDocument1 pageNursing Interventions for SchizophreniaTalTal Balcera Beniten100% (1)
- Annex A. ChecklistDocument2 pagesAnnex A. ChecklistroseannurakNo ratings yet
- CHD With NCPDocument10 pagesCHD With NCPJohanna Kirsten F. DaguioNo ratings yet
- Propranolol, Prophylactic Warfarin, Low Molecular Weight Heparin (LMWH), Furosemide, AntibioticsDocument8 pagesPropranolol, Prophylactic Warfarin, Low Molecular Weight Heparin (LMWH), Furosemide, AntibioticsArlyn MarcelinoNo ratings yet
- Decreased Cardiac OutputDocument3 pagesDecreased Cardiac OutputRizalyn QuindipanNo ratings yet
- NCPDocument9 pagesNCPLeolene Grace BautistaNo ratings yet
- Case StudyDocument34 pagesCase StudyBSNNursing101No ratings yet
- Nursing Care Plan WeeblyDocument8 pagesNursing Care Plan Weeblyapi-277498943No ratings yet
- St. Anthony's Nursing Care Plan for Acute Chest PainDocument1 pageSt. Anthony's Nursing Care Plan for Acute Chest PainjoegeNo ratings yet
- NCP MiDocument4 pagesNCP MiPitaca Madiam Annabehl PaulNo ratings yet
- CarePlan #2Document3 pagesCarePlan #2Monika StasiakNo ratings yet
- Impaired Breathing PatternDocument1 pageImpaired Breathing PatternHanya Bint PotawanNo ratings yet
- Decreased Cardiac Output RM 7Document9 pagesDecreased Cardiac Output RM 7api-283470660No ratings yet
- NCP H MoleDocument6 pagesNCP H MoleMina RacadioNo ratings yet
- NCP Knowledge Deficit PDFDocument2 pagesNCP Knowledge Deficit PDFskylertNo ratings yet
- Nursing Care Plan. HypertensionDocument2 pagesNursing Care Plan. HypertensionKiara Shanelle Posadas AbrioNo ratings yet
- NCP Ineffective Cardiopulmonary PerfusionDocument3 pagesNCP Ineffective Cardiopulmonary PerfusionjamiemapanaoNo ratings yet
- Acute Pain SCMCDocument2 pagesAcute Pain SCMCWik Wik PantuaNo ratings yet
- NCP - Decreased Cardiac OutputDocument3 pagesNCP - Decreased Cardiac OutputIzza DeloriaNo ratings yet
- Rufino, Leslie Kriztel S. BSN 3-2 Group 1Document6 pagesRufino, Leslie Kriztel S. BSN 3-2 Group 1Deinielle Magdangal RomeroNo ratings yet
- NCP Activity IntoleranceDocument3 pagesNCP Activity IntoleranceJopaii TanakaNo ratings yet
- NCP AneurysmDocument4 pagesNCP AneurysmJanielle Christine Monsalud100% (1)
- Nursing Care Plan FinalDocument16 pagesNursing Care Plan FinalErickson OcialNo ratings yet
- NCPDocument10 pagesNCPNefre Dayap DarrocaNo ratings yet
- Nursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveDocument2 pagesNursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveFreisanChenMandumotanNo ratings yet
- Drug StudyDocument20 pagesDrug StudydjanindNo ratings yet
- Potential Nursing Care Plan for SchizophreniaDocument1 pagePotential Nursing Care Plan for SchizophreniaopxNo ratings yet
- Acute Cardiac Pain Management GuideDocument31 pagesAcute Cardiac Pain Management Guidejan100% (1)
- Decreased Cardiac Output FinalDocument2 pagesDecreased Cardiac Output FinalSandraDeeNo ratings yet
- NCPDocument7 pagesNCPMarius Clifford BilledoNo ratings yet
- General ObjectivesDocument1 pageGeneral ObjectivesErwin DegraciaNo ratings yet
- Cues Nursing Diagnosis Scientific Rationale Objectives Nursing Interventions Rationale EvaluationDocument8 pagesCues Nursing Diagnosis Scientific Rationale Objectives Nursing Interventions Rationale EvaluationMa Virginia Nathalia CreerNo ratings yet
- Intracranial HemorrhageDocument41 pagesIntracranial Hemorrhagedoctormussieaberra100% (1)
- Myocardial Infarction Concept MapDocument7 pagesMyocardial Infarction Concept Mapkarelclarke629280% (5)
- NCP AidsDocument16 pagesNCP AidstferdianingsihNo ratings yet
- NCPDocument5 pagesNCPSheana TmplNo ratings yet
- Chest Pain Care PlanDocument2 pagesChest Pain Care Planapi-545292605No ratings yet
- HIV Case Study: Priority Nursing Diagnoses and CareDocument3 pagesHIV Case Study: Priority Nursing Diagnoses and CarechoobiNo ratings yet
- Managing Hypertension to Prevent ComplicationsDocument10 pagesManaging Hypertension to Prevent ComplicationsArabylle Maranca AbuelNo ratings yet
- NCPDocument3 pagesNCPArien CaleonNo ratings yet
- Nursing Care Plan: Precipitating FactorDocument8 pagesNursing Care Plan: Precipitating FactorJe Zal100% (1)
- Nursing Care Plan for Alcohol Withdrawal AnxietyDocument5 pagesNursing Care Plan for Alcohol Withdrawal Anxietykuro hanabusaNo ratings yet
- NCP-Septic Shock (Acute Pain)Document3 pagesNCP-Septic Shock (Acute Pain)Ted anadiloNo ratings yet
- NCP Tissue PerfusionDocument4 pagesNCP Tissue PerfusionLisa Tandog100% (1)
- Nursing Care PlanDocument3 pagesNursing Care PlanJayalakshmi David50% (2)
- Date and Time: Nursing Care Plan (NCP)Document3 pagesDate and Time: Nursing Care Plan (NCP)Deanne Carla DalilisNo ratings yet
- Metabolism Case StudiesDocument3 pagesMetabolism Case StudiesEpoy Bantawig0% (1)
- Nursing Care for Pleuritic Chest PainDocument1 pageNursing Care for Pleuritic Chest PainAira AlaroNo ratings yet
- ASSESSMENT EXPLANATION OF THE OBJECTIVES NURSING INTERVENTIONS RATIONALE EVALUATIONDocument5 pagesASSESSMENT EXPLANATION OF THE OBJECTIVES NURSING INTERVENTIONS RATIONALE EVALUATIONRussel SantosNo ratings yet
- Pleural Effusion: Bukidnon State University City of MalaybalayDocument49 pagesPleural Effusion: Bukidnon State University City of MalaybalayKarima JonesNo ratings yet
- Decrease Cardiac OutputDocument6 pagesDecrease Cardiac OutputGerardeanne ReposarNo ratings yet
- CVD Pt Comm ImproveDocument12 pagesCVD Pt Comm ImproveRaphael FranciscoNo ratings yet
- NCP Ineffective Tissue PerfusionDocument2 pagesNCP Ineffective Tissue PerfusionYasminGianneDeOcampoBarizoNo ratings yet
- Ccu Cad NCPDocument5 pagesCcu Cad NCPheyyymeeeNo ratings yet
- NCP Intra FinalDocument7 pagesNCP Intra FinalRoxanne Ganayo ClaverNo ratings yet
- Impaired Tissue PerfusionDocument2 pagesImpaired Tissue PerfusionLyka Mae Imbat - PacnisNo ratings yet
- Cardiac Failure & Myocardial Infarction GuideDocument6 pagesCardiac Failure & Myocardial Infarction GuideDaniel GeduquioNo ratings yet
- Systolic Dysfunction:: Types of Heart FailureDocument13 pagesSystolic Dysfunction:: Types of Heart FailureElisabeth F. OjhaNo ratings yet
- Individual Therapy Key PointsDocument9 pagesIndividual Therapy Key PointsCristina L. JaysonNo ratings yet
- HelloDocument1 pageHelloCristina L. JaysonNo ratings yet
- FBDocument1 pageFBCristina L. JaysonNo ratings yet
- May 2014 NLE Rooms CDODocument71 pagesMay 2014 NLE Rooms CDOCoolbuster.NetNo ratings yet
- 1 STPRCDocument1 page1 STPRCCristina L. JaysonNo ratings yet
- PRC TinaDocument4 pagesPRC TinaCristina L. JaysonNo ratings yet
- OooDocument1 pageOooCristina L. JaysonNo ratings yet
- 3 RDDocument1 page3 RDCristina L. JaysonNo ratings yet
- Mindanao Sanitarium Nursing ClinicalsDocument1 pageMindanao Sanitarium Nursing ClinicalsCristina L. JaysonNo ratings yet
- New Bon-NleDocument3 pagesNew Bon-NleCristina L. JaysonNo ratings yet
- Medical Sources BibliographyDocument1 pageMedical Sources BibliographyCristina L. JaysonNo ratings yet
- Normal Anatomy and PhysiologyDocument8 pagesNormal Anatomy and PhysiologyCristina L. JaysonNo ratings yet
- CorrectionsDocument4 pagesCorrectionsCristina L. JaysonNo ratings yet
- Diagnostic TestsDocument11 pagesDiagnostic TestsCristina L. JaysonNo ratings yet
- References For Drug Study and Diagnostic TestsDocument2 pagesReferences For Drug Study and Diagnostic TestsCristina L. JaysonNo ratings yet
- Diagnostic TestsDocument11 pagesDiagnostic TestsCristina L. JaysonNo ratings yet
- Nursing HistoryDocument1 pageNursing HistoryCristina L. JaysonNo ratings yet
- NCPDocument10 pagesNCPCristina L. JaysonNo ratings yet
- 1st Phase ReportDocument42 pages1st Phase ReportCristina L. JaysonNo ratings yet
- PerosDocument5 pagesPerosCristina L. JaysonNo ratings yet
- 634379489751247500Document32 pages634379489751247500Cristina L. JaysonNo ratings yet
- Phytoplankton Data DipsinDocument125 pagesPhytoplankton Data DipsinCristina L. JaysonNo ratings yet
- GordonsDocument3 pagesGordonsCristina L. JaysonNo ratings yet
- Grand Case Presentation InformationDocument7 pagesGrand Case Presentation InformationCristina L. JaysonNo ratings yet
- Project Contract For Phyto Ra-2Document1 pageProject Contract For Phyto Ra-2Cristina L. JaysonNo ratings yet
- IrisDocument4 pagesIrisYazmin Vasquez BarreraNo ratings yet
- Final DefenseDocument16 pagesFinal DefenseCristina L. JaysonNo ratings yet
- Project Contract For Phyto Ra-2Document1 pageProject Contract For Phyto Ra-2Cristina L. JaysonNo ratings yet
- 3vital Information: Year) - BSED BioDocument3 pages3vital Information: Year) - BSED BioCristina L. JaysonNo ratings yet
- Figure 1. New Criteria For AKI Diagnosis Are Displayed. in Order To Diagnose AKIDocument8 pagesFigure 1. New Criteria For AKI Diagnosis Are Displayed. in Order To Diagnose AKIMayra Alejandra Prada SerranoNo ratings yet
- BuratDocument5 pagesBuratFreya AvellanoNo ratings yet
- How to treat and prevent breast engorgementDocument1 pageHow to treat and prevent breast engorgementkurniaNo ratings yet
- Career Map - DoctorDocument7 pagesCareer Map - DoctorAdityaNo ratings yet
- Cardiac Case Study NDDocument11 pagesCardiac Case Study NDapi-313165458No ratings yet
- Private Practice and Public School Speech Therapy Options in AustinDocument2 pagesPrivate Practice and Public School Speech Therapy Options in Austiniese027No ratings yet
- Asama PosterDocument1 pageAsama Postershuvojit moulikNo ratings yet
- Risk Prediction Model for Heart Failure in DiabetesDocument20 pagesRisk Prediction Model for Heart Failure in DiabetesjamesboendNo ratings yet
- Competitor AnalysisDocument30 pagesCompetitor AnalysisMukulNo ratings yet
- Role of CPAP in ICUDocument21 pagesRole of CPAP in ICUheriNo ratings yet
- The Pelvic Floor and Core ExercisesDocument4 pagesThe Pelvic Floor and Core ExercisesJeffrey PeekoNo ratings yet
- Comparative-Study-Of-Four-Methods-Of-Clinical-Estimation-Of-Fetal-Weight 2Document9 pagesComparative-Study-Of-Four-Methods-Of-Clinical-Estimation-Of-Fetal-Weight 2Abegail Fermanejo-GeneraoNo ratings yet
- EMT Training at Mansion Mandiri HotelDocument4 pagesEMT Training at Mansion Mandiri Hotelyuna triazNo ratings yet
- Treatment of Endometriosis in Women Desiring FertilityDocument23 pagesTreatment of Endometriosis in Women Desiring FertilityVaisnavi Muthoovaloo67% (3)
- Vital Signs ChecklistDocument21 pagesVital Signs ChecklistJapsay Francisco GranadaNo ratings yet
- Antimicrobial Activity of Disinfectants Commonly Used in The Food Industry in MexicoDocument6 pagesAntimicrobial Activity of Disinfectants Commonly Used in The Food Industry in MexicoJoel CarinoNo ratings yet
- SENCHS Joins The Philippine Dengue AwarenessDocument3 pagesSENCHS Joins The Philippine Dengue AwarenessFhikery ArdienteNo ratings yet
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary DetailsAshok KumarNo ratings yet
- Complete Genetics Disease ChartDocument14 pagesComplete Genetics Disease ChartJames FlanneryNo ratings yet
- Ch.12 Getting the measure of hormones講義Document7 pagesCh.12 Getting the measure of hormones講義邱小瀧No ratings yet
- Biosure RGDocument2 pagesBiosure RGJuan Martinez Del AngelNo ratings yet
- Fetal Assessment DRDocument1 pageFetal Assessment DRMicah Lou CalambaNo ratings yet
- 2013 Pankaj R BodadeDocument8 pages2013 Pankaj R BodadeGeorge StoicaNo ratings yet
- Nice Neotech - Accessories - 20Document1 pageNice Neotech - Accessories - 20David Gnana DuraiNo ratings yet
- Comparison of Bupivacaine-Dexmedetomidine VS Bupivacaine-Fentanyl VS Bupivacaine - Saline For Unilateral Spinal Anaesthesia in Lower Limb SurgeryDocument9 pagesComparison of Bupivacaine-Dexmedetomidine VS Bupivacaine-Fentanyl VS Bupivacaine - Saline For Unilateral Spinal Anaesthesia in Lower Limb SurgeryIJAR JOURNALNo ratings yet
- Chronology of Human Dentition & Tooth Numbering SystemDocument54 pagesChronology of Human Dentition & Tooth Numbering Systemdr parveen bathla100% (4)
- 4 - Tracheostomy Care and SuctioningDocument4 pages4 - Tracheostomy Care and SuctioningABEGAIL BALLORANNo ratings yet
- Eclampsia Guidelines FINAL Ratified MCYP SG Sept20 15Document20 pagesEclampsia Guidelines FINAL Ratified MCYP SG Sept20 15Grigore PopaNo ratings yet
- Impaired Gas Exchange NCPDocument1 pageImpaired Gas Exchange NCPCj AlconabaNo ratings yet