Professional Documents
Culture Documents
Vascularized Lymph Node Transfer Based On The Hilar Perforators Improves The Outcome in Upper Limb Lymphedema
Uploaded by
balab2311Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vascularized Lymph Node Transfer Based On The Hilar Perforators Improves The Outcome in Upper Limb Lymphedema
Uploaded by
balab2311Copyright:
Available Formats
HAND SURGERY
AND
MICROSURGERY
Vascularized Lymph Node Transfer Based on the Hilar Perforators Improves the Outcome in Upper Limb Lymphedema
Bahar Bassiri Gharb, MD, FEBOPRAS,* Antonio Rampazzo, MD, FEBOPRAS,* Stefano Spanio di Spilimbergo, MD,* Enny-Sonia Xu, MS,* Kuo-Piao Chung, PhD, and Hung-Chi Chen, MD, FACS*
The supercial location of lymph nodes, their association with known vessels, and inconspicuous scar following ap harvest have made the inguinal region a favorite donor site for the harvest of vascularized lymph nodes.79 However, this technique has not gained popularity, probably because the numerous variations of the regional vascular anatomy10 have been associated with risk of ap failure. Furthermore, if the selected vascular pedicle does not directly perfuse the lymph nodes their function could be jeopardized. The experience gained from perforator ap surgery, and improved knowledge of vascularization of skin and lymph nodes allowed us to modify the conventional approach to the harvest of inguinal nodes, to improve the outcome and increase the consistency of the results. In 2004, we started to raise a lymph node cutaneous ap from the groin, after direct visualization of the cutaneous and hilar perforators and selection of the dominant pedicle to both components of the ap to ensure the most physiologic blood supply to the lymph nodes. In this study, we discuss the modied technique and compare the results to the outcomes achieved with the conventional approach.
Background: Maintenance of the blood supply to the lymph nodes is necessary for survival and function. We report the outcome of vascularized lymph node transfer with hilar perforators compared with the conventional technique. Patients: A total of 21 patients affected by early stage II upper limb lymphedema were included in this study. Of them, 11 patients received a free groin ap containing lymph nodes and 10 patients received vascularized inguinal lymph nodes with hilar perforators. Mean follow-up was 46 and 40 months, respectively. Complications, secondary procedures, circumference of the limb, and subjective symptomatology were registered. The differences were evaluated statistically. Results: The limb circumferences decreased signicantly in the new group. The number of secondary procedures was signicantly higher in the standard group. There were 2 cases of partial ap loss and donor site lymphorrhea in the standard group. In both the groups, visual analog scale scores improved after the operation. Conclusions: Transfer of vascularized inguinal lymph nodes based on the hilar perforators improves the outcomes in the treatment of early lymphedema of the upper extremity. Key Words: vascularized lymph node, free lymph node transfer, perforator ap, lymphedema, breast cancer (Ann Plast Surg 2011;XX: 000 000)
PATIENTS AND METHODS
Vascularized lymph node transfer has been approved by the internal review board of our hospital for patients affected by early stage II lymphedema of the limbs according to the criteria of the International Society of Lymphology.11 Diagnosis and staging of lymphedema are made on the basis of history, clinical examination, and lymphoscintigraphy with Technetium 99m. All patients presenting with early stage II lymphedema of the upper extremity after mastectomy and axillary dissection are offered vascularized lymph node transfer when the volume of the limb continues to increase after a minimum of 6 consecutive months conservative therapy consisting of limb elevation, compression garments, and decongestive treatment.
pper limb lymphedema affects approximately 30% of women undergoing lymphadenectomy or lymphatic radiation for breast cancer.1 Although a majority of the patients are responsive to conservative measures, in 10% the treatment fails requiring further management before brosis, lipogenesis, and hyperkeratosis make the process irreversible. Normally after injury, the lymph ow is restored fairly quickly because of the robust regenerative capacity of the lymphatic vessels.2 However, when the regenerative potentials have been damaged by scarring and irradiation, transfer of lymph nodes could represent the most physiological method to restore the afferent lymphatic pathways and to deliver the lymph load to deep venous system. Maintenance of the blood supply to the transferred lymph node is necessary for survival and preservation of function,35 as afferent and efferent continuity is reestablished spontaneously following division if the nodal vascular supply is retained.6
Received May 22, 2010, and accepted for publication, after revision, August 15, 2010. From the *Plastic Surgery Department, China Medical University Hospital, Taichung, Taiwan; and Department of Public Health, Institute of Health Care Organization Administration, College of Public Health, National Taiwan University, Taipei, Taiwan. Reprints: Hung-Chi Chen, MD, PhD, FACS, Plastic Surgery Department, China Medical University Hospital, 2, Yuh-Der Road, Taichung, Taiwan. E-mail: D19722@mail.cmuh.org.tw. Copyright 2011 by Lippincott Williams & Wilkins ISSN: 0148-7043/11/0000-0001 DOI: 10.1097/SAP.0b013e3181f88e8a
Operative Procedure Standard Approach
The inguinal ligament is marked between the pubic tubercle and the anterior superior iliac spine. The axis of the ap is drawn 2 cm distal and parallel to inguinal ligament. The rst incision is made laterally, down to the deep fascia. Thereafter, the dissection progresses medially over the muscle fascia. At the level of sartorius, the deep branch of the supercial circumex iliac artery usually pierces the muscle fascia; therefore, the dissection is carried out deep to the fascia. Harvest of the ap proceeds medially until the femoral artery is reached. Lymph nodes present in the medial subcutaneous fat tissue are harvested en bloc with the ap (Figs. 13).
Perforator-Based Approach
The position of the inguinal ligament is marked as discussed earlier in the text. A slightly oblique incision is made through the skin, just lateral to the femoral artery starting below the inguinal www.annalsplasticsurgery.com | 1
Annals of Plastic Surgery Volume XX, Number XX, XXX 2011
Gharb et al
Annals of Plastic Surgery Volume XX, Number XX, XXX 2011
FIGURE 1. Schematic representation of the standard groin flap containing lymph nodes. The flap is harvested from lateral to medial, based on the deep branch of the superficial circumflex iliac artery (Db-SCIA). The lymph nodes are randomly included in the flap and if the superficial branch of the superficial circumflex iliac artery (Sb-SCIA) is not preserved, their physiologic vascularization is jeopardized. FA indicates femoral artery; FV, femoral vein; LN, lymph node; SM, sartorius muscle. Illustration by Antonio Rampazzo.
FIGURE 3. Conventional groin flap containing lymph nodes (deep surface). Sartorius fascia is covering the deep aspect of the flap.
Postoperative Protocol
After surgery, a light medication is applied and the limb is kept mildly elevated. The patients are encouraged to actively move the ngers, although movement of the wrist is restricted by an ulnar-sided wrist splint. For aps inset at the forearm, a splint is not required. Five days postoperatively, and once wound healing is evident, the patient is encouraged to start a passive and active rehabilitation program coordinated by a trained physiotherapist. Discharge is usually possible 7 days after surgery.
Data Collection and Analysis
Circumferential measurements of the affected and normal upper limbs were taken by trained nurses, 10 cm above and below the olecranon, at the wrist, and at the midpalm level before surgery and postoperatively at regular intervals. All of the complications were recorded. Secondary procedures required to improve the result and the number of episodes of cellulitis affecting the upper extremity were registered. Variations of the subjective symptomatology (elasticity of the skin, heaviness of the limb, pain) were assessed with visual analog scale before and at the last follow-up. The preoperative and postoperative upper limb circumferences were expressed as differences with the contralateral (normal side). Differences at the last follow-up were evaluated statistically with the Wilcoxon paired rank test. Preoperative differences between the 2 groups were evaluated in the same manner. Differences in the requirement for secondary procedures between the 2 groups were evaluated with the nonparametric Fisher exact test. Results were considered statistically signicant if P 0.05 and highly signicant if P 0.01.
FIGURE 2. Conventional groin flap containing lymph nodes. The lymph nodes are included en bloc in the flap. ligament. The subsequent dissection is carried out with the aid of the operating microscope and microsurgical instruments. The terminal perforating arterial and venous branches are identied and dissected retrograde down to the source vessels (supercial branch of the supercial circumex iliac artery and vein, supercial inferior epigastric artery and vein, or other axial vessels with unusual course). The skin perforators usually exit between several lymph nodes, which are directly visualized and can be carefully isolated avoiding damage to their vascular hilum. At this stage, the main vascular pedicle is seen and 2 or 3 lymph nodes directly perfused by the main pedicle are selected for transfer (Fig. 4). The inferior margin of the skin ap is incised rst and the course of the pedicle checked from the deep surface. The design of the ap is nalized and the superior incision is performed. When the skin ap is raised, it is possible to complete the dissection of the lymph nodes and the pedicle down to the femoral artery and vein (Figs. 5, 6). The lymph nodes are handled gently and the small afferent lymphatics to the external capsule divided with scissors and not cauterized, to help with the regeneration at the recipient site. 2 | www.annalsplasticsurgery.com
RESULTS
Between September 1997 and April 2008, 25 patients were treated with vascularized inguinal lymph nodes transfer (Tables 1, 2). Perforator-based approach was used in all patients from 2004. Four patients did not have complete records, and therefore were excluded from the study. The number of patients treated with the standard technique and the modied approach was 11 and 10, respectively. Mean age was 54 and 55 years, respectively. Four patients in the standard technique group and 5 patients in the perforator-based group had received radiotherapy after mastectomy 2011 Lippincott Williams & Wilkins
Annals of Plastic Surgery Volume XX, Number XX, XXX 2011
Lymph Node Transfer Based on Hilar Perforators
FIGURE 4. Perforator-based flap. The superficial branch of the superficial circumflex iliac artery is visualized passing between 2 rows of lymph nodes, through the medial incision.
FIGURE 6. Flap based on the hilar perforators. The vascular pedicle passes between the lymph nodes before entering the skin flap. nodes to transfer. The recipient site was the wrist in all patients in the standard technique group, whereas in 2 cases, in the perforatorbased group, the ap was inset at the forearm. Recipient vessels were always radial artery (end-to-side) or its proximal muscle branches (1 case, end-to-end) and the comitant veins of the radial artery (end-to-end). In the standard approach group, there were 2 cases of partial necrosis of the skin paddle treated conservatively. Two patients developed seroma at the donor site. Two patients suffered from multiple episodes of cellulitis affecting the forearm during the follow-up. Eight patients requested further suction-assisted lipectomy to improve the result. In the perforator-based group, there were no immediate complications. One patient suffered 2 episodes of cellulitis at the forearm during the follow-up (36 months). One patient required further debulking of the forearm (radical reduction of lymphedema with preservation of the perforators [RRPP]12) and suction-assisted lipectomy of the arm. One patient required suction-assisted lipectomy of the affected arm. We did not report any case of lower extremity lymphedema and cellulitis following transfer of the ap in either group. None of the patients complained of swelling and heaviness of the donor extremity. In both the groups, patients reported an improvement of the subjective symptomatology following surgery as shown by the preand postoperative visual analog scale scores (standard group, 6.1 vs. 5.3; perforator-based group, 6.3 vs. 5.1). However, these differences were not signicant. There was no statistical difference in the limb circumference measurements between the 2 groups preoperatively. Differences between preoperative and postoperative measurements were statistically signicant only in the perforator-based group at the levels below elbow, wrist, and midpalm (P 0.004, 0.002, 0.007, respectively). All the other differences were not statistically signicant. The difference in the requirement of secondary procedures between the 2 groups was signicant (P 0.03).
FIGURE 5. Schematic representation of the flap based on the hilar perforators. The superficial branch of the superficial circumflex iliac artery (Sb-SCIA) is the dominant vessel responsible for the vascularization of the lymph nodes giving off the hilar perforators and the perforators to the skin. DbSCIA indicates deep branch of the superficial circumflex iliac artery; FA, femoral artery; FV, femoral vein; LN, lymph node; SM, sartorius muscle. Illustration by Antonio Rampazzo.
and axillary dissection. All of the patients evidenced complete obstruction of the lymphatics at the preoperative lymphoscintigraphy. The mean follow-up was 46 months (26 120 months) and 40 months (38 50 months). The feeding artery of the ap was the deep branch of the supercial circumex iliac artery in all patients in the standard group. In the perforator-based group, 7 aps were vascularized by the supercial branch of the supercial circumex iliac artery and 3 aps were nourished by the supercial inferior epigastric artery. In the latter patients, the design of the ap was modied intraoperatively to incorporate the supercial inferior epigastric artery as the axis of the ap. In 2 cases, the supercial branch of the supercial circumex iliac artery did not join the deep branch and reached the femoral artery independently. In the other 5 cases, the supercial and the deep branches of the supercial circumex iliac artery united 1 to 2 cm before reaching the femoral artery. In the perforator-based group, in all cases it was possible to select 2 to 3 lymph 2011 Lippincott Williams & Wilkins
DISCUSSION
Lymph nodes represent physiologic lymphaticovenous anastomosis.13 Because the colloid osmotic pressure of the lymph is lower than that of the blood, protein-free uid is absorbed from www.annalsplasticsurgery.com | 3
Gharb et al
Annals of Plastic Surgery Volume XX, Number XX, XXX 2011
the lymph into the blood capillaries to establish the equilibrium of Starling forces across the lymph-blood barrier. If the vascular supply is not optimal, there is less opportunity for lymph absorption into the vein and the tissue itself atrophies,2 losing the ability to spontaneously reestablish afferent and efferent continuity following division.6,14,15 Therefore, restoration of lymphatic function following lymph node transfer requires establishment of adequate perfusion.3,4,16 Clinical experience with transfer of vascularized lymph nodes has been mostly limited to the inguinal region because of reduced morbidity associated with the harvest of the supercial lymph nodes and inconspicuous donor scar. Conventionally, the aps with or without a skin component were based on the deep branch of the supercial circumex iliac artery and dissected as a traditional groin ap is harvested.79 However, the deep branch of the supercial circumex iliac artery plays only a marginal role in the perfusion of the inguinal nodes giving off mainly branches to the muscles in the femoral triangle17 and vascularizes the skin lateral to the anterior superior iliac spine. As already described by Acland18 and subsequently stressed out by Cormack and Lamberty,17 the supercial branch of the supercial circumex iliac artery is the main supply of the lymph nodes. If the origin of the supercial branch from the main trunk is severed, the lymph nodes will lose their physiologic blood supply in most of the cases and their function will be hampered. Other 2 cutaneous arteries, the supercial inferior epigastric artery or the ascending branch of the supercial external pudendal artery can occasionally represent the dominant pedicle, running through the lymph nodes and supplying the hilar perforators, when the supercial circumex iliac artery is absent. Given the variability of the vascular anatomy of the groin, the success of the operation can be ensured only when the dominant artery, simultaneously responsible for perfusion of the lymph nodes and the skin, is chosen as the pedicle of the ap. The rst clinical application of vascularized inguinal lymph nodes was reported by Clodius et al.7 Transfer of a pedicled groin ap from the contralateral side achieved stable reduction in the circumference of the lymphedematous limb. However, the second patient who received a free groin ap experienced rapid recurrence of lymphedema. Becker et al8 published a series of 24 patients with long-term outcome following microsurgical inguinal lymph node transplantation to the axilla. The ap consisted of lymph nodes and subcutaneous fat vascularized by supercial circumex iliac artery and vein. They sustained that the upper limb perimeter returned to normal in 10 patients (42%) and decreased in 12 patients (50%). Twenty-nine percent of the patients7 required a secondary transfer because of the incomplete result following the rst operation. Lymphorrhea compared in 33% of the patients and 29% suffered 1 episode of cellulitis. Lin et al9 reported the transfer of vascularized groin lymph nodes using the wrist as a recipient site. A groin ap based on the supercial circumex iliac vessels was performed in 13 patients. The hand circumferences decreased signicantly in 12 patients. Two patients required further debulking procedures. The incidence of cellulitis was decreased in 11 patients. In the recent years, the concept of perforator aps and attainment of rened skills necessary to dissect ne perforators has gradually modied our approach to the harvest of inguinal lymph nodes. Exploration of the vascular anatomy is performed through retrograde dissection of the small perforators to the skin down to the source vessel, with direct visualization of the lymph nodes, their distribution, and localization of the hilar perforators. This approach allowed us to harvest safely the skin island and lymph nodes on the same vascular pedicle in 10 patients. We compared the results of the perforator-based approach with the standard technique. The pa 2011 Lippincott Williams & Wilkins
Forearm cellulites, inguinal seroma Partial ap necrosis, inguinal seroma
Complications
Follow-up (mo)
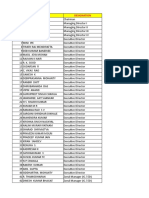
26 60 60 120 26 24 60 36 30 29 38 1 2 3 4 5 6 7 8 9 10 11 69 51 48 69 46 46 49 79 46 51 45 Right Left Left Right Right Left Left Right Left Right Left No No No No No Yes No Yes Yes Yes No Db-SCIA Db-SCIA Db-SCIA Db-SCIA Db-SCIA Db-SCIA Db-SCIA Db-SCIA Db-SCIA Db-SCIA Db-SCIA Wrist Wrist Wrist Wrist Wrist Wrist Wrist Wrist Wrist Wrist Wrist SAL arm and forearm SAL arm SAL forearm SAL forearm SAL forearm arm SAL arm SAL forearm arm SAL arm 7/26/2/3.5 7/4/0/0.5 9/7/11/5 8/6/1.5/0 3.5/5.5/2/2 4.5/5.8/2/0 1/4/2/2 8/5/1.5/0 3.5/6/3.5/0.5 3.5/4.5/2/1 2/4/12/15 8/15/8/3.5 3/1/0/0 3/0/2/0 11/8/1/0 0/4/1.5/1 1.5/4.5/4/0 3/1.5/2.5/3 13/7/1/0.5 1.5/2.5/4/0 5/6/2/1 3/4/13/14
Partial ap necrosis
AE indicates above elbow; BE, below elbow; W, wrist; P, midpalm; Db-SCIA, deep branch of the supercial circumex iliac artery; SAL, suction-assisted lipectomy.
TABLE 1. Patients Data: Standard Groin Flap Containing Lymph Nodes
4 | www.annalsplasticsurgery.com
Patient Number
Age
Upper Extremity
Radiotherapy
Feeding Artery
Recipient Site
Other Procedures
Preoperative AE, BE, W, P
Last Follow-up AE, BE, W, P
Forearm cellulites
Annals of Plastic Surgery Volume XX, Number XX, XXX 2011
Lymph Node Transfer Based on Hilar Perforators
TABLE 2. Patients Data: Flap Based on the Hilar Perforators
Patient Upper Feeding Recipient Number Age Extremity Radiotherapy Artery Site 1 2 3 4 5 6 7 8 9 10 76 48 47 63 47 22 75 53 69 56 Right Left Left Right Left Left Left Right Right Left No No No Yes No No Yes Yes Yes Yes SIEA Sb-SCIA SIEA Sb-SCIA Sb-SCIA Sb-SCIA SIEA Sb-SCIA Sb-SCIA Sb-SCIA Other Procedures Preoperative Last Follow-up Follow-up AE, BE, W, P AE, BE, W, P (mo) 4/2.5/2/1.5 4.5/8/2/2 4/6/3/1 4/2.5/2/1 4/6/3/1 2/2/0/0.5 1/1/1/1 0.5/0/1/0 0/5/1.5/0 1/0/1/0.5 38 23 40 43 50 35 44 45 39 40 Complications
Wrist 2/8.5/8/4.5 Wrist 7/11.5/3.5/1.5 Wrist Skin reduction/SAL arm 8.5/7.5/4/3 Wrist 2/7/8/4.5 Wrist SAL forearm 10/8/5/3 Wrist 4/3/1/1 Wrist 1/2/1.5/2 Forearm 4/1.5/4/1 Forearm 1/7/3/0 Wrist 1/0/2/1.5
Forearm cellulites
AE indicates above elbow; BE, below elbow; W, wrist; P, mid-palm; Sb-SCIA, supercial branch of the supercial circumex iliac artery; SIEA, supercial inferior epigastric artery; SAL, suction-assisted lipectomy.
tient population in the 2 groups was homogeneous, and there were no signicant differences in upper limb circumferences preoperatively. Postoperatively, the circumferences decreased signicantly only in the perforator-based group. Although patients in both the groups reported improvement of the subjective symptomatology, the patients in standard approach group required signicantly more debulking procedures. There were no statistical differences in the complication rate between the 2 groups but only 2 cases of partial ap necrosis and inguinal seroma occurred in the standard approach group. In conclusion, the perforator-based approach showed to be a versatile method, which allows modication of the preoperative plan on the basis of the intraoperative ndings, direct selection of the main vascular pedicle, and the number of transferred lymph nodes. All these factors contribute to improve the outcomes of vascularized lymph node transfer in the treatment of early upper limb lymphedema, as the physiological blood supply to lymph nodes is preserved. The possibility to select the dominant vascular pedicle and the number of transferred lymph nodes is helpful in increasing the predictability of the results and reducing the donor site morbidity. REFERENCES
1. Williams AF, Franks PJ, Moffatt CJ. Lymphoedema: estimating the size of the problem. Palliat Med. 2005;19:300 313. 2. Jila A, Kim H, Nguyen VP, et al. Lymphangiogenesis following obstruction of large postnodal lymphatics in sheep. Microvasc Res. 2007;73:214 223. 3. Shesol BF, Nakashima R, Alavi A, et al. Successful lymph node transplantation in rats, with restoration of lymphatic function. Plast Reconstr Surg. 1979;63:817 823. 4. Chen HC, OBrien BM, Rogers IW, et al. Lymph node transfer for the treatment of obstructive lymphoedema in the canine model. Br J Plast Surg. 1990;43:578 586. 5. Tobbia D, Semple J, Baker A, et al. Experimental assessment of autologous
6. 7. 8.
9.
10. 11.
12.
13. 14.
15.
16.
17. 18.
lymph node transplantation as treatment of postsurgical lymphedema. Plast Reconstr Surg. 2009;124:777786. Tilak SP, Howard JM. Regeneration and autotransplantation of lymph nodes. Ann Surg. 1965;161:441 446. Clodius L, Smith PJ, Bruna J, et al. The lymphatics of the groin ap. Ann Plast Surg. 1982;9:447 458. Becker C, Assouad J, Riquet M, et al. Postmastectomy lymphedema: longterm results following microsurgical lymph node transplantation. Ann Surg. 2006;243:313315. Lin CH, Ali R, Chen SC, et al. Vascularized groin lymph node transfer using the wrist as a recipient site for management of postmastectomy upper extremity lymphedema. Plast Reconstr Surg. 2009;123:12651275. Cooper TM, Lewis N, Baldwin MA. Free groin ap revisited. Plast Reconstr Surg. 1999;103:918 924. International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema. 2009 Consensus Document of the International Society of Lymphology. Lymphology. 2009;42:51 60. Salgado CJ, Sassu P, Gharb BB, et al. Radical reduction of upper extremity lymphedema with preservation of perforators. Ann Plast Surg. 2009;63:302 306. Becker C, Hidden G. Transfer of free lymphatic aps. Microsurgery and anatomical study. J Mal Vasc. 1988;13:119 122. Rothkotter HJ, Pabst R. Autotransplantation of lymph node fragments. Structure and function of regenerated tissue. Scand J Plast Reconstr Surg Hand Surg. 1990;24:101105. Blum KS, Hadamitzky C, Gratz KF, et al. Effects of autotransplanted lymph node fragments on the lymphatic system in the pig model. Breast Cancer Res Treat. 2010;120:59 66. Tobbia D, Semple J, Baker A, et al. Lymphedema development and lymphatic function following lymph node excision in sheep. J Vasc Res. 2009;46:426 434. Cormack GC, Lamberty BG. The Arterial Anatomy of Skin Flaps. 2nd ed. London, United Kingdom: Churchill Livingston; 1994. Acland RD. The free iliac ap: a lateral modication of the free groin ap. Plast Reconstr Surg. 1979;64:30 36.
2011 Lippincott Williams & Wilkins
www.annalsplasticsurgery.com | 5
You might also like
- Analyzing Sri Lankan Ceramic IndustryDocument18 pagesAnalyzing Sri Lankan Ceramic Industryrasithapradeep50% (4)
- 173089Document22 pages173089aiabbasi9615100% (1)
- PPM Informed Consent in Anesthesia WITH FORMSDocument10 pagesPPM Informed Consent in Anesthesia WITH FORMSbalab2311No ratings yet
- Anesthesia Consent FormDocument2 pagesAnesthesia Consent Formbalab2311No ratings yet
- Brushbond TI Flexicoat PDFDocument3 pagesBrushbond TI Flexicoat PDFbalab2311No ratings yet
- Arvind Textiles Internship ReportDocument107 pagesArvind Textiles Internship ReportDipan SahooNo ratings yet
- Yamamoto 2018Document9 pagesYamamoto 2018cocooakNo ratings yet
- Original Article: Laparoscopic Inguinal Lymphadenectomy: A New Minimally Invasive Technique To Treat Vulva CarcinomaDocument6 pagesOriginal Article: Laparoscopic Inguinal Lymphadenectomy: A New Minimally Invasive Technique To Treat Vulva CarcinomaVlad GrigoreNo ratings yet
- Management of Anal FistulaDocument5 pagesManagement of Anal Fistulailham adhaniNo ratings yet
- Huge Extradural Multilevel Lumbar Abscess. Case ReportDocument11 pagesHuge Extradural Multilevel Lumbar Abscess. Case ReportNervul VagNo ratings yet
- Fascia Wrapping Technique A Modified Method For The Treatment of Cubital Tunnel SyndromeDocument7 pagesFascia Wrapping Technique A Modified Method For The Treatment of Cubital Tunnel SyndromeJuanHoyosNo ratings yet
- Pelvic Lymphadenectomy Step-By-Step Surgical EducaDocument5 pagesPelvic Lymphadenectomy Step-By-Step Surgical EducaVlad GrigoreNo ratings yet
- VaricocelectomyDocument10 pagesVaricocelectomyRj TanNo ratings yet
- Main Principles of Varicose Disease Surgical Treatment A. Conservative TherapyDocument3 pagesMain Principles of Varicose Disease Surgical Treatment A. Conservative TherapyManushi HenadeeraNo ratings yet
- Review Article: Intersphincteric Resection and Coloanal Anastomosis in Treatment of Distal Rectal CancerDocument10 pagesReview Article: Intersphincteric Resection and Coloanal Anastomosis in Treatment of Distal Rectal CancerJaysonGarabilesEspejoNo ratings yet
- Ciencia e Technica Omentum Overlay PDFDocument10 pagesCiencia e Technica Omentum Overlay PDFAlin MihetiuNo ratings yet
- Williams2013 Article LaparoscopicManagementOfHighTrDocument3 pagesWilliams2013 Article LaparoscopicManagementOfHighTrVishnu priya kokkulaNo ratings yet
- Surgical Management of Rectal Carcinoma - MILES PROCDocument5 pagesSurgical Management of Rectal Carcinoma - MILES PROCdptkomangNo ratings yet
- Types of Abdominal IncisionsDocument3 pagesTypes of Abdominal Incisionsjhuzt4_facebook_343onlyNo ratings yet
- 2014 172 0 Retroperitoneal and Retrograde Total Laparoscopic Hysterectomy As A Standard Treatment in A Community Hospital 97 101 1Document5 pages2014 172 0 Retroperitoneal and Retrograde Total Laparoscopic Hysterectomy As A Standard Treatment in A Community Hospital 97 101 1Sarah MuharomahNo ratings yet
- LaparoscopeDocument9 pagesLaparoscopedharmaNo ratings yet
- Oesophagocoloplasty For Corrosive Oesophageal Stricture: AbstractDocument12 pagesOesophagocoloplasty For Corrosive Oesophageal Stricture: AbstractSpandan KadamNo ratings yet
- NAIS Initial PaperDocument10 pagesNAIS Initial Paperjesus Porras ColonNo ratings yet
- 4 PDFDocument3 pages4 PDFSamiaNazNo ratings yet
- Current Trends in Extended Lymph Node Dissection For Esophageal CarcinomaDocument6 pagesCurrent Trends in Extended Lymph Node Dissection For Esophageal CarcinomaYacine Tarik AizelNo ratings yet
- Mastectomy/ Modified Radical Mastectomy: IndicationsDocument6 pagesMastectomy/ Modified Radical Mastectomy: IndicationsNANDAN RAINo ratings yet
- Wjols 2010 03 091Document7 pagesWjols 2010 03 091TJ LapuzNo ratings yet
- Articulo 1 Quiste ColeDocument4 pagesArticulo 1 Quiste ColeMaria Elena VinuezaNo ratings yet
- Arthroscopic Suture Bridge Transosseus Equivalent Fixation of RC TendonDocument8 pagesArthroscopic Suture Bridge Transosseus Equivalent Fixation of RC TendonIlias GalanopoulosNo ratings yet
- Nephrectomy ProcedureDocument4 pagesNephrectomy ProcedureRon Java FantillanNo ratings yet
- Https:grupologsa - Eu:wp-Content:uploads:2023:01:01 AA 2016 4 ZubilewiczDocument6 pagesHttps:grupologsa - Eu:wp-Content:uploads:2023:01:01 AA 2016 4 Zubilewiczbraulio HuarachaNo ratings yet
- Lymphedema Rates in Pedicled ALTP For Coverage in Irradiated Groin Defects 2019Document4 pagesLymphedema Rates in Pedicled ALTP For Coverage in Irradiated Groin Defects 2019yeapdshengNo ratings yet
- Ma 07004Document5 pagesMa 07004Lilik PrasajaNo ratings yet
- Abdominoperineal Resection MilesDocument17 pagesAbdominoperineal Resection MilesHugoNo ratings yet
- Jurnal Windi 2Document6 pagesJurnal Windi 2Fiella Ardhilia NuchnumNo ratings yet
- Laparoscopic Surgery in Gynaecologic OncologyDocument7 pagesLaparoscopic Surgery in Gynaecologic OncologyManan BoobNo ratings yet
- The Bilateral Pedicled Epilated Scrotal Flap: A Powerful Adjunctive For Creation of More Neovaginal Depth in Penile Inversion VaginoplastyDocument8 pagesThe Bilateral Pedicled Epilated Scrotal Flap: A Powerful Adjunctive For Creation of More Neovaginal Depth in Penile Inversion VaginoplastySexologia Del OesteNo ratings yet
- Img 0072Document1 pageImg 0072O'jays NavarroNo ratings yet
- Ahn 2011Document4 pagesAhn 2011Residentes PediatríaNo ratings yet
- Superiorly Based Perforator Plus FL Ap For Inguinal Defects: Original ArticleDocument5 pagesSuperiorly Based Perforator Plus FL Ap For Inguinal Defects: Original ArticleamdreyNo ratings yet
- Sotelo Et Al, Laparoscopic Rectovesical Fistula RepairDocument5 pagesSotelo Et Al, Laparoscopic Rectovesical Fistula RepairjordynixnNo ratings yet
- Original ArticleDocument9 pagesOriginal ArticleJason HuangNo ratings yet
- Final Hernioplasty Compilation RevisedDocument58 pagesFinal Hernioplasty Compilation RevisedRaidis PangilinanNo ratings yet
- Ruurda Et Al-2015-Journal of Surgical OncologyDocument9 pagesRuurda Et Al-2015-Journal of Surgical OncologyJohnny TeoNo ratings yet
- Secondary Extra-Anatomic InfrainguinalDocument5 pagesSecondary Extra-Anatomic InfrainguinalAlexandre MaedaNo ratings yet
- International Journal of Surgery Case ReportsDocument3 pagesInternational Journal of Surgery Case Reportshussein_faourNo ratings yet
- Gibson Et Al-2012-Transforaminal Endoscopic Spinal SurgeryDocument7 pagesGibson Et Al-2012-Transforaminal Endoscopic Spinal SurgeryjuanguapoNo ratings yet
- Femoral HerniaDocument4 pagesFemoral HerniaKatie AndersonNo ratings yet
- Robotic-Assisted Laparoscopic Radical Cystectomy With Extracorporeal Urinary Diversion: Initial ExperienceDocument11 pagesRobotic-Assisted Laparoscopic Radical Cystectomy With Extracorporeal Urinary Diversion: Initial ExperiencesandyrraoNo ratings yet
- Laparoscopic Umbilical Hernia Repair Technique PapDocument6 pagesLaparoscopic Umbilical Hernia Repair Technique PapEremeev SpiridonNo ratings yet
- Omentum OverlayDocument10 pagesOmentum OverlayAlin MihetiuNo ratings yet
- Repair of Neglected Achilles Tendon Ruptures JFAS 1994Document8 pagesRepair of Neglected Achilles Tendon Ruptures JFAS 1994Evan BowlesNo ratings yet
- Pelvic and Paraaortic Lymphadenectomy in Gynecologic Cancers - UpToDateDocument31 pagesPelvic and Paraaortic Lymphadenectomy in Gynecologic Cancers - UpToDateAMGY82100% (1)
- Chapter 5 - VenipunctureDocument14 pagesChapter 5 - VenipunctureHrvojeNo ratings yet
- The Spleen: Splenic Trauma and Splenectomy: TrunkDocument3 pagesThe Spleen: Splenic Trauma and Splenectomy: TrunkAsish GeiorgeNo ratings yet
- Et0420 MedAffairs MouawadDocument5 pagesEt0420 MedAffairs MouawadAna Silvia LebrOnNo ratings yet
- 1 s2.0 S0002961017313703 MainDocument4 pages1 s2.0 S0002961017313703 MainFlorin AchimNo ratings yet
- Incision Access UrologyDocument47 pagesIncision Access UrologyHafizur RashidNo ratings yet
- A Simple Method For Lower Extremity Phlebography-Pseudo-Obstruction of The Popliteal Vein!Document4 pagesA Simple Method For Lower Extremity Phlebography-Pseudo-Obstruction of The Popliteal Vein!Diva PrayogaNo ratings yet
- RectopexyDocument7 pagesRectopexyInzamam Ul HaqNo ratings yet
- Lap NephrectomyDocument13 pagesLap NephrectomynadalNo ratings yet
- реконструкция нижней челюстиDocument8 pagesреконструкция нижней челюстиIrinaBorodulinaNo ratings yet
- The Effect of Spinal Anaesthesia On Penile TumescenceDocument5 pagesThe Effect of Spinal Anaesthesia On Penile TumescenceMaria MiripNo ratings yet
- Surgical Endoscopy Aug1998Document99 pagesSurgical Endoscopy Aug1998Saibo BoldsaikhanNo ratings yet
- Baldwin - 2010 - Veterinary Clinics of North America Equine PracticeDocument6 pagesBaldwin - 2010 - Veterinary Clinics of North America Equine PracticeTania Garcia MollNo ratings yet
- Building Blocks Issue 7 26 1Document10 pagesBuilding Blocks Issue 7 26 1balab2311No ratings yet
- Craniosynostosis & Craniofacial Surgery: A Parent's GuideDocument16 pagesCraniosynostosis & Craniofacial Surgery: A Parent's Guidebalab2311No ratings yet
- Azhaar TopicDocument4 pagesAzhaar Topicbalab2311No ratings yet
- IndianJAnaesth542116-1332734 034207Document5 pagesIndianJAnaesth542116-1332734 034207balab2311No ratings yet
- Midfacial Reconstruction Using Calvarial Split Bone GraftsDocument6 pagesMidfacial Reconstruction Using Calvarial Split Bone Graftsbalab2311No ratings yet
- 26 3 MovahedDocument4 pages26 3 Movahedbalab2311No ratings yet
- Onlay Bone Graft Augmentation For Refined Correction of Coronal SynostosisDocument9 pagesOnlay Bone Graft Augmentation For Refined Correction of Coronal Synostosisbalab2311No ratings yet
- Crackers Price ListDocument4 pagesCrackers Price Listbalab2311No ratings yet
- Particularities in The Surgical Technique of Calvaria GraftDocument6 pagesParticularities in The Surgical Technique of Calvaria Graftbalab2311No ratings yet
- Super StuccoDocument2 pagesSuper Stuccobalab2311No ratings yet
- CT Scanning Techniques and ApplicationsDocument358 pagesCT Scanning Techniques and Applicationsbalab2311No ratings yet
- Software Test ISO StandardsDocument2 pagesSoftware Test ISO StandardsTony DavisNo ratings yet
- Gorlov Wind TurbineDocument3 pagesGorlov Wind TurbineDwayneNo ratings yet
- 20779A ENU CompanionDocument86 pages20779A ENU Companionmiamikk204No ratings yet
- Front Pages1Document5 pagesFront Pages1Anonymous g7uPednINo ratings yet
- General Director AdDocument1 pageGeneral Director Adapi-690640369No ratings yet
- ACCOUNTS Foundation Paper1Document336 pagesACCOUNTS Foundation Paper1mukni613324100% (1)
- Editing For BeginnersDocument43 pagesEditing For BeginnersFriktNo ratings yet
- AP Physics Name: AP Thermal PracticeDocument2 pagesAP Physics Name: AP Thermal PracticeMuddamsetty ArunkalyanNo ratings yet
- Application For Leave - EODocument1 pageApplication For Leave - EOcomelec carmenNo ratings yet
- Comparison of BD 37 01 and AASHTO LRFD 2Document59 pagesComparison of BD 37 01 and AASHTO LRFD 2Jan Gerona ApostaderoNo ratings yet
- 101 Union of Filipro Employees Vs Vivar (Labor)Document1 page101 Union of Filipro Employees Vs Vivar (Labor)Kayelyn Lat100% (1)
- ACC 101 - 3rd QuizDocument3 pagesACC 101 - 3rd QuizAdyangNo ratings yet
- PDS Air CompressorDocument1 pagePDS Air Compressordhavalesh1No ratings yet
- Packing Shipping InstructionsDocument2 pagesPacking Shipping InstructionsJ.V. Siritt ChangNo ratings yet
- Group 7 - Mountain DewDocument18 pagesGroup 7 - Mountain DewRishabh Anand100% (1)
- M/B Schematic Version Change List: Release Date PCB P/N Note Pcba P/N PCB DescriptionDocument36 pagesM/B Schematic Version Change List: Release Date PCB P/N Note Pcba P/N PCB DescriptionAdriano Neoaver Tavares100% (2)
- Arab Open University B326: Advanced Financial Accounting TMA - Spring 2022-2023 V2Document7 pagesArab Open University B326: Advanced Financial Accounting TMA - Spring 2022-2023 V2samiaNo ratings yet
- Study On Color Fastness To Rubbing by Crock MeterDocument4 pagesStudy On Color Fastness To Rubbing by Crock Metertushar100% (5)
- AMM Company ProfileDocument12 pagesAMM Company ProfileValery PrihartonoNo ratings yet
- Katalog Bonnier BooksDocument45 pagesKatalog Bonnier BooksghitahirataNo ratings yet
- Standard C4C End User GuideDocument259 pagesStandard C4C End User GuideKanali PaariNo ratings yet
- Siemens Power Engineering Guide 7E 223Document1 pageSiemens Power Engineering Guide 7E 223mydearteacherNo ratings yet
- Parts Price ListDocument5,325 pagesParts Price ListAlva100% (1)
- History of BRAC BankDocument7 pagesHistory of BRAC Bankrayhan555No ratings yet
- Salary Data 18092018Document5,124 pagesSalary Data 18092018pjrkrishna100% (1)
- Enhancing LAN Using CryptographyDocument2 pagesEnhancing LAN Using CryptographyMonim Moni100% (1)
- Module 8 - Simple Interest and Compound InterestDocument11 pagesModule 8 - Simple Interest and Compound InterestDawn Juliana AranNo ratings yet