Professional Documents
Culture Documents
00004630-200511000-00003 Comparison of Measured Resting Energy Expenditure
Uploaded by
José Luis Navarro RomeroOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
00004630-200511000-00003 Comparison of Measured Resting Energy Expenditure
Uploaded by
José Luis Navarro RomeroCopyright:
Available Formats
Comparison of Measured Resting Energy Expenditure Versus Predictive Equations in Pediatric Burn Patients
Rungsinee A. Liusuwan, MSRD,* Tina L. Palmieri, MD,* Lysa Kinoshita, RRT,* David G. Greenhalgh, MD*
Many equations have been developed to estimate resting energy expenditure (REE) in thermally injured patients. A consensus has not been reached on the accuracy of these equations in children. The purpose of our study was to compare three predictive equations: Harris Benedict 2 multiplier (HB 2), Mayes (MG), and the WorId Health Organization 2 multiplier (WHO 2) with measured resting energy expenditure I.3 multiplier (MREE 1.3) in pediatric burn patients. MREE was measured by open-circuit indirect calorimetry in 10 burned children (6 boys, 4 girls) aged 2 to 10 years with TBSA burn ranges from 35% to 97%. MREE 1.3 was compared with values obtained by HB 2, MG, and WHO 2 predictive equations. When comparing MREE 1.3 with all three equations, significant differences were found when compared with HB 2 and MG, but there were no significant difference between MREE 1.3 vs WHO 2. The HB 2 and MG equations overpredicted MREE 1.3 by 29% and 19%, respectively. Many predictive equations have been developed to predict energy expenditure in burns, but their accuracy in predicting MREE 1.3 is variable. A larger study comparing/contrasting predictive equations and resting energy expenditure measured by indirect calorimetry is needed to improve the prediction of energy needs in burned children. (J Burn Care Rehabil 2005;26:464470)
Thermal injury is among the most severe types of trauma that the body can sustain. An extensive burn increases energy requirements as the result of its induction of the hypermetabo1ic and catabolic state.1,2 It is well-documented that nutritional support may improve morbidity and mortality after severe thermal injury.3 It also is known, however, that complications of both underfeeding and overfeeding may be detrimental. Overfeeding can cause hepatic dysfunction, hyperglycemia, and elevated carbon dioxide production, which may impair weaning from mechanical ventilation.4 However, underfeeding can delay wound healing, decrease resistance to infection, and prolong mechanical ventilation by failing to restore respiratory muscle strength and endurance.4 Therefore, adequate nutritional support is essential in
From the *Shriners Hospital for Children Northern California, Sacramento, and Department of Surgery, University of California, Davis. Address correspondence to David G. Greenhalgh, Department of Burn Surgery, Shriners Hospitals for Children, Northern California, 2425 Stockton Boulevard, Suite 718, Sacramento, California 95817. Copyright 2005 by the American Burn Association. 0273-8481/2005 DOI: 10.1097/01.bcr.0000185786.38365.3d
burned patients to prevent the detrimental consequences of overfeeding and underfeeding. After burn injury, patients not only present with dramatic increases in the basal metabolic rate, but they also develop a stress-induced catabolism which usually is commensurate with the size of their burns.5 The metabolic response in burn injury may vary depending upon the percentage of open wounds and the infections, all of which may increase the resting energy expenditure. For patients with large cutaneous burns, the resting metabolic rate may be increased to 100% greater than normal.6 Indirect calorimetry is useful in detecting variations in energy expenditure among individuals and for detecting changes in metabolism that occur during the course of a burn that cannot be estimated by static formulas. Unlike indirect calorimetry measurements, static formulas may not take into consideration hypermetabo1ic and catabolic states, which can persist for several weeks and even months after burn injury. Thus, these formulas may contribute to overfeeding and underfeeding the patients. Several equations have been developed to predict the high energy needs of the burn patient either by using burn-related or healthy pediatric equations multiplied by an activity or injury factor.6 9 Measure-
464
Journal of Burn Care & Rehabilitation Volume 26, Number 6
Liusuwan et al
465
Table 1. American Association for Respiratory Care (AARC) Clinical Practice Guidelines
AARC Clinical Practice Guideline for Exclusion of REE 1. REE less than 12 hr postoperatively 2. Oxygen requirement of 60% FIO2 3. Patients using percussive ventilators, such as Volumetric Diffusive Respirators, (Percussionaire Corporation. Sand Point, Idaho) 4. An airway with significant air leaks 5. Chest tubes with evident leaks 6. An uncooperative or agitated patient
Committee. This retrospective study included burn patients ages 2 to 10 years old who were admitted within 10 days of burn injury with at least 20% TBSA to the Shriners Hospitals for Children Northern California between January 2001 and January 2004. In addition, inclusion required enteral feeding for the entire duration of this study and a total of three MREEs (one being instituted soon after admission and weekly thereafter). Patients needed to have a Foley catheter in place for the collection of weekly nitrogen balance and a prealbumin analysis performed weekly. Subjects also had documented admission and discharge weights.
ment of resting energy expenditure (MREE) by using indirect calorimetry frequently indicates that predictive equations overestimate the actual energy needs.1,10 12 Although indirect calorimetry is considered the gold standard for determining calorie goals for burn patients, this instrument may not be available to all clinicians, and the use of the appropriate predictive equations may be used as an alternative. Current literature suggests that a consensus has not been reached on the use of these equations in children. This lack of consensus justifies a closer examination of these predictive equations to provide optimal nutritional support for burn patients. The purpose of our study was to evaluate several well-established predictive equations for the calculation of expected calorie requirements in burned children and to compare these values with those obtained from indirect calorimetry.
Indirect Calorimetry
Indirect calorimetry was obtained within 24 hours of admission in nonintubated burn patients with 20% TBSA as well as patients who required mechanical ventilation. Patients were excluded from the study in accordance with the American Association for Respiratory Care Clinical Practice Guidelines (Table 1).13 The Medical Graphic CCM-D Model 790601-001 (Medical Graphics Corporation, St Paul, MN) was used for all REE studies. The mode of testing was by ventilator, mouthpiece, mask, or canopy. Patients were tested in bed to eliminate the need to support the head and extremities. The environment was quiet and interruption free. All patients tested were on continuous tube feeding, and the rate was kept constant for 12 hours before testing. A minimum of 2 hours elapsed after dressing changes or other painful invasive procedures before testing per guidelines suggested for nutrition assessment in critical care and respiratory care clinics of North America.13,14 A minimum of 20 minutes of breath by breath expired gas analysis was collected. The quality of the test was evaluated by determining whether the respiratory quotient (RQ) was consistent with the patients nutritional intake, if RQ rested within normal physio-
SUBJECTS AND METHODS
Subjects
Approval to perform the study was obtained from the University of California, Davis Human Subjects
Table 2. Commonly used equations to estimate caloric needs
Equations Harris Benedict W weight in kg WHO Age and Gender Male Female H Height in cm Male 3 yr Male310 yr Female 3 yr Female 310 yr Male and Female Male and Female
Formulas 66 (13.7 W) (5 H) (6.8 A) 665 (9.6 W) (1.8 H) (4.7 A) A age (60.9 W) 54 (22.7 W) 495 (61 W) 51 (22.5 W) 499 108 68W 3.9 % TBSA 818 37.4W 9.3 % TBSA
Mayes (3 yr) Mayes (310 yr)
These three sets of equations were used in predicting energy needs. Harris Benedict is based on weight, height, and age. World Health Organization (WHO) is based weight and age. Mayes equation is based on weight %TBSA.
466 Liusuwan et al
Journal of Burn Care & Rehabilitation November/December 2005
logical range (0.67-1.3), if measured volume of oxygen consumption (VO2) was within 10% of the mean value measured, if measured volume of carbon dioxide (VCO2) was within 6% of mean value, and if the measurement was of sufficient length to account for variability in VO2 and VCO2. A minimum of 5 to 8 minutes of breath by breath data was used to obtain the RQ and REE for each patient.
Table 3. Demographics of study patients
Variable Age, years % burn, TBSA Admission weight, kg Discharge weight, kg Height, cm Minimum 2 35 13 14 85 Maximum 10 97 60 45 176 Mean SD 52 64 24 25 13 23 8 117 25
Biochemical Parameters
Blood samples were collected to determine weekly prealbumin using the Dimension Clinical Chemistry System. The 24-hour urinary urea nitrogen (Mikro-Kjehadahl) was calculated using the following formula: N balance Nintake Noutput (24hour protein intake/6.25 ) (24-hour UUN estimated of nonurea nitrogen losses).15 nificant. The prealbumin was 9 2 mg/dl for the first 2 weeks after burn injury whereas the value improved to 18:1:3 (18 3) mg/dl at 3 weeks after burn (Table 4). There was a significant improvement of mean prealbumin, from 9 mg/dl to 18 mg/dl. The mean nitrogen balance increased from 2 to 6 at 3 weeks after burn as compared with the first 2 weeks after injury. The mean RQ SD range was 0.88 0.09 (0.771.1), which suggests no overfeeding or underfeeding throughout the course of the burn treatment. On the basis of our data, two of our patients, with RQs of 0.77 and 0.78, were considered underfed, and one patient, with an RQ greater than 1, was considered overfed. The rest of our subjects fell within the range of 0.80 to 0.95. Estimated energy requirement includes a multiplication factor such as an activity factor or a stress factor. Analysis of variance performed from Mayes et al18 and Saffle et al11 have verified that 1.3 is the most reliable multiplier of MREE. Stress factors of 1.5 to 2.0 have been suggested as multipliers for burn in predictive equations.3 Thus, our study used these stress factors as a multiplier (Table 5). The mean value of the Harris Benedict equation with 2.0 multiplier (HB 2) was 2085 475 calories. The MG equation had mean value of 1924 475 calories, whereas the WHO equation with the 2 multiplier (WHO 2) had mean value of 1665 275 calories. The HB 2
Table 4 Nutrition param
Nutrition Parameters Mean Value SD (Range) 0.88 0.09 92 18 3 2 0.8 (3 to 3) 6 1 (3 to 10)
Predictive Equations
Three well-known formulas, Harris-Benedict (HB),16 World Health Organization (WHO),17 and Mayes (MG)18 equations were calculated and compared with MREE with 1.3 multiplier as suggested by Mayes et al.18 The multiplier of 1.3 added to MREE was used to maintain 95% of preburn weight at discharge and ensure adequate nutrition.18 The injury factor of 2 was added to HB and WHO in accordance with the guidelines for burn injury in the Multidisciplinary Handbook on Pediatric Nutritional Support.19 Table 2 describes the commonly used equations.
Statistical Analysis
An independent t-test was used to evaluate significance of the difference between admitted weight and the discharged weight. Two-way analysis of variance was used to evaluate the effects of sex, age, and the primary differences between each equation as compared with the REE standard. The Tukey test was used to make all pair-wise comparisons between groups. P .05 was used for the determination of statistical significance. Systat (version 9.0, Systat, Inc, Point Richmond, CA) was the statistical software package used for the analyses.
RESULTS
The age of our patients ranged from 2 to 10 years, with the mean age of 5 2 years (Table 3). The burn size ranged from 35% to 97%, with a mean of 64 24% TBSA. Height ranged from 85 to 176 cm, with a mean value of 117 25 cm. Although there was a 2-kg difference between mean admission and discharge weights, the difference was not statistically sig-
RQ Pre-albumin first 2 weeks after burn (mg/d1) Pre-albumin post 3 weeks after burn (mg/dl) N-balance first 2 weeks after burn N-balance post 3 weeks after burn
Laboratory values such as pre-albumin and N-balance from 2 weeks after bum were compared with 3 weeks after burn RQ, respiratory quotient
Journal of Burn Care & Rehabilitation Volume 26, Number 6
Liusuwan et al
467
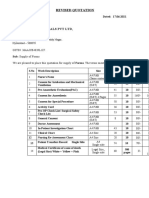
TABLE 5. Measured resting energy expenditure (REE) vs predicted REE
% TBSA Age Sex MG 72 5 35 2 95 3 97 3 55 2 38 6 80 4 85 7 44.5 10 42 7 64 5 23 2.5 F F M M F M M M M F 2106 1333 1663 1663 1235 2398 1918 2255 2876 1794 1924* 475 WHO 2 1541 1434 1804 1804 1216 1921 1364 1682 2203 1680 1665 275 HB 2 2050 1943 1779 1680 1878 2219 1663 2069 3400 2172 2085* 475 MREE 1.3 2284 1279 1199 1642 1556 1481 1457 1503 1728 1968 1610 305
Figure 1. Comparison of resting energy expenditure values from indirect calorimetry (MREE 1.3, shaded) with predictive equation (MG, unshaded).
Mean SD
MREE 1.3 Measured resting energy expenditure from indirect calorimetry 1.3-average of 3 data points; MG, Mayes equation; WHO 2, World Health Organization with multiplier of 2; HB 2, Harris benedict equations with multiplier of 2. * Denotes significant differences from MREE 1.3
was 475 calories greater than MREE 1.3, whereas MG equation was 314 calories more than MREE 1.3 and the WHO 2 was 55 calories higher than the MREE 1.3 (Figures 1-3). Statistical analysis (using analysis of variance) revealed significant differences between MREE 1.3 and HB 2, as well as MREE 1.3 and MG, but no differences between MREE 1.3 and WHO 2.
Figure 2. Comparison of resting energy expenditure values from indirect calorimetry (MREE 1.3, shaded) with predictive equation (WHO 2, unshaded).
DISCUSSION
Several equations have been developed to predict energy needs of burned children. Some equations include TBSA burn, and others use an injury factor as well as an activity factor to predict the energy needs. The HB equation has a separate standard for men and women that incorporates weight in kilograms, height in centimeters, and age in years. The World Health Organization divides the equation into different age groups and sex: younger than 3 years of age boys and girls; age 310 years boys and girls with weight in kilograms incorporated in the equation. The Mayes equation is the only equation tested that includes % TBSA burn along with weight in kilograms and age in years. Our measurement of resting energy expenditure by indirect calorimetry revealed that the extent of hypermetabolism was less than predicted by the HB 2, MG, and WHO 2 formulas. The excess calories from these formulas range from 3%, 19%, and 29% greater than MREE 1.3 for
Figure 3. Comparison of resting energy expenditure values from indirect calorimetry (MREE 1.3, shaded) with predictive equation (HB 2, unshaded).
WHO 2, MG, and HB 2, respectively. Feeding patients much more than the actual caloric needs may lead to lipogenesis and increased CO2 production, which affects respiratory status, indicating increased minute ventilation, and may require increased ventilatory support. This finding that predictive equations overestimated measured resting energy expenditure is consistent with Carlson et al,2 Saffle et al,20 and Turner et
468 Liusuwan et al
Journal of Burn Care & Rehabilitation November/December 2005
al.10 When comparing all of the tested equations against MREE with the recommended multiplier of 1.3, we found significant differences between MREE 1.3 and the HB 2 and MG but not WHO 2. The multiplier of 1.3 for MREE was chosen because most investigators agree that it is needed to maintain at least 95% of preburn weight and to keep the RQ within 0.80 to 0.95.11,18,21 This RQ range also suggests adequate feeding with mixed substrate oxidation of fat, protein, and carbohydrate. An RQ of 1.0 or more suggests overfeeding with the conversion of carbohydrate to fat, which creates a higher amount of CO2 but consumes relatively less O2. However, an RQ of 0.7 or less suggests fat oxidation, which means underfeeding.22 The largest discrepancy of energy needs was found with the HB equation, which predicts the energy needs in excess of 29% greater than the MREE 1.3. There are several possible explanations why the HB 2 may not accurately predict MREE 1.3 for our population. First, the level of technological sophistication was lower in the 1900s, when the HB predictive equations were developed, than it is today. Second, the HB equations were developed in a normal healthy population of 97 infants and 239 adults but excluded school-aged children.16 The WHO 2 equation overpredicted the MREE 1.3 for only 3% in our study. This equation was developed from a larger pool of subjects (7500) and was designed to work not only in infants and adults but also in children. Moreover, just like HB equation, the WHO equation does not include the %TBSA burn as part of the equations, which many investigators believe to be a primary influencing factor of resting energy expenditure22 The MG equation is the only equation that includes %TBSA burn as part of the equation and was 19% greater than the value of MREE 1.3. This difference may be result from the use of preburn weight in the MG study vs admission weight in our study because most of our patients did not know their preadmission weight. It is also noted that the MG equation was designed for patients with 10% to 50% TBSA and our study population had a mean burn size of 64%. Because many studies have shown that there is no further increase in metabolism with burn sizes greater than 50%,2,23,24 using the %TBSA burn as part of the equation for burn size greater than 50% may not be appropriate. In our study, we used the maximum burn of 50% for the MG calculation despite patients having greater than 50% burns. Although Mayes et al18 found that the WHO equation considerably underpredicted the MREE in burned children younger than 3 years of age, our data showed the
opposite. These findings may be attributable to our small sample size in the group that was younger than 3 years age. Rodriguez et al25 examined 116 children and adolescents (57 obese and 59 nonobese) whose ages were between 7.8 and 16.6. The study recommended that the WHO may be useful in girls and that the Schofield weight-only equation may be useful in nonobese children. It is noted that the HB equation significantly underestimated REE in the Rodriguez study which, again, was the opposite result found in our study. This may be attributable to the age of the population studied; the patients in Rodriguez et als study had a mean age of 11.9 years, and those in our study had mean age of 5 years. Also mean weight for Rodriguez et als subjects was 63.9 for obese and 43.2 kg for nonobese, whereas our population has mean weight of 23 to 25 kg. The difference observed may be attributable to the fact that our population may not exactly match the clinical characteristics with Rodriguez et als study. Dickerson et al3 suggested that 33% of the 46 publications published from 1953 to 2000 for estimating resting energy expenditure of thermally injured patients were biased toward overpredicting the measured resting energy expenditure, whereas 19% of publications consistently underpredicted the measured resting energy expenditure. They felt that 48% contained methods that were unbiased. Our results suggest that a consensus has not been reached on the effectiveness of these equations in estimating energy needs of burned children. Several theories may be used to explain the discrepancies. First, the current standard practice is to perform early excision and grafting to aggressively close the wound. This practice has the potential to lower the energy needs in burn patients. Second, the benefits of early enteral feeding in lowering hypermetabolism and reducing catabolism have been shown by many, but not all, investigators.5,26 28 Third, the development and technological advances of portable indirect calorimetry may provide a more accurate measurement for calories and oxygen consumption than does the older equipment. The newer instrument may decrease errors caused by leaks and has an improved calibration to increase the accuracy of measurements. These factors collectively may contribute to the discrepancy found between MREE 1.3 and the predicted equations. Therefore, our results suggest that predictive equations may need to be re-evaluated more frequently to keep pace with the changes in clinical practice as well as advances in technology. One of the main goals for our feeding regimen is to
Journal of Burn Care & Rehabilitation Volume 26, Number 6
Liusuwan et al
469
ensure that patient receives 10% of his or her estimated calories on the daily basis. Weight change often is used as an indicator for adequacy of nutritional support. In this study, there were no significance differences (P 0.05) between admission and discharge weights, which suggests that our current feeding regimen based on the range of WHO x 2.0 and MREE x 1.3 as well as receiving 10% of the predicted energy needs may be appropriate to maintain 10% of admitted weight, which is our institution goal. The clinical observation of our institution was that many patients were able to maintain 10% of their admitted weight at discharge as the result of our standard practice. Another goal of nutritional support is to provide adequate protein to maintain a positive nitrogen balance. One of the simplest methods to estimate protein requirements is to perform a nitrogen balance study. The mean of the nitrogen balances were 2 for the first 2 weeks after burn and gradually increased thereafter to mean value of 6 by week 3 after burn. This finding suggests adequate protein intake in these children. The serum concentration of prealbumin was used as a nutritional marker in this study. Much of the literature advocates using prealbumin levels as an indicator of the response to nutritional support because of its short half-life and small body pool size.29 32 Our patients had significant improvement of prealbumin levels by week 3 after burn, suggesting adequate visceral protein stores and an improved nutritional status. Because there is no gold standard set for the amount of weight change in critical care patients to reflect adequacy of nutritional support, it is important to monitor other laboratory tests designed to evaluate nutrition, such as prealbumin together with a clinical picture of a patient to derive appropriate nutritional care plan. Indirect calorimetry is considered the gold standard, yet it also presents its own limitations. Access to indirect calorimetry, as well as specific clinical situations, may not allow the patient to be a candidate for this technique. Therefore, although predictive equations may not be able to fully determine the exact energy needs of the patient, they are a useful tool in a clinical setting. Whether a predictive equation or direct measurements are used, clinical judgment is the key to providing the patient with specific nutritional interventions. The number of patients reported is limited because of the young age group and vigorous entry criteria. Although this study may be limited by our small sample size, it suggests that nutritional management of young children with burn injury continues to present
a challenge. The abundance of predictive equations confirms the inaccuracy of current nutritional need calculations. It has been many years since the first published predictive equation was proposed, and consensus has still not been reached on which equation is the best predictor of estimating caloric needs of burn patients. Our findings suggest that a larger study comparing/contrasting predictive equations and resting energy expenditure measured by indirect calorimetry is needed to establish an equation that can best predict the energy needs of children with burns.
REFERENCES
1. Cunningham JJ, Hegarty MT, Meara PA, Burke JF. Measured and predicted calorie requirements of adults during recovery from severe burn trauma. Am J Clin Nutr 1989;49: 4048. 2. Carlson DE, Cioffi WG Jr, Mason AD Jr, McManus WF, Pruitt BA Jr. Resting energy expenditure in patients with thermal injuries. Surg Gynecol Obstet 1992;174:2706. 3. Dickerson RN, Gervasio JM, Riley, ML, et al. Accuracy of predictive methods to estimate resting energy expenditure of thermally injured patients. JPEN J Parenter Enteral Nutr 2002;26:1729. 4. Hart D, W.S., Chinkes, DL, Beauford RB, et al. Effects of early excision and aggressive enteral feeding on hypermetabolism, catabolism, and sepsis after severe burn. J Trauma 2003;54:75564. 5. Mochizuki H, Trocki O, Dominioni, L, Brackett KA, Joffe SN, Alexander JW. Mechanism of prevention of postburn hypermetabolism and catabolism by early enteral feeding. Ann Surg 1984;200:297310. 6. Long C. Energy expenditure of major burns. J Trauma 1979;19 (11 Suppl):904-6. 7. Curreri PW, Richmond D, Marvin J, Baxter CR. Dietary requirements of patients with major burns. J Am Diet Assoc 1974;65:4157. 8. Allard JP, Pichard C, Hoshino E. Validation of a new formula for calculating the energy requirements of burn patients. J Parenter Enteral Nutr 1990;14:1158. 9. Xie WG. Li A, Wang SL. Estimation of calorie requirements of burned chinese adults. Burns 1993;19:146. 10. Turner WW, Jr, Ireton CS, Hunt, JL. Baxter CR. Predicting energy expenditures in burned patients. J Trauma 1985;25: 116. 11. Saffle JR, Medina E, Raymond, J, Westenskow D, Kravitz M, Warden GD. Use of indirect calorimetry in the nutritional management of burned patients. J Trauma 1985;25:329. 12. Gore DC, Rutan RL, Hildreth M, Desai MH, Herdon DN. Comparison of resting energy expenditures and caloric intake in children with severe burns. J Burn Care Rehabil 1990;11: 4004. 13. American Association for Respiratory Care. AARC clinical practice guideline. Metabolic measurement using indirect calorimetry during mechanical ventilation. Respir Care 1994; 39:1170-5. 14. Berry JK, Braunschweig, CA. Nutritional assessment of the critically ill patient. Crit Care Nurs Q 1998;21:3346. 15. Larsson J, Lennmarken C, Martensson J, Sandstedt S, Vinnars E. Nitrogen requirements in severely injured patients. Br J Surg 1990;77:413-6. 16. Harris JA, Benedict F. A biometric study of basal metabolism in man. Washington, DC: Carnegie Institute of Washington; 1919. p. 279. 17. World Health Organization Energy and Protein Require-
470 Liusuwan et al
Journal of Burn Care & Rehabilitation November/December 2005
18. 19. 20. 21. 22. 23. 24.
25.
ments. Reports of a joint FAO/WHO/UNU expert consultation. WHO Technical Report Series 1985;724. Mayes T, Gottschlich MM, Khoury J, Warden GD. Evaluation of predicted and measured energy requirements in burned children. J Am Diet Assoc 1996;96:249. Chan DS, Wong, M. Multidisciplinary handbook on pediatric nutritional support. Am J Health Syst Pharm 1997;54:1355. Saffle JR, Larson CM, Sullivan J. A randomized trial of indirect calorimetry based feedings in thermal injury. J Trauma 1991;30:776-83. Trocki MJ, Robbins ST, Eichelberger MR. Evaluation of early enteral feeding in children less than 3 years old with smaller burns (8-25 percent TBSA). Burns 1995;21:1723. Allard JP, Whiwell, J, Paschutinski L, Peters WI. Factors influencing energy expenditure in patients with burns. J Trauma 1988;28:199202. Milner, EA. A longitudinal study of resting energy expenditure in thermally injured patients. J Trauma 1994;37: 16770. Cunningham JJ. Factors contributing to increased energy expenditure in thermal injury: a review of studies employing indirect calorimetry. JPEN J Parenter Enter Nutr 1990;14: 64956. Rodriguez, G. Moreno LA, Sarria A, Fleta J, Bueno M. Rest-
26.
27. 28. 29. 30. 31. 32.
ing energy expenditure in children and adolescents: agreement between calorimetry and prediction equations. C1in Nutr 2002;21:25560. Dominioni L, Trocki O, Fang, CH, et al. Enteral feeding in burn hypermetabolism: nutritional and metabolic effects of different levels of calorie and protein intake. J Parenter Enteral Nutr 1985;9:26979. Wood RH, Caldwell FT Jr, Wallace RH. Effect of early feeding on the postburn hypermetabolic response in rats. J Trauma 1990;30 (12 Suppl):S2430. Wood, RH, Caldwell FT Jr, Bowser-Wallace, RH. The effect of early feeding on postburn hypermetabolism. J Trauma 1988;28:17783. Winkler MF, Gerrior SA, Pomp A. Use of retinol-binding protein and prealbumin as indicators of the response to nutrition therapy. J Am Diet Assoc 1989;89:6847. Brose L Prealbumin as a marker of nutritional status. J Burn Care Rehabil 1990;11:3725. Pleban WE. Prealbumin: a biochemical marker of nutritional support. Conn Med 1989;53:4057. Moskowitz SR, Pereira G, Spitzer A, Heaf L, Amsel J, Watkins JB. Prealbumin as a biochemical marker of nutritional adequacy in premature infants. J Pediatr 1983;102: 74953. Cadmus
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Case TetanusDocument37 pagesCase TetanusKimhazel A. Galleon100% (1)
- TPH TherapheuticsDocument10 pagesTPH TherapheuticsAl Sah Him100% (2)
- E BooksDocument29 pagesE BooksTawfeeq BA Abbad100% (2)
- Mims Doctor 2020Document68 pagesMims Doctor 2020Zulqarnain RamliNo ratings yet
- Useful Tips To Write RN ResumesDocument22 pagesUseful Tips To Write RN ResumesRN resume100% (1)
- Tap Into Your Happy Chemicals - Dopamine, Serotonin, Endorphins, & OxytocinDocument8 pagesTap Into Your Happy Chemicals - Dopamine, Serotonin, Endorphins, & OxytocinCorola_de_minuniNo ratings yet
- Lakshmi Micro TeachingDocument20 pagesLakshmi Micro Teachingduddela lakshmi100% (1)
- Acute Colonic Pseudo-ObstructionDocument4 pagesAcute Colonic Pseudo-ObstructionJosé Luis Navarro Romero100% (1)
- 00006123-200802001-00006 EpilepsyDocument1 page00006123-200802001-00006 EpilepsyJosé Luis Navarro RomeroNo ratings yet
- 00006123-200802001-00011 Multiloculated Pyogenic Brain AbscessDocument6 pages00006123-200802001-00011 Multiloculated Pyogenic Brain AbscessJosé Luis Navarro RomeroNo ratings yet
- 00006123-200802001-00012 Hyperbaric Oxygen Treatment of PostoperativDocument10 pages00006123-200802001-00012 Hyperbaric Oxygen Treatment of PostoperativJosé Luis Navarro RomeroNo ratings yet
- TiflitisDocument5 pagesTiflitisJosé Luis Navarro RomeroNo ratings yet
- 00006123-200802001-00036 Stereotactic RadiosurgeryDocument4 pages00006123-200802001-00036 Stereotactic RadiosurgeryJosé Luis Navarro RomeroNo ratings yet
- 00004630-200511000-00002 Energy Expenditure in Burns Let's MeasureDocument2 pages00004630-200511000-00002 Energy Expenditure in Burns Let's MeasureJosé Luis Navarro RomeroNo ratings yet
- 00006123-200802001-00019 EndosDocument1 page00006123-200802001-00019 EndosJosé Luis Navarro RomeroNo ratings yet
- 00006123-200802001-00013 Infections and InfestationsDocument1 page00006123-200802001-00013 Infections and InfestationsJosé Luis Navarro RomeroNo ratings yet
- Prudent Use of Antimicrobial Agents: Not Just For HumansDocument3 pagesPrudent Use of Antimicrobial Agents: Not Just For HumansJosé Luis Navarro RomeroNo ratings yet
- 00006123-200802001-00006 EpilepsyDocument1 page00006123-200802001-00006 EpilepsyJosé Luis Navarro RomeroNo ratings yet
- Uso Prudentedelosantibio Ticos - Revisio N Delosconceptosyana Lisis DelasperspectivasDocument2 pagesUso Prudentedelosantibio Ticos - Revisio N Delosconceptosyana Lisis DelasperspectivasJosé Luis Navarro RomeroNo ratings yet
- Uso Prudentedelosantibio Ticos - HemosactuadodelamejormaneraposibleDocument2 pagesUso Prudentedelosantibio Ticos - HemosactuadodelamejormaneraposibleJosé Luis Navarro RomeroNo ratings yet
- Punjab Amarnath Yatra Doctor ListDocument6 pagesPunjab Amarnath Yatra Doctor ListChhote yadavNo ratings yet
- (Mangifera Indica L) Arumanis Terhadap Kadar SGPTDocument11 pages(Mangifera Indica L) Arumanis Terhadap Kadar SGPTMahati UlfahNo ratings yet
- Reducing Dental Anxiety in ChildrenDocument4 pagesReducing Dental Anxiety in Childrenapi-613602134No ratings yet
- Hayes & Strauss (1998) Dynamic Systems Theory..Document9 pagesHayes & Strauss (1998) Dynamic Systems Theory..Teodora-Aurora BrebenaruNo ratings yet
- The Pharmacy Act 1948Document27 pagesThe Pharmacy Act 1948alkca_lawyerNo ratings yet
- 2 5348228160427133754Document18 pages2 5348228160427133754Muhammad HasanNo ratings yet
- Community Development ProjectDocument12 pagesCommunity Development ProjectSwethaNo ratings yet
- Parasitology and EntomologyDocument89 pagesParasitology and EntomologyMeinrad Komba100% (3)
- AU NZ Cortitrol PIPDocument2 pagesAU NZ Cortitrol PIPthanh.tkNo ratings yet
- Arnica Montana-Based Product For Treating Joint Pain - Flexogor - Is Prepared For Sale in AsiaDocument2 pagesArnica Montana-Based Product For Treating Joint Pain - Flexogor - Is Prepared For Sale in AsiaPR.comNo ratings yet
- Neurology Physiology 25 Spinal Cord Ascending Tracts SpinothalamicDocument1 pageNeurology Physiology 25 Spinal Cord Ascending Tracts SpinothalamicxcqzprnfkrNo ratings yet
- 108 Names of DhanvantariDocument7 pages108 Names of DhanvantaricantuscantusNo ratings yet
- Inserto Control Idg PDFDocument3 pagesInserto Control Idg PDFLoren Orozco0% (1)
- Pertemuan 3Document8 pagesPertemuan 3Berkah Tania Sawitri PasaribuNo ratings yet
- Ob-Gyn - Pharmacology & Reproductive SystemsDocument72 pagesOb-Gyn - Pharmacology & Reproductive SystemsPrayana BanjarnahorNo ratings yet
- IntroductionDocument4 pagesIntroductionSam NautiyalNo ratings yet
- JR Kemo TitaDocument21 pagesJR Kemo TitaTitaPuspitasariNo ratings yet
- Brungi Hospital QuotationDocument2 pagesBrungi Hospital QuotationPurchase PNo ratings yet
- Biology Practicum ReportDocument6 pagesBiology Practicum ReportdrockriotNo ratings yet
- Senate Hearing, 108TH Congress - Embryonic Stem Cell Research: Exploring The ControversyDocument87 pagesSenate Hearing, 108TH Congress - Embryonic Stem Cell Research: Exploring The ControversyScribd Government Docs100% (1)
- The Role of Fever in The PastDocument6 pagesThe Role of Fever in The PastAhmet YıdızNo ratings yet
- Intensified Testing For Attention-Deficit Hyperactivity Disorder (ADHD) in Girls Should Reduce Depression and Smoking in Adult Females ADocument4 pagesIntensified Testing For Attention-Deficit Hyperactivity Disorder (ADHD) in Girls Should Reduce Depression and Smoking in Adult Females ARafael MartinsNo ratings yet
- Performance Measures For Upper Gastrointestinal Endoscopy: A European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement InitiativeDocument22 pagesPerformance Measures For Upper Gastrointestinal Endoscopy: A European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement InitiativeMadalina StoicescuNo ratings yet