Professional Documents
Culture Documents
Tongue Tie AAPD 2004 Classification, Treatment
Uploaded by
Dilmohit SinghOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tongue Tie AAPD 2004 Classification, Treatment
Uploaded by
Dilmohit SinghCopyright:
Available Formats
Clinical Section
Ankyloglossia in the Infant and Young Child: Clinical Suggestions for Diagnosis and Management
Ari Kupietzky, DMD, MSc Eyal Botzer, DMD
Dr. Kupietzky is clinical instructor, Department of Pediatric Dentistry, Hebrew University-Hadassah School of Dental Medicine, and pediatric dentist in private practice, Jerusalem, Israel; Dr. Botzer is director, Division of Pediatric Dentistry, Tel Aviv Sourasky Medical Center, Tel Aviv, Israel. Correspond with Dr. Kupietzky at drkup@netvision.net.il
Abstract
Since the recommended time for a childs first dental visit is early, it is essential that pediatric dentists be familiar with all possible pathologies occurring during this early period of life. The parents of infants and toddlers who notice in their child a tonguetie (ankyloglossia) are likely to turn first to their pediatric dentist for advice and help. Treatment options such as observation, speech therapy, frenotomy without anesthesia, and frenectomy under general anesthesia have all been suggested in the literature. The purposes of this report are to describe ankyloglossia, its clinical significance, and the timing of treatment. The frenotomy procedure is presented for the pediatric dentist with clinical suggestions for the diagnosis and management of ankyloglossia.(Pediatr Dent. 2005;27:40-46) KEYWORDS: FRENOTOMY, FRENULOPLASTY, FRENECTOMY, ANKYLOGLOSSIA, TONGUE-TIE
Received May 3, 2004 Revision Accepted November 24, 2004
clinical section
ince the recommended time for a childs first dental visit is early, it is essential that the dentist be familiar with all possible pathologies occurring during this early period of life. Pediatric dentists are well acquainted with and capable of diagnosing and treating children over 2 years of age presenting with oral problems relating to the teeth and their supporting structures. The problems of infants 1 year of age or younger, however, may be less familiar to the dentist. The parents of infants and toddlers who notice in their child a tonguetie are likely to turn first to their dentist for advice and help. Lactation specialists in certain communities may refer infants with breast-feeding problems to the dentist for correction of ankyloglossia (AG) that they identified as being the cause of the childs feeding difficulties. The American Academy of Pediatric Dentistry guidelines1 call for a complete and thorough oral exam and evaluation of the infant at the first infant dental visit. Dentists who perform such services for infants should be prepared to provide therapy when indicated or be capable of identifying the need to refer the patient to an appropriately trained individual for necessary treatment. The purposes of this report are to describe AG, its clinical significance, and timing of treatment. The frenotomy
procedure is presented with clinical suggestions for the diagnosis and management of AG.
Definition, incidence, and clinical sequalae of ankyloglossia
AG (more commonly called tongue-tie) is a congenital anomaly characterized by an abnormally short lingual frenum, which may restrict tongue tip mobility.2 There is much controversy regarding this condition. Differences of opinion regarding its definition, clinical significance, need for surgical intervention, and timing of treatment may all be found in the scientific literature. Otolaryngologists, oral surgeons, pediatricians, speech therapists, and lactation consultants may all voice different opinions regarding the various aspects of AG.2-4 AG definitions range from vague descriptions of a tongue that functions with a less-than-normal range of activity to a specific description of the frenum being short, thick, muscular, or fibrotic.5-7 Others only designate AG as an extreme fixation of the tongue to the floor of the mouth; or as a minor limitation of movement not defined as AG. The plethora and variety of AG definitions in the literature suggests the lingering controversy regarding this condition and its clinical significance.
40
Kupietzky, Botzer
Diagnosis and management of ankyloglossia
Pediatric Dentistry 27:1, 2005
Table 1. Hazelbaker 19 The Assessment Tool for Lingual Frenulum Function Function items Lateralization 2=complete 1=body of tongue, but not tongue tip 0=none Lift of tongue 2=tip to mid-mouth 1=only edges to mid-mouth 0=tip stays at alveolar ridge or tip rises only to mid-mouth with jaw closure Extension of tongue 2=tip over lower lip 1=tip over lower gum only 0=neither of the above or anterior or mid-tongue humps Spread of anterior tongue 2=complete 1=moderate or partial 0=little or none Cupping of tongue 2=entire edge, firm cup 1=side edges only, moderate cup 0=poor or no cup Peristalis 2=complete anterior to posterior (originates at tip) 1=partial: originating posterior to tip 0=none or reverse peristalsis Snap-back 2=none 1=periodic 0=frequent or with each suck Scoring 14=perfect score (regardless of appearance item score) 11=acceptable if appearance item score is 10 <11=function impaired; frenotomy should be considered if management fails Frenotomy is necessary if function score is <11 and appearance score is <8 Appearance items Appearance of tongue when lifted 2=round or square 1=slight cleft in tip apparent 0=heart-shaped Elasticity of frenulum 2=very elastic 1=moderately elastic 0=little or no elasticity Length of lingual frenulum when tongue lifted 2=>1cm or embedded in tongue 1=1 cm 0=<1 cm Attachment of lingual frenulum to tongue 2=posterior to tip 1=at tip
clinical section
0=notched Attachment of lingual frenulum to inferior alveolar ridge 2=attached to floor of mouth or well below ridge 1=attached just below ridge 0=attached at ridge
Reprinted with permission from Alison K. Hazelbaker, MA, IBCLC, RLC.
Pediatric Dentistry 27:1, 2005
Diagnosis and management of ankyloglossia
Kupietzky, Botzer
41
Table 2. Classification of Ankyloglossia Based on Free Tongue Length* Clinically acceptable, normal range of free tongue=>16 mm Class I: mild ankyloglossia=12-16 mm Class II: moderate ankyloglossia=8-11 mm Class III: severe ankyloglossia=3-7 mm Class IV: complete ankyloglossia=<3 mm
*As per Kotlow.5
AG incidence varies from 0.02% to 5%, depending on the study, its definition of AG, and population examined.3,4,7-13 The incidence among outpatients of a childrens hospital with breast-feeding problems was almost 3 times higher (13%).4 Two independent studies of oral anomalies in neonates found a significant 3X predilection for AG in males.12,13 AG may occur with increased frequency in various congenital syndromes, including Opitz syndrome, orofaciodigital syndrome, Beckwith-Wiedemann syndrome, Simpson-Golabi-Behmel syndrome, and X-linked cleft palate.3
Figure 1. Newborn infant with significant ankyloglossia. The lingual frenum extends from the alveolar ridge to the tongue, preventing the tip of the tongue to lift to the mid-mouth when crying. The tongue resembles an arrow or heart shape.
clinical section
Sequlae
The possible sequlae of AG remain controversial, and the range of suggested complications is great. Among the suggestions found in the literature are: (1) lower incisor deformity; (2) gingival recession; and (3) malocclusions.14 It should be emphasized that, without further research, clinicians should not advise parents that the existence of AG will result in a malocclusion in their child. Although there is a lack of scientific evidence proving a relationship between speech disorders and AG, a consensus seemingly exists that AG is not a cause of a delay in speech onset. AG may interfere with articulation, however, as will be described in forthcoming detail. The existence of AG in the newborn may result in breastfeeding difficulties, including ineffective latch, inadequate milk transfer, and maternal nipple pain. An infant with AG may experience difficulty latching on to the nipple and may compress the nipple against the gum pad instead of the tongue, resulting in nipple pain and an inefficient, inadequate seal. A mother experiencing such pain may often contemplate switching the baby to a bottle. Indiscriminate or immediate clipping of all or most lingual frenula, however, is not universally recommended. It is crucial to understand the mechanism of feeding and its relationship with oral structures to comprehend the suggested role of AG in feeding problems. Many of the reports on this suggested mechanism are anecdotal,15-17 and evidence-based studies are lacking. A recent study of 3,000 infants concluded that: 1. AG represents a significant proportion of breast-feeding problems. 2. Surgical interventions in the presence of significant AG facilitated successful and improved breast-feeding.4
Dentists are encouraged to learn more about the mechanisms of breast-feeding in the lactation literature. AG may have sequalae beyond those of speech or feeding difficulties. Children may be teased by their peers for their anomaly. Social issues include the inability to lick ice cream, play a musical wind instrument, and even kiss.5
Clinical assessment in infant
A thorough intraoral exam should be performed on the infant. Inspection of the tongue and its function should be part of the routine first dental visit. Parents should be advised regarding the presence and severity of AG and made aware of potential feeding, speech, and dental problems.4 The newborn exam may show a membrane attached between the tip and middle portion of the tongues inferior aspectextending to the anterior floor of the mouth, just beneath or directly onto the alveolar ridge. The clinician should examine the tongues appearance when the tongue is lifted as the infant cries or tries to extend the tongue4 (Figure 1). While lifting the infants tongue, the frenum should be palpated and its elasticity determined. The attachment of the frenum to the tongue should normally be approximately 1 cm posterior to the tongues tip. The frenums attachment to the inferior alveolar ridge should be proximal to or into the genioglossus muscle on the floor of the mouth. The mother should be interviewed regarding the infants ability to breastfeed. Does the infant demonstrate frustration at the breast? Is the infant experiencing inability to sustain a good latch to the nipple? Does the mother experience any nipple pain or discomfort while the infant nurses? If any of these factors are present, a lactation specialist should be consulted for breast-feeding assessment.
Clinical assessment in preschool/school-age patient
Although there is a lack of scientific evidence proving a true relationship between speech disorders and AG, there seems
42
Kupietzky, Botzer
Diagnosis and management of ankyloglossia
Pediatric Dentistry 27:1, 2005
to be a consensus that AG may be the cause of specific speech disorders in certain individuals. AG does not prevent or delay the onset of speech, but may interfere with articulation. A simple speech articulation test has been suggested. 14 Although dentists lack training in phonetic analysis, it is nonetheless possible for individuals other than speech pathologists to judge the accuracy of a sample of patient articulatory production.14 If the elevation of the tongue tip is restricted, the articulation of 1 or more of the tongue soundssuch as t, d, l, th, and swill not be accurate. The patient who can produce these sounds accurately is probably not a candidate for surgical correction. Patients who have difficulty should be referred to a speech pathologist for evaluation.14 As noted, it is important to remember that AG is not a cause of speech delay.3 Children with AG are expected to acquire speech and language at a normal rate, although some may experience articulation difficulties for certain speech sounds, as previously indicated. Occasionally, parents with a speech-delayed child may erroneously ascribe the delay to AG and demand surgical correction in the hope that normal speech and language will result.3 In such a patient, a potential cause such as audiologic or neurodevelopmental factors may be the etiology of the problem. Surgical repair should be delayed until obtaining the appropriate assessments and diagnosis. Several suggestions have been made in the literature regarding a systematic protocol for AG assessment, lingual function, and need to for surgical correction.14,18,19 Hazelbaker developed an assessment tool to quantify the function and appearance of the tongue in infants with AG.19 The scoring and examination method is presented in Table 1. Kotlow introduced a simple classification, measuring the free tongue.5 This method can be used in older patients as well as infants. The term free tongue is defined as the tongues length from the insertion of the lingual frenum into the tongues base to the tongues tip. The categories and definitions of Kotlows protocol are presented in Table 2. Lalakea recommended measuring lingual mobility in children and tongue elevation to document and define the degree of restriction and AG.3 Mobility is evaluated by measuring in millimeters the tip of the tongue extended past the lower dentition. Elevation is measured by recording interincisal distance with the tongue tip maximally elevated and in contact with the upper teeth. Typically, children with AG have protrusion and elevation values of 15 mm or less, and 20 to 25 mm or greater in normal children. Clinicians should remember that, despite all the methods previously mentioned, currently there is no way based on examination to predict which children are likely to develop speech or mechanical symptoms related to their AG.3 Lalakea suggested that, given the minor nature of the surgery and significant potential for speech difficulties and later social and mechanical problems, it may be appropriate to consider surgery for children with significant AG at any age, including infants and toddlers who have yet to demonstrate
overt symptoms. Parents should be informed that there is no way to predict which children will develop symptoms related to their condition and which may outgrow their condition. Although early intervention in all children may be unwarranted, delaying intervention until obvious difficulties emerge may commit some children unnecessarily to a period of speech therapy and social embarrassment. Another consideration is that up to several months of age, a frenotomy can be performed quickly in the clinic without requiring general anesthesia (GA). In contrast, if surgery is deferred until the child is older, GA is usually required if a frenectomy is performed. Frenotomy can be accomplished, however, in children older than 1 year using conscious sedation (ie, nitrous oxide/oxygen inhalation with oral premedication). It should be noted that some experts categorically state that frenotomy should not be performed before 4 to 5 years of age.6,20
Treatment
Several AG treatment methods have been suggested. Management approaches range from very early treatment without anesthesia to the other extremethat AG should never be treated.21 Physicians may often delay recommending treatment of a short lingual attachment unless there are obvious speech or nursing difficulties.5 Treatment options such as observation, speech therapy, frenotomy without anesthesia, and frenectomy under GA have all been suggested in the literature.
clinical section
Clinical procedure
Frenotomy technique3,4 (Figure 2) The frenotomy procedure is defined as the cutting or division of the frenum. The procedure may be accomplished without local anesthesia and with minimal discomfort to the infant.4 The discomfort associated with the release of thin and membranous frena is brief and quite minor.3 The authors, however, highly recommend the use of topical anesthetic gel for pain control and to alleviate any parental concerns. Other clinicians suggest always using local anesthesia regardless of the age or extent of the attachment.21 The parent or an assistant holds and stabilizes head. The infant is placed supine with the elbows held securely close to the body. The tongue is lifted gently with sterile gauze and stabilized exposing the frenum. This may be achieved by the placement of 2 gloved fingers of the clinicians left hand placed below the tongue on either side of the midline, retracting the tongue upward toward the palate and exposing the frenum (Figures 2A and 2B). The frenum is then divided with small sterile scissors at its thinnest portion (Figure 2C). The incision begins at the frenums free border and proceeds posteriorly, adjacent to the tongue. This is necessary to avoid injury to the more inferiorly placed submandibular ducts in the floor of the mouth. Occasionally, complete release may be accomplished with a single scissors cut. More frequently, however, especially
Pediatric Dentistry 27:1, 2005
Diagnosis and management of ankyloglossia
Kupietzky, Botzer
43
Figure 2A. The frenotomy procedure in a 1-week-old infant who had presented with breast-feeding difficulties.
Figure 2B. A topical anesthetic may be applied. Only a thin and membranous frenum should be corrected with the frenotomy procedure, as can be seen in this case. Frena of thicker and more fibrous/vascular nature are contraindicated for this procedure.
clinical section
Figure 2C. The frenum is divided with small sterile scissors at its thinnest portion and above the submandibular salivary gland ducts.
Figure 2D. Postoperative view immediately following first incision. Occasionally, complete release may be accomplished with a single scissors cut, but more frequently, 2 or 3 sequential cuts are required.
Figure 2E. The procedure is completed. There should be minimal blood loss. Bleeding can be controlled easily with a brief period of pressure applied with gauze. The incision is not sutured.
when the frenum is quite tight, 2 or 3 sequential cuts are required; each cut provides some release, allowing improved retraction and visualization for subsequent cuts.4 Care is taken not to incise any vascular tissue. The frenum is poorly vascularized and innervated, allowing the clinician to accomplish the procedure without any complications. There should be minimal blood loss (ie, no more than a drop or two, collected on sterile gauze3; Figure 2E). If needed, bleeding can be controlled easily with a brief period of pressure applied with gauze. The incision is not sutured (Figure 2E). Crying is usually limited to the time the infant is restrained. Feeding may be resumed immediately and is without apparent infant discomfort. No specific follow-up care is required, except that breast milk is recommended for at least the next few feedings. Acetaminophen may be used for pain control, but is usually not necessary. Parents should be advised that a postoperative white fibrin clot might be seen to form at the incision site during the first couple of days. The parents should be reassured that it is
44
Kupietzky, Botzer
Diagnosis and management of ankyloglossia
Pediatric Dentistry 27:1, 2005
Figure 3A. The frenectomy procedure in a 7-year-old boy, referred by a speech pathologist for surgical correction. Note the fibrous and thick attachment compared with a thin, membrane-like frenum, as illustrated in Figure 2B.
Figure 3B. Following release and division of the frenum, sutures were placed. Note the relative complexity of the incision as compared with that of the frenotomy.
clinical section
Figure 3C. Two-month postoperative view. Child is able to proximate the tongue to the buccal surface of maxillary incisors.
Figure 3D. Six months after surgery, the lingual frenum is fully healed.
Frenectomy (Figure 3) The frenectomy procedure is defined as the excision or removal of the frenum. Frenectomy is the preferred procedure for patients with a thick and vascular frenum where severe bleeding may be expected, and in some cases, reattachment of the frenum by scar tissue may occur. The procedure in young children is performed under GA. Older children or adults, however, may tolerate the procedure with the use of local anesthesia alone. The frenum is released in a similar manner as in frenotomy although occasionally limited division of the genioglossus may be required for adequate release. The wound is sutured with a z-plasty flap closure.
Figure 3E. The child can fully protrude the tongue past incisors.
Discussion
part of the healing process and not be mistakenly perceived as infection. Antibiotic therapy is not needed. Follow-up in 1 to 2 weeks should show that the incision is completely healed. Clinicians who typically perform frenotomy include otolaryngologists, dentists, and pediatricians. Interestingly, 22% of a group of 425 North American pediatricians who responded to a survey indicated that they had performed frenotomies, although only 10% reported that they have
Pediatric Dentistry 27:1, 2005
Diagnosis and management of ankyloglossia
Kupietzky, Botzer
45
been taught the technique in residency.2 This should encourage dentists not familiar with the procedure to study the technique and incorporate it into their practice. The technique, similar to all surgical procedures may, however, result in several possible complications. Complications of frenotomy include infection, excessive bleeding, recurrent AG due to excessive scarring, new speech disorders developing postoperatively, and glossoptosis (tongue swallowing) due to excessive tongue mobility.4 One incident of a life-threatening complication after lingual frenotomy has been reported in the literature.22 A 7-year-old boy with a tight lingual frenum was placed under GA with a nasal pharyngeal airway and face mask. The frenum was incised and sutured. Immediately after removal of the airway, upper airway obstruction occurred. The patient displayed evidence of upper airway collapse, which resolved spontaneously within an hour. The authors explained that, normally, contraction of the genioglossus muscle pulls the tongue and hyoid bone anteriorlyit being the principal dilator of the upper airway. A tight lingual frenum also holds the tongue anteriorly, and, after surgical release, the genioglossus muscle may not be able to generate sufficient force to prevent airway collapse. It is not this reports intention to instruct readers to begin and perform frenotomies in their daily practice. Rather, it is suggested that clinicians consider performing this procedure for the benefit of their patients after obtaining further training regarding the technique. A clinician seeing an infant is encouraged to: 1. examine the frenum attachment; 2. diagnose AG if it is present and evaluate its severity; 3. be aware of the benefits of frenotomy; 4. refer patients to a qualified surgeon if unable to perform a frenotomy. When this techniques relative simplicity is weighted against the severity of the consequences of untreated cases or the future treatment with the frenectomy procedure, pediatric dentists should consider the frenotomy technique. This report should facilitate early treatment of this relatively common disturbance.
References
1. American Academy of Pediatric Dentistry. Guideline on infant oral health care. Pediatr Dent 2002(7);24:47. 2. Lalakea ML, Messner AH. Ankyloglossia: Does it matter? Pediatr Clin North Am 2003;50;381-397. 3. Ballard JL, Auer CE, Khoury JC. Ankyloglossia: Assessment, incidence, and effect of frenuloplasty on the breast-feeding dyad. Pediatrics 2002;110:e63.
4. Messner AH, Lalakea ML. Ankyloglossia: Controversies in management. Int J Pediatr Otorhinolaryngol 2000;54:123-131. 5. Kotlow LA. Ankyloglossia (tongue-tie): A diagnostic and treatment quandary. Quintessence Int 1999;30:259-262. 6. Wallace AF. Tongue-tie. Lancet 1963;2:377-378. 7. Flinck A, Paludan A, Matsson L, Holm AK Axelsson I. Oral findings in a group of newborn Swedish children. Int J Paediatr Dent 1994;4;67-73. 8. Messner AH, Lalakea ML. Ankyloglossia: Incidence and associated feeding difficulties. Arch Otolaryngol Head Neck Surg 2000;126:36-39. 9. Horton CE, Crawford HH, Adamson JE, Ashbell TS. Tongue-tie. Cleft Palate J 1969;6:8-23. 10. Catlin FL de Haan V. Tongue-tie. Arch Otolaryngol 1971;94:548-557. 11. Warden PJ. Ankyloglossia: A review of the literature. Gen Dent 1991;39:252-253. 12. Friend GW, Harris EF, Mincer HH, et al. Oral anomalies in the neonate, by race and gender, in an urban setting. Pediatr Dent 1990;12:157-161. 13. Jorgenson RJ, Shapiro SD, Salinas CF, Levin S. Intraoral findings and anomalies in neonates. Pediatrics 1982;69:577-581. 14. Williams WN, Waldron CM. Assessment of lingual function when ankyloglossia (tongue-tie) is suspected. J Am Dent Assoc 1985;110:353-326. 15. Marmet C, Shell E, Aldana S, Assessing infant suck dysfunction: Case management. J Hum Lact 2000;16:332-336. 16. Masaitis NS, Kaempf JW. Developing a frenotomy policy at one medical center: A case study approach. J Hum Lact 1996;12:229-232. 17. Wiessinger D, Miller M. Breastfeeding difficulties as a result of tight lingual and labial frena: A case report. J Hum Lact 1995;11:313-316. 18. Fletcher SG. Meldrum JR. Lingual function and relative length of the lingual frenum. J Speech Lang Hear Res 1968;2:382-390. 19. Hazelbaker AK. The assessment tool for lingual frenulum function (ATLFF): Use in a lactation consultant private practice. Thesis. Pasadena, Calif: Pacific Oaks College; 1993. 20. Notestine GE. The importance of identification of ankyloglossia (short lingual frenum ) as a cause of breast-feeding problems. J Hum Lact 1990;6:113-115. 21. Wright JE J. Tongue-tie. Paediatr Child Health 1995;31:276-278. 22. Walsh F, Kelly D. Partial airway obstruction after lingual frenotomy. Anesth Analg 1995;80;1066-1067.
clinical section
46
Kupietzky, Botzer
Diagnosis and management of ankyloglossia
Pediatric Dentistry 27:1, 2005
You might also like
- MKT 6080 Final Project Milestone 2 WorksheetDocument12 pagesMKT 6080 Final Project Milestone 2 WorksheetDEENo ratings yet
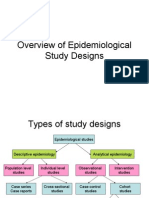
- Overview of Epidemiological Study DesignsDocument16 pagesOverview of Epidemiological Study DesignsLakshmi Seth100% (2)
- Arcon Vs Non Arcon Articulators.: Presented by Dr. Jeewan Bachan Dhinsa 1718703Document18 pagesArcon Vs Non Arcon Articulators.: Presented by Dr. Jeewan Bachan Dhinsa 1718703manasviNo ratings yet
- Wiley - Clinical Cases in Orthodontics - 978-1-118-29247-1Document2 pagesWiley - Clinical Cases in Orthodontics - 978-1-118-29247-1MayerNo ratings yet
- 1975 Jan-Feb #62Document28 pages1975 Jan-Feb #62Merlin ChowkwanyunNo ratings yet
- Leukoplakia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandLeukoplakia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Kim Seol Hee, 2019, The Effects of Orofacial Myofunctional Training On The PDFDocument9 pagesKim Seol Hee, 2019, The Effects of Orofacial Myofunctional Training On The PDFSerina Cahya NabilahNo ratings yet
- Review FrenectomyDocument6 pagesReview FrenectomyNyitnyit KunyitNo ratings yet
- Myofunctional Appliance Treatment: Sleep Dentistry For The 21st CenturyDocument4 pagesMyofunctional Appliance Treatment: Sleep Dentistry For The 21st CenturyNaeem MoollaNo ratings yet
- Periodicity DentalGuideDocument52 pagesPeriodicity DentalGuideSalam BataienehNo ratings yet
- Traumatic Injuries To The Teeth4541Document114 pagesTraumatic Injuries To The Teeth4541Irfan AliNo ratings yet
- Chapter 41.Ppt HypersensitivityDocument63 pagesChapter 41.Ppt HypersensitivityMaria Mercedes LeivaNo ratings yet
- Fluids and Electrolytes 2015Document117 pagesFluids and Electrolytes 2015Rashed ShatnawiNo ratings yet
- Good Morning.: @areebazainabDocument42 pagesGood Morning.: @areebazainabshabana waniNo ratings yet
- Minor Oral Surgical Procedures in Children ClassDocument65 pagesMinor Oral Surgical Procedures in Children ClassReenaChauhanNo ratings yet
- Medical Emergencies in The Dental Office PDFDocument52 pagesMedical Emergencies in The Dental Office PDFsrprior100% (1)
- Management of Class II Div IDocument13 pagesManagement of Class II Div Iapi-19840404No ratings yet
- Tanvi Shah - Maaz ShaikhDocument29 pagesTanvi Shah - Maaz ShaikhTanvi ShahNo ratings yet
- Prosthetic Management of Soft Palate Defects: Presented byDocument57 pagesProsthetic Management of Soft Palate Defects: Presented byPiyush DongreNo ratings yet
- Oral Manifestaions of Systemic DiseasesDocument116 pagesOral Manifestaions of Systemic DiseaseslikhithaNo ratings yet
- Pulp Therapy of Non-Vital Teeth (Pulpectomy)Document27 pagesPulp Therapy of Non-Vital Teeth (Pulpectomy)Mahmoud A. ZoghborNo ratings yet
- A Critical Appraisal of Tongue-Thrusting-Tulley PDFDocument11 pagesA Critical Appraisal of Tongue-Thrusting-Tulley PDFmalifaragNo ratings yet
- Extraoral and Intraoral ExaminationDocument64 pagesExtraoral and Intraoral ExaminationAhmed HotiebaNo ratings yet
- Manual CariogramDocument51 pagesManual CariogramDesty DarmaNo ratings yet
- Thumb Sucking HabbitDocument23 pagesThumb Sucking Habbitmabds312No ratings yet
- Secondary Bone Grafting For Alveolar Clefts SurgicalDocument6 pagesSecondary Bone Grafting For Alveolar Clefts SurgicalRidwan SNo ratings yet
- Periodontal Diseases in Children PedoDocument34 pagesPeriodontal Diseases in Children PedoFourthMolar.comNo ratings yet
- Periodontal Problems in KidsDocument49 pagesPeriodontal Problems in KidsRaksmey PhanNo ratings yet
- Existing Restoration - Clinical Status: Secondary Caries Marginal Integrity Biomechanical FormDocument47 pagesExisting Restoration - Clinical Status: Secondary Caries Marginal Integrity Biomechanical FormDaniel WangNo ratings yet
- Evaluation of The Relationship Between Bruxism and Premature Occlusal ContactsDocument6 pagesEvaluation of The Relationship Between Bruxism and Premature Occlusal ContactsWellyAnggarani100% (1)
- Epidemiologi Dental CariesDocument21 pagesEpidemiologi Dental CariesSampahAjaNo ratings yet
- NSAIDs in DentistryDocument7 pagesNSAIDs in DentistryEliza DNNo ratings yet
- Non-Caries Dental DiseaseDocument61 pagesNon-Caries Dental Diseaseapi-19916399No ratings yet
- DR Nick Lekic - Space MaintainersDocument35 pagesDR Nick Lekic - Space MaintainersanatomimanusiaNo ratings yet
- Administration of Coagulation-Altering Therapy in The Patient Presenting For Oral Health and Maxillofacial SurgeryDocument18 pagesAdministration of Coagulation-Altering Therapy in The Patient Presenting For Oral Health and Maxillofacial SurgeryLaura Giraldo QuinteroNo ratings yet
- Management of Pediatric Medical - Emergencies in The Dental OfficeDocument22 pagesManagement of Pediatric Medical - Emergencies in The Dental Officebanyubiru0% (1)
- Odontogenic Cysts Summary Chart: Radicular Cyst (Periapical Cyst)Document4 pagesOdontogenic Cysts Summary Chart: Radicular Cyst (Periapical Cyst)ML90No ratings yet
- Space Maintenance: Emma Laing, Paul Ashley, Farhad B. Naini & Daljit S. GillDocument8 pagesSpace Maintenance: Emma Laing, Paul Ashley, Farhad B. Naini & Daljit S. GillAnonymous JR1VNCNo ratings yet
- IRTDocument2 pagesIRTIgnacioNo ratings yet
- Tooth Discolour at Ion PedoDocument28 pagesTooth Discolour at Ion PedoFourthMolar.comNo ratings yet
- Crossbite PosteriorDocument11 pagesCrossbite PosteriorrohmatuwidyaNo ratings yet
- SSCDocument50 pagesSSCMustafa Tambawala100% (1)
- Dental Anatomy and PhysiologyDocument36 pagesDental Anatomy and PhysiologyCpt.WnchstrNo ratings yet
- D-Dentin-Lec 1Document45 pagesD-Dentin-Lec 1api-3710331100% (7)
- Association Between Oral Habits, Mouth BreathingDocument9 pagesAssociation Between Oral Habits, Mouth BreathingdewiayuNo ratings yet
- 2 Anatomy of TMJDocument117 pages2 Anatomy of TMJSugandhi Pidaparthi100% (1)
- CementumDocument10 pagesCementumAshish BisaneNo ratings yet
- Endodontics in Systemically Compromised PatientsDocument30 pagesEndodontics in Systemically Compromised Patientscarolina pavezNo ratings yet
- Space ManagementDocument11 pagesSpace Managementdr parveen bathla100% (1)
- Adpied Paper From EmailDocument17 pagesAdpied Paper From Emailapi-401213596No ratings yet
- Pulpectomy PedoDocument30 pagesPulpectomy PedoDr.Harsh100% (1)
- Dry Mouth (Xerostomia)Document18 pagesDry Mouth (Xerostomia)dr_jamal1983No ratings yet
- Impression Making - BDJ - 4800516aDocument9 pagesImpression Making - BDJ - 4800516aDr Anand Rajapur100% (1)
- Reducing The Risk of Failure Incomplete Denture PatientsDocument8 pagesReducing The Risk of Failure Incomplete Denture PatientsHisyam IshakNo ratings yet
- Avulsion: DEFINITION: - Tooth Avulsion (Exarticulation) Implies Total Displacement of The ToothDocument39 pagesAvulsion: DEFINITION: - Tooth Avulsion (Exarticulation) Implies Total Displacement of The Toothshailesh_shenoyNo ratings yet
- Lesions of Oral Soft Tissues in Children PedoDocument74 pagesLesions of Oral Soft Tissues in Children PedoFourthMolar.comNo ratings yet
- 2 Anatomical LandmarksDocument9 pages2 Anatomical LandmarksShady MahmoudNo ratings yet
- Dentin HypersenstivityDocument4 pagesDentin Hypersenstivitymohamed saadNo ratings yet
- 2dev of MaxillaDocument78 pages2dev of MaxillapriyaNo ratings yet
- Animal DentistryDocument10 pagesAnimal DentistryFei Fei LoNo ratings yet
- Access To Special Care Dentistry, Part 9. Special Care Dentistry Services For Older PeopleDocument14 pagesAccess To Special Care Dentistry, Part 9. Special Care Dentistry Services For Older PeoplehaihaitakNo ratings yet
- Revised Application Form PDFDocument1 pageRevised Application Form PDFDilmohit SinghNo ratings yet
- Infant Oral Health 1Document19 pagesInfant Oral Health 1Dilmohit SinghNo ratings yet
- Definition of Early Childhood Caries (ECC) : Originating Council Review Council Adopted RevisedDocument1 pageDefinition of Early Childhood Caries (ECC) : Originating Council Review Council Adopted RevisedDilmohit SinghNo ratings yet
- CGHS Bengaluru Rates List As On NOv.2014Document53 pagesCGHS Bengaluru Rates List As On NOv.2014mamuhydNo ratings yet
- Tooth BleachingDocument24 pagesTooth BleachingDilmohit SinghNo ratings yet
- PEAK Restoration of The Endodontically Treated ToothDocument20 pagesPEAK Restoration of The Endodontically Treated Toothlishenwong100% (1)
- Dentin BondingDocument15 pagesDentin BondingDilmohit SinghNo ratings yet
- 8.review Meenu Mary PaulDocument10 pages8.review Meenu Mary PaulDilmohit SinghNo ratings yet
- Bite SplintsDocument15 pagesBite SplintsAmit Parmar100% (1)
- FINAL SplintingDocument46 pagesFINAL SplintingDilmohit SinghNo ratings yet
- Perio TestDocument9 pagesPerio TestDilmohit SinghNo ratings yet
- Perio TestDocument9 pagesPerio TestDilmohit SinghNo ratings yet
- Reimplantation of Avulsed Primary IncisorsDocument4 pagesReimplantation of Avulsed Primary IncisorsDilmohit SinghNo ratings yet
- 53867257Document7 pages53867257Dilmohit SinghNo ratings yet
- Lingual Frenectomy Using Multiple Series Z-PlastyDocument3 pagesLingual Frenectomy Using Multiple Series Z-PlastyDilmohit SinghNo ratings yet
- A Carbohydrate-Restrictive Strategy Is Safer and As Efficient As Intensive Insulin Therapy in Critically Ill PatientsDocument6 pagesA Carbohydrate-Restrictive Strategy Is Safer and As Efficient As Intensive Insulin Therapy in Critically Ill PatientsTeresaNo ratings yet
- Health Optimizing Physical Education 1Document22 pagesHealth Optimizing Physical Education 1Russel MejicoNo ratings yet
- Department of Education: Action Plan For Wins (Wash in School)Document3 pagesDepartment of Education: Action Plan For Wins (Wash in School)Rosalie Belaguas Rojonan50% (2)
- 2005 PDFDocument436 pages2005 PDFAbdulazizNo ratings yet
- Group Mediclaim Policy Coverages For Employees of Century PlyDocument2 pagesGroup Mediclaim Policy Coverages For Employees of Century PlyUDAYNo ratings yet
- Practical Cardio-Oncology (2019, CRC Press)Document261 pagesPractical Cardio-Oncology (2019, CRC Press)Anitei GabrielaNo ratings yet
- Science 9 Quarter 1 Week 2 Sim 3Document30 pagesScience 9 Quarter 1 Week 2 Sim 3Jelly FloresNo ratings yet
- SpondylolisthesisDocument121 pagesSpondylolisthesisWilliam Surya HartantoNo ratings yet
- Test Bank For 3 2 1 Code It 2020 8th Edition Michelle Green Full DownloadDocument24 pagesTest Bank For 3 2 1 Code It 2020 8th Edition Michelle Green Full Downloadrobertabergmjnxqrasct100% (43)
- Hyperthermia HIV NURSING CARE PLAN FLODocument4 pagesHyperthermia HIV NURSING CARE PLAN FLOMicaela CrisostomoNo ratings yet
- Residency Prog CanadaDocument116 pagesResidency Prog Canadahswami20037730No ratings yet
- ABCDE Assessment Exam: Eunice QuijanoDocument3 pagesABCDE Assessment Exam: Eunice QuijanoQuijano GpokskieNo ratings yet
- Lectura Unidad 8Document16 pagesLectura Unidad 8Day FuNo ratings yet
- Gems and Gems Advanced 2016Document2 pagesGems and Gems Advanced 2016Plate MealsNo ratings yet
- Murshidabad Action Plan10-11Document13 pagesMurshidabad Action Plan10-11Prabir Kumar ChatterjeeNo ratings yet
- Uro-Gynaecology From Cambridge To UAE?Document28 pagesUro-Gynaecology From Cambridge To UAE?Michelle FynesNo ratings yet
- Contraindications To Implant Treatment 1Document1 pageContraindications To Implant Treatment 1Hussien A. Abu OlbaNo ratings yet
- Marshall Islands Medical Certificate B-SideDocument1 pageMarshall Islands Medical Certificate B-Sidedeniss sumilovsNo ratings yet
- Post Term PregnancyDocument22 pagesPost Term PregnancyDarianne HernandezNo ratings yet
- KMPDU Private Practice CBA EldoretDocument57 pagesKMPDU Private Practice CBA Eldoretapi-175531574No ratings yet
- Blood Glucose MonitoringDocument4 pagesBlood Glucose MonitoringAman ChaudharyNo ratings yet
- Mental StatusDocument6 pagesMental StatusIgor Oliveira100% (1)
- Scientific and Ethical Issues in The Use of Placebo Controls in Clinical TrialsDocument20 pagesScientific and Ethical Issues in The Use of Placebo Controls in Clinical TrialsNicusor OnaciuNo ratings yet
- Infection Control Practice On Vital Signs Equipment: A Survey Among Senior Nursing Students in Iloilo City, PhilippinesDocument7 pagesInfection Control Practice On Vital Signs Equipment: A Survey Among Senior Nursing Students in Iloilo City, PhilippinesRyan Michael OducadoNo ratings yet
- Attributable Fractions (As11) : Course: PG Diploma/ MSC EpidemiologyDocument37 pagesAttributable Fractions (As11) : Course: PG Diploma/ MSC EpidemiologyLakshmi SethNo ratings yet
- KUsta PDFDocument29 pagesKUsta PDFTokekKompieNo ratings yet
- Mallory Brearey-Resume 2021 1Document2 pagesMallory Brearey-Resume 2021 1api-507675724No ratings yet