Professional Documents
Culture Documents
31c Autoimmune Hemolytic Anemia
31c Autoimmune Hemolytic Anemia
Uploaded by
murali_bharadwazCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
31c Autoimmune Hemolytic Anemia
31c Autoimmune Hemolytic Anemia
Uploaded by
murali_bharadwazCopyright:
Available Formats
Immunohemolytic Anemia o Antibodies bind to red cells, leading to their premature destruction.
o Diagnosis requires the detection of antibodies and/or complement on red cells from the patient o direct Coombs antiglobulin test patient's red cells are mixed with sera containing antibodies that are specific for human immunoglobulin or complement. (MCQ) If either immunoglobulin or complement is present on the surface of the red cells, the multivalent antibodies cause agglutination, which is easily appreciated visually as clumping. o indirect Coombs antiglobulin test patient's serum is tested for its ability to agglutinate commercially available red cells bearing particular defined antigens This test is used to characterize the antigen target temperature dependence of the responsible antibody Warm Antibody Type. This is the most common form of immunohemolytic anemia(MCQ) About 50% of cases are idiopathic (primary); (MCQ) Most causative antibodies are of the IgG class; less commonly, IgA (MCQ) The red cell hemolysis is mostly extravascular(MCQ) IgG-coated red cells bind to Fc receptors on phagocytes, which remove red cell membrane during partial phagocytosis. the loss of membrane converts the red cells to spherocytes, which are sequestered and removed in the spleen. Moderate splenomegaly due to hyperplasia of splenic phagocytes is usually seen. (MCQ) Antigenic drugs. hemolysis usually follows large, intravenous doses of the offending drug occurs 1 to 2 weeks after therapy is initiated Seen in penicillin and cephalosporins, quinidine(MCQ) Tolerance-breaking drugs(MCQ) -methyldopa is the prototype produce of antibodies against red cell antigens, particularly the Rh blood group antigens. Cold Agglutinin Type immunohemolytic anemia caused by IgM antibodies (MCQ) bind red cells avidly at low temperatures (04C) (MCQ) they appear transiently following certain infections, such as with (MCQ)
Mycoplasma pneumonia Epstein-Barr virus cytomegalovirus, influenza virus human immunodeficiency virus (HIV). In these settings the disorder is self-limited antibodies rarely induce clinically important hemolysis. Chronic cold agglutinin immunohemolytic anemia occurs in association with certain B-cell neoplasms or as an idiopathic condition. (MCQ) more difficult to treat unlike antibody immunohemolytic anemia Vascular obstruction caused by agglutinated red cells results in pallor, cyanosis, and Raynaud phenomenon in body parts exposed to cold temperature. (MCQ) Cold Hemolysin Type. Cold hemolysins autoantibodies responsible for an unusual entity known as paroxysmal cold hemoglobinuria. causes substantial, sometimes fatal, intravascular hemolysis and hemoglobinuria. (MCQ) The autoantibodies are IgGs (MCQ) IgGs bind to the P blood group antigen on the red cell surface in cool, peripheral regions of the body. (MCQ) Complement-mediated lysis occurs when the cells recirculate to warm central regions, since the complement cascade functions more efficiently at 37C. (MCQ) Most cases are seen in children following viral infections; in this setting the disorder is transient, and most of those affected recover within 1 month. Hemolytic Anemia Resulting from Trauma to Red Cells seen in individuals with cardiac valve prostheses Artificial mechanical cardiac valves are more frequently implicated than are bioprosthetic porcine valves(MCQ) Microangiopathic hemolytic anemia Causes (MCQ) most commonly seen with disseminated intravascular coagulation thrombotic thrombocytopenic purpura (TTP) hemolytic-uremic syndrome (HUS) malignant hypertension systemic lupus erythematosus, disseminated cancer. The common pathogenic feature in these disorders is a microvascular lesion that results in luminal narrowing, often due to the deposition of fibrin and platelets. These vascular changes produce shear stresses that mechanically injure passing red cells
. Regardless of the cause, traumatic damage leads to the appearance of (MCQ) red cell fragments (schistocytes), burr cells, helmet cells, triangle cells in blood smears
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Perspectives From Parents of Children With and Without ExceptionalitiesDocument103 pagesPerspectives From Parents of Children With and Without ExceptionalitiesFranNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Fastigial Nuclei) .: Cerebellar LobesDocument6 pagesFastigial Nuclei) .: Cerebellar Lobesmurali_bharadwazNo ratings yet
- Vertebral Arteries, and Their Divisions. Arteries Fuse To Form The Basilar ArteryDocument6 pagesVertebral Arteries, and Their Divisions. Arteries Fuse To Form The Basilar Arterymurali_bharadwazNo ratings yet
- UDIPDocument156 pagesUDIPVaishnavi JayakumarNo ratings yet
- Hegel: Elements of The Philosophy of RightDocument570 pagesHegel: Elements of The Philosophy of Rightpointedstick100% (2)
- Active and Inactive FaultsDocument19 pagesActive and Inactive FaultsRina Moreno100% (2)
- Detailed Lesson Plan Order of Adjectives Final DemoDocument8 pagesDetailed Lesson Plan Order of Adjectives Final DemoJennifer Padolina100% (15)
- ECO 112 (Test II, Set Paper I)Document4 pagesECO 112 (Test II, Set Paper I)Wisdom Thuso Sepepe Jr.No ratings yet
- Internal Control - Hayes - Chapter 6Document44 pagesInternal Control - Hayes - Chapter 6saif khanNo ratings yet
- Plan CL XI MoldovaDocument6 pagesPlan CL XI MoldovaNatalia Naumiuc ȚîrdeaNo ratings yet
- Quiz 3Document6 pagesQuiz 3murali_bharadwazNo ratings yet
- Quiz 2Document8 pagesQuiz 2murali_bharadwazNo ratings yet
- Quiz 1Document8 pagesQuiz 1murali_bharadwazNo ratings yet
- Brain Gross AnatomyDocument5 pagesBrain Gross Anatomymurali_bharadwazNo ratings yet
- The Auditory System: NeuraxisDocument2 pagesThe Auditory System: Neuraxismurali_bharadwazNo ratings yet
- Medullar Oblongata (Myelencephalon) Gastrointestinal MotilityDocument10 pagesMedullar Oblongata (Myelencephalon) Gastrointestinal Motilitymurali_bharadwazNo ratings yet
- 1 Contraception Part 1Document9 pages1 Contraception Part 1murali_bharadwazNo ratings yet
- Presented To CD4+ T Cells. (MCQ) Damage and The Characteristic Mucosal PathologyDocument3 pagesPresented To CD4+ T Cells. (MCQ) Damage and The Characteristic Mucosal Pathologymurali_bharadwazNo ratings yet
- 33 Polycystic Kidney DiseaseDocument2 pages33 Polycystic Kidney Diseasemurali_bharadwaz100% (1)
- Aiims May 2013 Transfer 6Document6 pagesAiims May 2013 Transfer 6murali_bharadwazNo ratings yet
- Aiims May 2013 Transfer 6Document6 pagesAiims May 2013 Transfer 6murali_bharadwazNo ratings yet
- 33 Polycystic Kidney DiseaseDocument2 pages33 Polycystic Kidney Diseasemurali_bharadwaz100% (1)
- Red Cells or White Cells.: g/100 Ml. (MCQ)Document7 pagesRed Cells or White Cells.: g/100 Ml. (MCQ)murali_bharadwazNo ratings yet
- RickricketsDocument30 pagesRickricketsmurali_bharadwazNo ratings yet
- Celiac Disease PresentationDocument24 pagesCeliac Disease Presentationmurali_bharadwazNo ratings yet
- DR Murali Bharadwaz Classes For APPGDocument6 pagesDR Murali Bharadwaz Classes For APPGmurali_bharadwazNo ratings yet
- The Long Way Down ReviewDocument4 pagesThe Long Way Down Reviewapi-608661248No ratings yet
- The Woods Heritage School First Term Examination Class - XII Subject - English Language MM: 80Document3 pagesThe Woods Heritage School First Term Examination Class - XII Subject - English Language MM: 80rockyrocksjhsNo ratings yet
- AVMM MasterDocument3 pagesAVMM MasterNidhiNo ratings yet
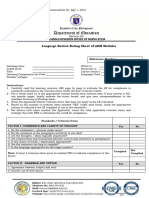
- Language Evaluation Rating Sheet of ADM ModulesDocument4 pagesLanguage Evaluation Rating Sheet of ADM ModulesPrincess SupnetNo ratings yet
- ContinueDocument2 pagesContinueramuji414No ratings yet
- 208 - Labor Law Suggested Answers (1994-2006), WordDocument108 pages208 - Labor Law Suggested Answers (1994-2006), WordNathalie QuinonesNo ratings yet
- 2016F CHE313 Course SyllabusDocument3 pages2016F CHE313 Course SyllabusthescienceguyNo ratings yet
- Class 4 First Three Months in School: Answer The QuestionsDocument10 pagesClass 4 First Three Months in School: Answer The QuestionsMichiyo ShimboNo ratings yet
- Lot 2,3,4 E-Auction - Process - DocumentDocument37 pagesLot 2,3,4 E-Auction - Process - DocumentVishalNo ratings yet
- First Friday Mass LetterDocument8 pagesFirst Friday Mass LetterMari VicNo ratings yet
- Overview of Literary Periods and MovementsDocument92 pagesOverview of Literary Periods and MovementsZarah Joyce SegoviaNo ratings yet
- Demoniality. Inccubi and Succubi-17th-CDocument292 pagesDemoniality. Inccubi and Succubi-17th-CKika SuperbruixaNo ratings yet
- October 2017 C34Document44 pagesOctober 2017 C34Noura TomNo ratings yet
- GUI For Error Correction and DetectionDocument10 pagesGUI For Error Correction and Detectionbezawit hailemariamNo ratings yet
- Use of The Mini International Neuropsychiatric Interview (MINI) As A Screening Tool in Prisons: Results of A Preliminary StudyDocument5 pagesUse of The Mini International Neuropsychiatric Interview (MINI) As A Screening Tool in Prisons: Results of A Preliminary StudyRafael MartinsNo ratings yet
- Effectiveness of Comparative AdvertisementDocument25 pagesEffectiveness of Comparative AdvertisementSadiq SagheerNo ratings yet
- Identity Portraits Lesson Plan - Jordan MeyerDocument3 pagesIdentity Portraits Lesson Plan - Jordan Meyerapi-486623744No ratings yet
- Student Name: Elisia-Martha Shinedhima STUDENT #: 215083903 COURSE: Business Ethics DUE DATE: 26 OCTOBER, 2020. QUESTION: Assignment 1Document4 pagesStudent Name: Elisia-Martha Shinedhima STUDENT #: 215083903 COURSE: Business Ethics DUE DATE: 26 OCTOBER, 2020. QUESTION: Assignment 1Boris PichlerbuaNo ratings yet
- Corporate Culture SurveyDocument2 pagesCorporate Culture SurveyNoli ChristianNo ratings yet
- Third Division: L/epublic of Tbe T) Btlippineg $upreme LtourtDocument16 pagesThird Division: L/epublic of Tbe T) Btlippineg $upreme Ltourtsandra mae bonrustroNo ratings yet
- Brinas V People G.R. No. 254005Document9 pagesBrinas V People G.R. No. 254005weddanever.cornelNo ratings yet
- Introduction To Islamic EconomicsDocument7 pagesIntroduction To Islamic EconomicsSalman ButtNo ratings yet