Professional Documents
Culture Documents
Lecture 62: Dr. Cohen, Clinical Correlations Respiratory Distress in
Uploaded by
mcwnotes0 ratings0% found this document useful (0 votes)
102 views3 pages 37 weeks gestational age still have higher morbity rate than if allowed to go to full term of 42 wks. Risk factors include low socioeconomic status, inadequate prenatal care, poor nutrition, poor education and intercurrent or untreated illness or infection. Apnea (typically central and obstructive), IVH (interventricular hemorrhage), infections, hypothermia, metabolic (hypercalcemic, low blood glucose, etc), GI,
Original Description:
Original Title
Lecture 62: Dr. Cohen, Clinical Correlations Respiratory Distress In
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document 37 weeks gestational age still have higher morbity rate than if allowed to go to full term of 42 wks. Risk factors include low socioeconomic status, inadequate prenatal care, poor nutrition, poor education and intercurrent or untreated illness or infection. Apnea (typically central and obstructive), IVH (interventricular hemorrhage), infections, hypothermia, metabolic (hypercalcemic, low blood glucose, etc), GI,
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
102 views3 pagesLecture 62: Dr. Cohen, Clinical Correlations Respiratory Distress in
Uploaded by
mcwnotes 37 weeks gestational age still have higher morbity rate than if allowed to go to full term of 42 wks. Risk factors include low socioeconomic status, inadequate prenatal care, poor nutrition, poor education and intercurrent or untreated illness or infection. Apnea (typically central and obstructive), IVH (interventricular hemorrhage), infections, hypothermia, metabolic (hypercalcemic, low blood glucose, etc), GI,
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
Lecture 62: Dr.
Cohen, Clinical Correlations
Respiratory Distress in a Newborn
• Respiratory Distress Case #1:
– 30 wk gestation newborn in respiratory distress
– Exam reveals premature baby with no abnormalities except lung distress
• Prematurity:
– < 37 weeks gestational age (however 37-38 wks still have higher morbity rate
than if allowed to go to full term of 42 wks)
– Risk factors include low socioeconomic status, inadequate prenatal care, poor
nutrition, poor education and intercurrent or untreated illness or infection
– Complications include RDS (respiratory distress syndrome), apnea (typically
central and obstructive), IVH (interventricular hemorrhage), infections,
hypothermia, metabolic (hypercalcemic, low blood glucose, etc), GI, renal, and
hyperbilirubinemia
• RDS:
– Common cause of morbidity
– Male predominance
– Low gestational age (almost 100% at 25 wks, doesn't reach 0% until over 38
weeks)
– Maternal diabetes
– Perinatal asphyxia
– Caused by a decreased production and secretion of surfactant
– Failure to develop FRC and alveoli tend to collapse
– Surfactant synthesis depends on pH, temp and perfusion
– Hypoxia, asphyxia, hypovolemia and cold may worsen condition
– Atelectasis (collapse of alveoli) makes lungs less compliant
– Increased work of breathing
– Ventilation/Perfusion mismatches - hypoxia
• 2 Causes of RDS:
– Fetal Lung Development
Pseudoglandular Stage (7-17 wk gestation): branching that yields fetal
lung
Canalicular Stage (16-25 wk): pre-viable lung becomes potentially
viable, development of air-blood barrier, development of Type II cells
and beginning of surfactant production
Saccular and Alveolar Stages (25 wks): final branching, potential
increase in lung volume for gas exchange *POTENTIAL FOR VIABLE
BABY
Surface area and lung volume increase exponentially after 25 wks
– Surfactant
Made by type II alveolar cells
Made of phosphatidylcholine and SP-A, B, C and D
SP-B is required for life
Has polar and non-polar end
Alveolus wants to collapse due to water surface tension however
surfactant acts by reducing surface tension of water
Laplace’s Law (decrease T thereby decreasing P)
Saline lungs would eliminate air-water interface and therefore less
pressure is required
• Vicious circle
– Clinical manifestations:
Signs occur within minutes of birth
Tachypnea respiratory rate
• mechanical pulmonary dysfunction, acid-base imbalance, blood
gas abnormalities
• minimize work of breathing by adjusting resp. rate
• Pts w/ stiff lungs breath fast and shallow
• Pts w/ increased resistance breath slower and deeper
Grunting
• Expiration through a partially closed vocal cord
• Produces an elevated transpulmonary pressure in the absence
of airflow
V/Q ration is enhances b/c of increased airway pressure and lung
volume
Intercostal and subcostal retractions
• Retractions are caused by use of accessory muscles of
respiration
• Due to decreased compliance
Nasal flaring
• Enlargement of nostrils during inspiration to reduce resistance
(by power of 4)
• Nasal resistance contributes to airway resistance
• Poiseuille’s Law
Cyanosis
• Fick's Law of Diffusion
• Increased membrane thickness decreases the rate of diffusion
• What do you see?
– Breath sounds may be diminished or normal; they may havea harsh quality or
fine rales or crackles
• Natural Course
– Progressive worsening or cyanosis and distress
– BP falls
– Fatigue, cyanosis and pallor increase
– Apnea and irregular resp appear
– Acidosis
– Peaks at 3 days w/ gradual improvement if infant survives
• Diagnosis
– CXR (Chest X-Ray)
Fine reticular granularity ("ground glass appearance")
– Air bronchograms
– Lab
Hypoxemia
Hypercarbia (increased pCO2)
– Metabolic acidosis
• Differential Dx
– Group B strep Pneumonia
– Cyanotic Heart Disease
– Persistent Pulmonary Hypertension
– Pneumothorax
– Aspiration Pneumonia
• Treatment
– *Treat the basic defect = Prematurity
Gentle handling and minimal disturbance
Isolette to maintain neutral core temp and reduce O2 consumption
IV fluids, glucose, electrolytes and nutrition
– RDS
Warm humidified O2 should be administered to keep pO2 between 55-
70mmHg (>90% Saturation)
Continuous positive airway pressure by nasal prongs
Mechanical ventilation
Antibiotics
Exogenous surfactant administration
• Has improved survival, increased compliance and reduced vent
pressures
• Has not reduced incidence of chronic lung disease and has
complications
– Complication includes pneumothorax
– Inadequate exchange of O2 and CO2
– Treat secondary manifestations such as circulatory insufficiency and metabolic
acidosis
– Careful monitoring of heart rate, respiratory rate, BP, fluids and electrolytes
• Prognosis
– Mortality from RDS has decreased to about 10%
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Humerus Arm Anatomical Neck ArmDocument41 pagesHumerus Arm Anatomical Neck ArmmcwnotesNo ratings yet
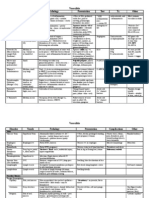
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDocument3 pagesVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesNo ratings yet
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDocument3 pagesVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesNo ratings yet
- Cytokines: Cytokine Source Target/Effect OtherDocument1 pageCytokines: Cytokine Source Target/Effect OthermcwnotesNo ratings yet
- Cytokines: Cytokine Source Target/Effect OtherDocument1 pageCytokines: Cytokine Source Target/Effect OthermcwnotesNo ratings yet
- Antibodies: Type Response Action Other Hypersensitivity TypeDocument2 pagesAntibodies: Type Response Action Other Hypersensitivity TypemcwnotesNo ratings yet
- Antibodies: Type Response Action Other Hypersensitivity TypeDocument2 pagesAntibodies: Type Response Action Other Hypersensitivity TypemcwnotesNo ratings yet
- Lab 2: Contractility of Visceral and Vascular (Aorta) SmoothDocument3 pagesLab 2: Contractility of Visceral and Vascular (Aorta) SmoothmcwnotesNo ratings yet
- Hypersensitivity: Type Molecule Antigen Type Effector Mechanism Reaction DiseasesDocument1 pageHypersensitivity: Type Molecule Antigen Type Effector Mechanism Reaction DiseasesmcwnotesNo ratings yet
- Surface Molecules: Molecule Location Ligand Action OtherDocument1 pageSurface Molecules: Molecule Location Ligand Action OthermcwnotesNo ratings yet
- Lab 10 Digestive System: Salivary Glands, Tongue, Esophagus, StomachDocument3 pagesLab 10 Digestive System: Salivary Glands, Tongue, Esophagus, StomachmcwnotesNo ratings yet
- Lab 1: Electrical and Mechanical Properties of Skeletal MuscleDocument3 pagesLab 1: Electrical and Mechanical Properties of Skeletal MusclemcwnotesNo ratings yet
- Lab 1: Electrical and Mechanical Properties of Skeletal MuscleDocument3 pagesLab 1: Electrical and Mechanical Properties of Skeletal MusclemcwnotesNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- IKMAN NURHAKIM XII IPS 3 - Explanation Text BDRDocument2 pagesIKMAN NURHAKIM XII IPS 3 - Explanation Text BDRikman nibosNo ratings yet
- (YAKEEN 2.0) : Respiration in Plants (Revision Test)Document5 pages(YAKEEN 2.0) : Respiration in Plants (Revision Test)JAGGA GAMING OFFICIALNo ratings yet
- Lecture Notes On Transport of Respiratory GasesO2 by Prof Y JaggiDocument8 pagesLecture Notes On Transport of Respiratory GasesO2 by Prof Y JaggiGautam NatrajNo ratings yet
- Guyton Respiration OverviewDocument6 pagesGuyton Respiration Overviewbahahahah100% (1)
- Students - Cellular-RespirationDocument49 pagesStudents - Cellular-RespirationechaNo ratings yet
- Breathing and RespirationDocument1 pageBreathing and RespirationnaduniNo ratings yet
- 34 AsfiksiaDocument40 pages34 AsfiksiaDaeng Anggit AdirahmanNo ratings yet
- Mechanical Ventilation Airway Pressure Release Ventilation Checklist Respiratory Therapy - 070420Document3 pagesMechanical Ventilation Airway Pressure Release Ventilation Checklist Respiratory Therapy - 070420shubham2812No ratings yet
- Chest Physiotherapy in Intensive Care Unit (ICU) PDFDocument399 pagesChest Physiotherapy in Intensive Care Unit (ICU) PDFGuillermo Sasso Pacheco83% (6)
- Humidification in The Intensive Care UnitDocument272 pagesHumidification in The Intensive Care UnitAbu HibbaanNo ratings yet
- Management of Pneumothorax With Oxygen Therapy A CDocument4 pagesManagement of Pneumothorax With Oxygen Therapy A CAndreas Paian SiahaanNo ratings yet
- Nursing Care Plan Assessment Explanation of The Problem Goals and Objectives Intervention Rationale EvaluationDocument7 pagesNursing Care Plan Assessment Explanation of The Problem Goals and Objectives Intervention Rationale EvaluationGuile RilleraNo ratings yet
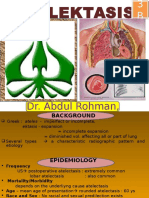
- AtelectasisDocument26 pagesAtelectasisArini NurlelaNo ratings yet
- Acute Respiratory FailureDocument17 pagesAcute Respiratory FailurejulianajosNo ratings yet
- PhysioEx Exercise 7 Activity 2Document7 pagesPhysioEx Exercise 7 Activity 2Jorge CuevaNo ratings yet
- Vela Plus SpecsDocument2 pagesVela Plus SpecsZulkifli IsmailNo ratings yet
- Toronto Notes Respirology PDFDocument40 pagesToronto Notes Respirology PDFJaya Semara Putra67% (3)
- 1 Neopuff Infant Resuscitator SetDocument2 pages1 Neopuff Infant Resuscitator SetbetehaNo ratings yet
- I. Objectives:: A Semi-Detailed Lesson Plan in General Biology-IiDocument19 pagesI. Objectives:: A Semi-Detailed Lesson Plan in General Biology-IiMhimi ViduyaNo ratings yet
- WHLP Gen Bio 4 2nd QuarterDocument6 pagesWHLP Gen Bio 4 2nd QuarterSir JoshNo ratings yet
- Hidung Dan Sinus ParanasalisDocument16 pagesHidung Dan Sinus ParanasalisChearin Dhea SNo ratings yet
- Lung Sounds: An Assessment of The Patient in Respiratory DistressDocument40 pagesLung Sounds: An Assessment of The Patient in Respiratory DistressJoseph Rodney de LeonNo ratings yet
- Incentive SpirometryDocument5 pagesIncentive Spirometryrachelmores12No ratings yet
- Chatburn - Fundamentals of MVDocument313 pagesChatburn - Fundamentals of MVJesus Alonso Hernandez ANo ratings yet
- Early Initiation MV 2017 - DR - TrisnaDocument34 pagesEarly Initiation MV 2017 - DR - TrisnaHappy ShalalaNo ratings yet
- 2017 Acute Respiratory Distress Syndrome PDFDocument354 pages2017 Acute Respiratory Distress Syndrome PDFA. Rauf100% (1)
- Year 8 Breathing and RespirationDocument4 pagesYear 8 Breathing and RespirationRodaina MahmoudNo ratings yet
- Puritan Bennett VentilatorDocument8 pagesPuritan Bennett VentilatorRohmatsolihinNo ratings yet
- Respiratory EmergencyDocument14 pagesRespiratory EmergencyThomas SentanuNo ratings yet
- Waveform Questions /critical Care Board ReviewDocument14 pagesWaveform Questions /critical Care Board ReviewAzmachamberAzmacareNo ratings yet