Professional Documents
Culture Documents
Bloodborne Pathogens: Histology Laboratory
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bloodborne Pathogens: Histology Laboratory
Copyright:
Available Formats
HISTOLOGY LABORATORY
BLOODBORNE PATHOGENS
EXPOSURE CONTROL PLAN
CONTENTS 1 Definitions ............................................................................................................3
2 Exposure determination ..............................................................................6 2.1 Job classification 2.2 High risk 2.3 Low risk 2.4 Notification of exposure 3 Methods of compliance .................................................................................8 3.1 Universal precautions 3.2 Engineering controls 3.3 Work practice controls 3.4 Personal protective equipment 4 Vaccinations and post-exposure evaluation 4.1 Availablity 4.2 Procedure 4.3 References Hepatitis B vaccine declination .............................11
5 Training ................................................................................................................14 5.1 Provision 5.2 Topics of instruction 5.3 Documentation 6 Record keeping ................................................................................................14 6.1 Required records 6.2 Record maintenance
Bloodborne Pathogens
1 Definitions 1.1 Blood Human blood, human blood components, and products made from human blood Bloodborne pathogen Any pathogenic microorganism that is present in human blood and can cause disease in humans; these pathogens include, but are not limited to, hepatitis B virus (HBV) and human immunodeficiency virus (HIV) Clinical laboratory A workplace where diagnostic or other screening procedures are performed on blood or other potentially infectious materials Contaminated Having the reasonably anticipated presence of blood or other potentially infectious materials on an item or surface Contaminated laundry Laundry which may contain sharps or has been soiled with blood or other potentially infectious material Contaminated sharps Any contaminated object that can penetrate the skin including, but not limited to, needles, scalpels, broken glass, broken capillary tubes, and exposed ends of dental wires Decontamination The use of physical or chemical means to remove, inactivate, or destroy bloodborne pathogens on a surface or item to the point where they are no longer capable of transmitting infectious particles and the surface or item is rendered safe for handling, use, or disposal
1.2
1.3
1.4
1.5
1.6
1.7
Bloodborne Pathogens
1.8
Engineering controls Controls such as sharps disposal containers and self-sheathing needles that isolate or remove the hazard of bloodborne pathogens Exposure incident A specific eye, mouth, other mucous membrane, non-intact skin, or parenteral contact with blood or other potentially infectious materials that results from the performance of an employee's duties
1.9
1.10 Handwashing facilities A facility providing an adequate supply of running potable water, soap and single use towels or hot air drying machines 1.11 Licensed health care professional One whose legally permitted scope of practice allows them to independently perform the activities required in administering the hepatitis B vaccination and performing post-exposure evaluation and follow-up; these services include ordering appropriate laboratory tests, determining contraindications to vaccination, and providing post-exposure prophylaxis and counseling. 1.12 Occupational exposure Reasonably anticipated skin, eye, mucous membrane, or parenteral contact with blood or other potentially infectious materials that may result from the performance of an employee's duties 1.13 Other potentially infectious materials The following human body fluids: semen, vaginal secretions, cerebrospinal fluid, synovial fluid, pleural fluid pericardial fluid, peritoneal fluid, amniotic fluid, saliva in dental procedures, any body fluid that is visibly contaminated with blood, and all body fluids in situations where it is difficult or impossible to differentiate between body fluids Any unfixed tissue or organ (other than intact skin) from a human (living or dead)
Bloodborne Pathogens
HIV-containing cell or tissue cultures, organ cultures, and HIV or HBV-containing culture medium or other solutions and blood, organs, or other tissues from experimental animals infected with HIV or HBV
1.14 Parenteral Piercing mucous membranes or the skin barrier through such events as needlesticks, human bites, cuts, and abrasions 1.15 Personal protective equipment Specialized clothing or equipment worn by an employee for protection against hazards; general work clothes such as uniforms, pants, shirts or blouses not intended to function as protection are not considered to be personal protective equipment 1.16 Regulated waste Liquid or semi-liquid blood or other potentially infectious materials Contaminated items that would release blood or other potentially infectious materials in a liquid or semi-liquid state if compressed Items that are caked with dried blood or other potentially infectious materials and are capable of releasing these materials during handling Contaminated sharps Pathological and microbiological wastes containing blood or other potentially infectious materials 1.17 Source individual Any individual, living or dead, whose blood or other potentially infectious materials may be a source of occupational exposure to the employee; examples include, but are not limited to, hospital and clinical patients clients in institutions for the developmentally disabled trauma victims clients of drug and alcohol treatment facilities residents of hospices and nursing homes
Bloodborne Pathogens
human remains individuals who donate or sell blood or blood components 1.18 Sterilization The use of a physical or chemical procedure to destroy a l l microbial life including highly resistant bacterial endospores 1.19 Universal precautions An approach to infection control in which all human blood and certain human body fluids are treated as if known to be infectious for HIV, HBV, and other bloodborne pathogens 1.20 Work practice controls Controls that reduce the likelihood of exposure by altering the manner in which a task is performed, for example, prohibiting recapping of needles by a two-handed technique. 1.21 Reference Federal Register. 58, no. 235 (6 December 1991), Rules and Regulations. Microfiche. 2 Exposure determination Laboratory regulations seek to l i m i t employees occupational exposure to blood and other potentially infectious materials as the result of performing their job duties. OSHA has not attempted to list all situations where exposures could occur. "Good Samaritan" acts such as assisting a co-worker with a nosebleed are not considered occupational exposure. Caution must be used when working in the histology laboratory. One never knows if a surface or item has been contaminated. One cannot be positive that a tissue specimen has been completely fixed. Any incidents of unexpected exposure should be documented and reported in the quality assurance minutes. 2.1 Job classification Exposure risk determination is made for histology and surgical pathology job classifications where occupational exposure to human blood and other potentially infectious materials such as
Bloodborne Pathogens
unfixed tissue specimens occurs. The determination is made without personal protective equipment. 2.2 High risk The following duties, usually performed by the surgical pathology assistant or the grossing room attendant, are high risk: handling leaking or contaminated specimen containers working with frozen sections that involve handling fresh unfixed human tissue including freezing specimens sectioning in the cryostat washing off freezing compound prior to fixation grossing specimens (cassetting, cutting in) that involve handling unfixed and fixed human tissue and organs examining and handling specimens as when searching for lymph nodes sectioning to obtain the proper size for processing wrapping small specimens in paper prior to cassetting sawing bone or calcified specimens with the band saw or Beuhler bone saw using disposable needlesdisposable needles should never be recapped; the syringe and needle combined should be disposed of in the sharps container cleaning up and disinfecting counter tops, cryostats, and refrigerators.
2.3
Low risk Low risk duties include those performed by the histology tecnicians, histology supervisor, and laboratory aides: picking up, grossing and cassetting kidney biopsies fixing, decalcifying, and cassetting bone marrow biopsies loading tissue processors and handling contaminated specimen containers such as with autopsy cases staining frozen sections and touch prep slides (smears) handling processed tissue sections (there is a slight risk in CJD infected brain cases) cleaning counters
Bloodborne Pathogens
2.4
cleaning tissue processors returning dirty specimen containers to autopsy
Notification of exposure Employees must report illness or exposure to possible infectious materials immediately to the supervisor and to employee health. Documentation should be maintained in employees personnel file.
3 Method of compliance 3.1 Universal precautions Universal precautions should be observed to prevent contact with blood and other potentially infectious materials. All body fluids and unfixed tissue from a human (living or dead) should be considered potentially infectious. Universal precautions are followed by environmental services as well as laboratory employees. All garbage is treated as infectious and disposed of in a specified landfill for hospital waste, in accordance with state regulations. Engineering controls Engineering controls are a means of isolating or removing bloodborne pathogens from the workplace. These must be provided by the employer. Sharps containers Sharps containers are closable, puncture resistant and leakproof on the sides and bottom. They should be used to dispose of anything that could puncture or cut the skin such as razor and microtome blades, pipettes, needles, cover glasses and glass slides. Sharps containers should not be overfilled and should be kept closed. When containers are full, environmental services should be called for pick-up and replacement. Regulated waste All waste in the laboratory is regulated. Garbage cans are provided by environmental services and are lined with brown plastic bags. Garbage cans are be emptied daily.
3.2
3.2.1
3.2.2.
Bloodborne Pathogens
Specimen containers should be emptied before being disposed of in garbage cans. All contaminated paper towels and gloves should be disposed of in garbage cans. Glass bottles should be placed in a large yellow trash can labeled, GLASS. Broken glassware should be disposed of in the sharps container. 3.2.3 Contaminated laundry On site linen services follows universal precautions. Contaminated laundry should be placed in the bags provided by linen services. If laundry is wet, it should be placed in a leakproof bag. Specimen containers If specimen containers are to stay on site, universal precautions are followed and they do not need to be labeled as biohazard; containers that will be used outside of the hospital must be show the biohazard label. Specimen containers must be closable and leakproof. If leakage does occur, the container should be placed in a secondary leakproof container with appropriate labeling. Handwashing facilities Sinks with soap and paper towel dispensers are located in each laboratory. Dispensers are filled by environmental services as needed. Work practice controls Handwashing Wash hands immediately after any exposure to blood or other potentially infectious materials, immediately after removing gloves, and before leaving the laboratory. Housekeeping Countertops should be cleaned with either chlorine bleach (sodium hypochlorite), or cyclophene. Wipe down countertops as soon as possible after exposure. Replace protective coverings and absorbent materials as soon as feasible when they become contaminated.
3.2.4
3.2.5
3.3 3.3.1
3.3.2
Bloodborne Pathogens
3.3.3
Equipment Equipment should be decontaminated if possible before being serviced. A biohazard label should be affixed to the portions which remain contaminated. Eating, drinking, smoking, and cosmetics Eating, drinking, smoking, applying cosmetics or lip balm, and handling contact lenses are prohibited in the histology laboratory and in the surgical pathology laboratory. Food and drink should not be kept in refrigerators, freezers, shelves, cabinets or on countertops or bench tops where blood or other potentially infectious materials are kept. Splashes All procedures involving blood or other potentially infectious materials should be performed in such a manner as to minimize splashing, spraying, spattering, and generation of droplets of these substances. Mouth pipetting Mouth pipetting and mouth suctioning of blood or other potentially infectious materials is prohibited. Personal protective equipment Personal protective equipment is ordered by the histology supervisor. Employees are responsible for requesting new orders when supplies are low. Gloves Small, medium, and large sizes of latex disposable gloves are kept in the lab. Gloves are to be worn when any possible contact with potentially infectious materials exists. Gloves should be changed as soon as feasible after contamination and should not be worn out of the laboratory. Safety glasses, goggles, and face shields Safety glasses, goggles and face shields should be worn when there is a possibility of a splash, spray, or spatter of blood or body fluids, such as when grossing specimens.
3.3.4
3.3.5
3.3.6
3.4
3.41
3.4.2
Bloodborne Pathogens
10
They should be disinfected after use with a 5% bleach solution. 3.4.3 Aprons, gowns, lab coats, and sleeves Whenever the possibility of occupational exposure exists, aprons, gowns, lab coats, and sleeves should be worn, as appropriate. Aprons and sleeves are disposable and lab coats and gowns should be placed in the laundry. These items should not be worn outside of the work area.
4 Immunizations 4.1 Availability Preventative immunizations including diphtherria/tetanus, MMR vaccine, and influenza are free to employees. The hepatitis B vaccine is available, free of charge, to employees who have had occupational exposure to blood or other potentially infectious materials. The hepatitis B vaccination is advised for histology and surgical pathology laboratory personnel. If the vaccination is refused, a signed declination (see following page) must be kept in the employees file. Employees may rescind the declination at any time and receive the hepatitis series at no charge. Immunization records are maintained in employees personnel files and by employee health. Employees hired after July 1, 1989, must show proof of vaccination or be immunized with the MMR vaccine. 4.2 Procedure Vaccinations will be administered by an occupational health nurse who will follow up with employees who have had direct contact with communicable disease or infectious materials. Antibody levels will be checked for all employees who have had exposure to infectious disease. References University of Utah Medical Center policy and procedure manual. 1:21, 1-35-38, 1:40-47.
4.3
Bloodborne Pathogens
11
Federal Registry, OSHA. Occupational exposure to bloodborne pathogens. Final rule, 29 CFR Part 1910.1030, 12-6-91.
Bloodborne Pathogens
12
HEPATITIS B VACCINE DECLINATION
I understand that due to my occupational exposure to blood or other potentially infectious materials I may be at risk of infection with the hepatitis B virus (HBV). I have been given the opportunity to be vaccinated with hepatitis B vaccine at no charge to myself. However, I decline hepatitis B vaccination at this time. I understand that by declining this vaccine, I continue to be at risk of acquiring hepatitis B, a serious disease. If in the future I continue to have occupational exposure to blood or other potentially infectious materials and I want to be vaccinated with hepatitis B vaccine, I may receive the vaccination series at no charge to me.
Signed
Date
Bloodborne Pathogens
13
5 Training 5.1 Provision An occupational health nurse w i l l educate employees in hospital hazards and responsible health and safe work practices annually as scheduled by the laboratory supervisor. New employees receive initial training during orientation. For specific job procedures, the lab supervisor w i l l train employees and provide written procedure descriptions. Topics of instructions Training should include protective equipment hand washing disinfection procedures disposal of contaminated and used supplies handling of contaminated laundry vaccinations accidental exposure procedures. Documentation Documentation of all training is retained in employee f i l e s under Infection Control.
5.2
5.3
6 Record keeping 6.1 Required records Records indicating incidents of occupational exposure should be kept for each employee. Employee files should include employees social security number hepatitis B vaccination record any follow-up procedures relating to vaccinations any follow-up, professional written opinions, and other information provided in the event of accidental exposure record of training sessions Record maintenance This information should be kept confidential and not disclosed without the written consent of the employee. Upon termination, employees files should be delivered to the
6.2
Bloodborne Pathogens
14
personnel resource department. This information will be retained for the duration of employment plus 30 years.
Bloodborne Pathogens
15
You might also like
- Practical Manual for Detection of Parasites in Feces, Blood and Urine SamplesFrom EverandPractical Manual for Detection of Parasites in Feces, Blood and Urine SamplesNo ratings yet
- Tuberculosis Prevention Plan: Histology LaboratoryDocument10 pagesTuberculosis Prevention Plan: Histology LaboratoryLynel Joy JamotilloNo ratings yet
- Urinalysis and Other Body FluidsDocument64 pagesUrinalysis and Other Body FluidsJahre Mark ToledoNo ratings yet
- Standard Operating Procedures For HospitDocument62 pagesStandard Operating Procedures For HospitThanRMNo ratings yet
- Universal Precautions QuizDocument8 pagesUniversal Precautions Quizaakurugu366No ratings yet
- Is Universal PrecautionsDocument2 pagesIs Universal Precautionsgulamg21No ratings yet
- AUBF Lec - Lab Safety - QADocument12 pagesAUBF Lec - Lab Safety - QALeinard ClaveroNo ratings yet
- Universal Precautions Quiz 14 15Document8 pagesUniversal Precautions Quiz 14 15O.r. CadzNo ratings yet
- Introductory Microbiology Laboratory ManualDocument91 pagesIntroductory Microbiology Laboratory Manualasad bashirNo ratings yet
- Lecuniversal PrecautionsDocument34 pagesLecuniversal PrecautionsRabia TahirNo ratings yet
- PMLS2 2Document45 pagesPMLS2 2john dale duranoNo ratings yet
- Standard Operating Procedures For Hospitals in ChhattisgarhDocument62 pagesStandard Operating Procedures For Hospitals in ChhattisgarhFifty One71% (7)
- 2StandardOperatingProceduresforHospitals PDFDocument62 pages2StandardOperatingProceduresforHospitals PDFJoseph JordanNo ratings yet
- Biosafety and Biosecurity Lec. 5Document7 pagesBiosafety and Biosecurity Lec. 5Ali AlhadiNo ratings yet
- Community Lec3Document25 pagesCommunity Lec3woow0217No ratings yet
- 1-Bloodborne PathogensDocument10 pages1-Bloodborne PathogensazozinlcNo ratings yet
- EC-06-001 - Standard and Transmission Based PrecautionsDocument24 pagesEC-06-001 - Standard and Transmission Based PrecautionsBezawit YosefNo ratings yet
- WEEK 1 Safety, Quality Assessment and Laboratory OperationDocument8 pagesWEEK 1 Safety, Quality Assessment and Laboratory OperationDayledaniel SorvetoNo ratings yet
- Policies & Procedures: 1. PurposeDocument5 pagesPolicies & Procedures: 1. PurposeKâtēbhÃłwešâbÿNo ratings yet
- Laboratory SafetyDocument30 pagesLaboratory SafetyEliana Nicole IbongNo ratings yet
- Post Exposure Management Hepatitis B Hepatitis C and HivDocument39 pagesPost Exposure Management Hepatitis B Hepatitis C and HivQaiser ZamanNo ratings yet
- Module 5-Laboratory SafetyDocument5 pagesModule 5-Laboratory SafetyAllyah Ross DuqueNo ratings yet
- MAS110 - Week 1 - Infection Control Worksheet 2Document4 pagesMAS110 - Week 1 - Infection Control Worksheet 2geonikawilliamsNo ratings yet
- The Infection Control Manual: Standard PrecautionsDocument5 pagesThe Infection Control Manual: Standard Precautionszenagit123456No ratings yet
- Management (NURS350) Fish Bone Report: (Non-Compliance Medical Waste)Document16 pagesManagement (NURS350) Fish Bone Report: (Non-Compliance Medical Waste)Æli HußßienNo ratings yet
- Collection and Storage of Pecimen in The Lab: Expired ContainersDocument5 pagesCollection and Storage of Pecimen in The Lab: Expired ContainersClick QuantumNo ratings yet
- Guielines For How To Conduct A Risk AssessmentDocument9 pagesGuielines For How To Conduct A Risk AssessmentmichelepositinoNo ratings yet
- Sop BSL IiDocument7 pagesSop BSL IiBridget HaleyNo ratings yet
- Spillage Management: Arrangements AND GuidanceDocument10 pagesSpillage Management: Arrangements AND GuidanceRani KarditaNo ratings yet
- Biosafety and Universal Precautions in The LaboratoryDocument48 pagesBiosafety and Universal Precautions in The LaboratoryRosemary ShirimaNo ratings yet
- Bloodborne Pathogen Exposure Control PlanDocument6 pagesBloodborne Pathogen Exposure Control Planapi-630289708No ratings yet
- Safety in The Laboratory Activity 1Document72 pagesSafety in The Laboratory Activity 1Rollin Navora PamintuanNo ratings yet
- BiohazardsDocument103 pagesBiohazardsAman Preet SinghNo ratings yet
- Management of Blood and Body Fluids SpillsDocument24 pagesManagement of Blood and Body Fluids SpillsFarah Andleeb MalikNo ratings yet
- ادوات مختبرية نظري دكتور بوتانDocument49 pagesادوات مختبرية نظري دكتور بوتانThicc JimmyNo ratings yet
- UPDATED - Safety Exam Study GuideDocument30 pagesUPDATED - Safety Exam Study GuideAbhi KumarNo ratings yet
- Infection Control in Operation TheatreDocument8 pagesInfection Control in Operation Theatresyedsalimahmed100% (7)
- Hospital Hazards PresentationDocument30 pagesHospital Hazards Presentationkhizgaming worldNo ratings yet
- Reading Output 2Document10 pagesReading Output 2HalluxNo ratings yet
- Waste Management Sops English1122Document28 pagesWaste Management Sops English1122johnfolorunshoNo ratings yet
- Assignment of CoronaDocument5 pagesAssignment of CoronaOsamah AshrafNo ratings yet
- Laboratory Safety Guidelines: Learning Guide SeriesDocument6 pagesLaboratory Safety Guidelines: Learning Guide SeriesIberisNo ratings yet
- FALLSEM2021-22 BIT1025 TH VL2021220102462 Reference Material I 22-09-2021 Sterilization and Waste Management 1Document20 pagesFALLSEM2021-22 BIT1025 TH VL2021220102462 Reference Material I 22-09-2021 Sterilization and Waste Management 1Kartik SharmaNo ratings yet
- Module TM1:: 08 Understanding Clinical & Biomedical TerminologyDocument29 pagesModule TM1:: 08 Understanding Clinical & Biomedical TerminologyLarry CalubagNo ratings yet
- Housekeeping ManualDocument28 pagesHousekeeping Manualocinauj85% (41)
- Exposure Control Plan - Biological AgentsDocument10 pagesExposure Control Plan - Biological AgentsMr TibsNo ratings yet
- Hema 2 IntroDocument7 pagesHema 2 IntroMa. Renster RazNo ratings yet
- Risk Management in Medical LaboratoriesDocument32 pagesRisk Management in Medical Laboratoriesapanisile14142No ratings yet
- Management of Occupational Exposure To Blood and Body Fluids - NoRestrictionDocument28 pagesManagement of Occupational Exposure To Blood and Body Fluids - NoRestrictionJamilNo ratings yet
- Lib Study Point 2Document25 pagesLib Study Point 2Tanya SinghNo ratings yet
- Handling of Cytotoxic DrugsDocument27 pagesHandling of Cytotoxic DrugsMr VoralpenNo ratings yet
- Needle Sticks Sharps Injuries: FactsDocument31 pagesNeedle Sticks Sharps Injuries: FactsDr. Ashish Jawarkar67% (3)
- P P Template Infection Prevention For Point of Care TestingDocument2 pagesP P Template Infection Prevention For Point of Care TestingCarlo AlvaradoNo ratings yet
- Blood Borne Virus PDFDocument7 pagesBlood Borne Virus PDFmkbh10No ratings yet
- Bloodborne PathogensDocument2 pagesBloodborne PathogensAaquil RaziNo ratings yet
- Autoclaving ProtocolsDocument25 pagesAutoclaving ProtocolsSerene KennyNo ratings yet
- Sterilization of Ophthalmic Surgical Instruments and EquipmentDocument27 pagesSterilization of Ophthalmic Surgical Instruments and EquipmentMohammad Abdullah BawtagNo ratings yet
- Basics of Biosafety: Working Safely With Biological MaterialsDocument48 pagesBasics of Biosafety: Working Safely With Biological MaterialsSilky ChughNo ratings yet
- Haematology Analyser Comparison 2019+Document2 pagesHaematology Analyser Comparison 2019+Luis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
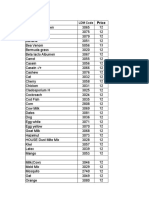
- Alfa Test ProfilesDocument1 pageAlfa Test ProfilesLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Single AllergenDocument2 pagesSingle AllergenLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- 8 Metabolic Conditioning Workouts For MMA FightersDocument5 pages8 Metabolic Conditioning Workouts For MMA FightersLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- OEC Exemption 2019Document1 pageOEC Exemption 2019Luis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Parameters LDM Machine Print Out CAP Result Ref Range Proficiency MIC Pol 2Document3 pagesParameters LDM Machine Print Out CAP Result Ref Range Proficiency MIC Pol 2Luis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- ChessDocument3 pagesChessLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- MicroDocument1 pageMicroLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Procedure: Non-SMILE Created Resources Author: N/A: Coulter A T 5 Diff Cap Pierce (CP) Operations ProcedureDocument12 pagesProcedure: Non-SMILE Created Resources Author: N/A: Coulter A T 5 Diff Cap Pierce (CP) Operations ProcedureLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- The Vert Specific Conditioning Guide : How Hard Can You Go and For How Long?.Document20 pagesThe Vert Specific Conditioning Guide : How Hard Can You Go and For How Long?.Luis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Dhoha R. HDocument1 pageDhoha R. HLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Team THUMP Txtbook PDFDocument20 pagesTeam THUMP Txtbook PDFLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Chest Day: Gaspari Nutrition: 7 Day Split Workout Workout Example 1Document3 pagesChest Day: Gaspari Nutrition: 7 Day Split Workout Workout Example 1Luis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Formaldehyde MSDS Mallinckrodt PDFDocument8 pagesFormaldehyde MSDS Mallinckrodt PDFLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Safety Data Sheet: 1. IdentificationDocument9 pagesSafety Data Sheet: 1. IdentificationLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- API System: 320 MBIO PracticalDocument24 pagesAPI System: 320 MBIO PracticalLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Api 20eDocument3 pagesApi 20eLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Microbiology Urine Culture 2019 2Document1 pageMicrobiology Urine Culture 2019 2Luis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Formaldehyde: 1. Product IdentificationDocument8 pagesFormaldehyde: 1. Product IdentificationLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Title: Microbiology Urine Screening Effective Date: 05/08/2013Document14 pagesTitle: Microbiology Urine Screening Effective Date: 05/08/2013Luis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Version 12 May 2013: BSAC Methods For Antimicrobial Susceptibility TestingDocument87 pagesVersion 12 May 2013: BSAC Methods For Antimicrobial Susceptibility TestingLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Version 12 Apr 2013 - Final12 PDFDocument87 pagesVersion 12 Apr 2013 - Final12 PDFLuis Ferdinand Dacera-Gabronino Gamponia-Nonan100% (1)
- Uti 11 30 PDFDocument6 pagesUti 11 30 PDFLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Formaldehyde MSDS Mallinckrodt PDFDocument8 pagesFormaldehyde MSDS Mallinckrodt PDFLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Selective Reporting of Antibiogram Results: ESCMID Online Lecture Library © by AuthorDocument44 pagesSelective Reporting of Antibiogram Results: ESCMID Online Lecture Library © by AuthorLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Sy0089 PDFDocument44 pagesSy0089 PDFLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Science Grade 7 Second QuarterDocument12 pagesScience Grade 7 Second QuarterAnneKARYLE67% (3)
- Augmentin Tablet Pi Ipi13 SiDocument11 pagesAugmentin Tablet Pi Ipi13 Siاسد راجNo ratings yet
- Tongue Conditions: ThrushDocument5 pagesTongue Conditions: ThrushMark TiongsonNo ratings yet
- 559 FullDocument12 pages559 FullAmatystNo ratings yet
- 6277-Article Text-44963-1-10-20221231Document10 pages6277-Article Text-44963-1-10-20221231Agus KarismaNo ratings yet
- 4 Life TestimoniesDocument87 pages4 Life TestimoniesBhavin VoraNo ratings yet
- Spondylosis, Cervical and LumbarDocument1 pageSpondylosis, Cervical and LumbarLuis HerreraNo ratings yet
- 03 Cutaneous MycosesDocument30 pages03 Cutaneous MycosesFelix AyornuNo ratings yet
- Practice Problems ADocument2 pagesPractice Problems ACrystal LynaeNo ratings yet
- Fdar Cabg 3nesurgicalDocument5 pagesFdar Cabg 3nesurgicalMary Margareth GonzalesNo ratings yet
- The Effect of Pursed - Lip Breathing Exercise Vs Diaphragmatic Breathing in Stabilizing The Vitals After 6-MWT Among Overweight Individuals-IJRASETDocument12 pagesThe Effect of Pursed - Lip Breathing Exercise Vs Diaphragmatic Breathing in Stabilizing The Vitals After 6-MWT Among Overweight Individuals-IJRASETIJRASETPublicationsNo ratings yet
- Nhis Drug Price List Final (2013 Ed)Document32 pagesNhis Drug Price List Final (2013 Ed)holuwadamilare935No ratings yet
- Pathogenesis of Non-Hodgkin's Lymphoma: Ournal of Linical NcologyDocument9 pagesPathogenesis of Non-Hodgkin's Lymphoma: Ournal of Linical NcologyZullymar CabreraNo ratings yet
- Swine Quiz Bowl QuestionsDocument6 pagesSwine Quiz Bowl QuestionsNezuko CutieeeNo ratings yet
- Charpak: New Evidences On The Kangaroo Mother Care MethodDocument51 pagesCharpak: New Evidences On The Kangaroo Mother Care MethodNewborn2013No ratings yet
- Ultrasound GuidanceDocument111 pagesUltrasound GuidanceRahmanandhikaNo ratings yet
- COMMON BEHAVIOURAL DISORDER OF CHILDREN AND MANAGEMENT .Edu TechDocument83 pagesCOMMON BEHAVIOURAL DISORDER OF CHILDREN AND MANAGEMENT .Edu Techjmbrand jmNo ratings yet
- NCRP Report No. 177 PDFDocument245 pagesNCRP Report No. 177 PDFVivien FerradaNo ratings yet
- Abdominal Swelling and Ascites: Global ConsiderationsDocument5 pagesAbdominal Swelling and Ascites: Global ConsiderationsJacob BorongNo ratings yet
- NOAC Trong Rung NhĩDocument23 pagesNOAC Trong Rung NhĩToan ngoNo ratings yet
- Advance Epi & Direct Acyclic GraphDocument14 pagesAdvance Epi & Direct Acyclic GraphPurnima VermaNo ratings yet
- Hiv Trends Pir RHWC DavaoDocument57 pagesHiv Trends Pir RHWC DavaoIsfahan MasulotNo ratings yet
- Down With Acid Chris RobinsonDWA3 Book DownloadDocument128 pagesDown With Acid Chris RobinsonDWA3 Book DownloadGabriel CassNo ratings yet
- Peritonitis Update On Pathophysiology, Clinical Manifestations, and PDFDocument11 pagesPeritonitis Update On Pathophysiology, Clinical Manifestations, and PDFAnonymous InJS6aYZ100% (1)
- Efektivitas Pemberian Ikan Gabus Kukus Terhadap Penyembuhan Laserasi Perineum Pada Ibu PostpartumDocument9 pagesEfektivitas Pemberian Ikan Gabus Kukus Terhadap Penyembuhan Laserasi Perineum Pada Ibu Postpartumjulimarni13No ratings yet
- Jemds Title PDocument1 pageJemds Title PKriti KumariNo ratings yet
- Neonatal Resuscitation: Presented By: Dr. Harish Uppala Chairperson: Dr. Kousalya Moderator: Dr. HemnathDocument23 pagesNeonatal Resuscitation: Presented By: Dr. Harish Uppala Chairperson: Dr. Kousalya Moderator: Dr. HemnathPraveen RamasamyNo ratings yet
- U.S. Patent 9,301,519, Entitled, Systems and Methods For Ex Vivo Organ Care, To Hassanein Et Al., Issued Apr. 5, 2016.Document106 pagesU.S. Patent 9,301,519, Entitled, Systems and Methods For Ex Vivo Organ Care, To Hassanein Et Al., Issued Apr. 5, 2016.Anonymous a7S1qyXNo ratings yet
- Optimal Management of Collagenous Colitis A Review 021016Document9 pagesOptimal Management of Collagenous Colitis A Review 021016Eliza DNNo ratings yet
- Project Biology 11Document15 pagesProject Biology 11ABHISHEK SinghNo ratings yet
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (30)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainFrom EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainRating: 4 out of 5 stars4/5 (95)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (61)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (59)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (45)